Abstract
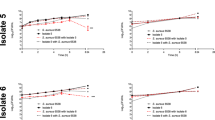
Polymicrobial lung infections in individuals with Cystic Fibrosis (CF) contribute to the complexity of this disease and are a major cause of morbidity and mortality in the CF community. The microorganisms most commonly associated with severe airway infections in individuals with CF are the opportunistic pathogens S. aureus, P. aeruginosa and bacteria from the Burkholderia cepacia complex (Bcc), particularly B. cenocepacia and B. multivorans. Three Bcc strains, two S. aureus wild-type strains, and two derivative mutants were used to investigate the interplay between S. aureus and Bcc with a focus on the hemolytic activity of Bcc. Our results revealed that extracellular products from S. aureus potentiated the hemolysis of Bcc strains. Moreover, this effect was influenced by the composition of the medium in which S. aureus is grown. These findings contribute towards the understanding of the impact of interactions between S. aureus and Bcc and their possible implications in the context of co-infections by these pathogens in individuals with CF.




Similar content being viewed by others
References
Surette MG (2014) The cystic fibrosis lung microbiome. Ann Am Thorac Soc 11(Suppl 1):S61-65. https://doi.org/10.1513/AnnalsATS.201306-159MG
Granchelli AM, Adler FR, Keogh RH, Kartsonaki C, Cox DR, Liou TG (2018) Microbial interactions in the cystic fibrosis airway. J Clin Microbiol. https://doi.org/10.1128/JCM.00354-18
Lyczak JB, Cannon CL, Pier GB (2002) Lung infections associated with cystic fibrosis. Clin Microbiol Rev 15(2):194–222
Chmiel JF, Aksamit TR, Chotirmall SH, Dasenbrook EC, Elborn JS, LiPuma JJ, Ranganathan SC, Waters VJ, Ratjen FA (2014) Antibiotic management of lung infections in cystic fibrosis. I. The microbiome, methicillin-resistant Staphylococcus aureus, Gram-negative bacteria, and multiple infections. Ann Am Thorac Soc 11(7):1120–1129. https://doi.org/10.1513/AnnalsATS.201402-050AS
Vanderhelst E, De Meirleir L, Verbanck S, Pierard D, Vincken W, Malfroot A (2012) Prevalence and impact on FEV(1) decline of chronic methicillin-resistant Staphylococcus aureus (MRSA) colonization in patients with cystic fibrosis. A single-center, case control study of 165 patients. J Cyst Fibros 11(1):2–7. https://doi.org/10.1016/j.jcf.2011.08.006
Dasenbrook EC, Checkley W, Merlo CA, Konstan MW, Lechtzin N, Boyle MP (2010) Association between respiratory tract methicillin-resistant Staphylococcus aureus and survival in cystic fibrosis. JAMA 303(23):2386–2392. https://doi.org/10.1001/jama.2010.791
Govan JR, Brown AR, Jones AM (2007) Evolving epidemiology of Pseudomonas aeruginosa and the Burkholderia cepacia complex in cystic fibrosis lung infection. Future Microbiol 2(2):153–164. https://doi.org/10.2217/17460913.2.2.153
Zemanick ET, Hoffman LR (2016) Cystic fibrosis: microbiology and host response. Pediatr Clin N Am 63(4):617–636. https://doi.org/10.1016/j.pcl.2016.04.003
Hotterbeekx A, Kumar-Singh S, Goossens H, Malhotra-Kumar S (2017) In vivo and In vitro Interactions between Pseudomonas aeruginosa and Staphylococcus spp. Front Cell Infect Microbiol 7:106. https://doi.org/10.3389/fcimb.2017.00106
Cohen TS, Hilliard JJ, Jones-Nelson O, Keller AE, O’Day T, Tkaczyk C, DiGiandomenico A, Hamilton M, Pelletier M, Wang Q, Diep BA, Le VT, Cheng L, Suzich J, Stover CK, Sellman BR (2016) Staphylococcus aureus alpha toxin potentiates opportunistic bacterial lung infections. Sci Transl Med. https://doi.org/10.1126/scitranslmed.aad9922
Ji Y, Bolhuis A, Watson ML (2019) Staphylococcus aureus products subvert the Burkholderia cenocepacia-induced inflammatory response in airway epithelial cells. J Med Microbiol 68(12):1813–1822. https://doi.org/10.1099/jmm.0.001100
Hutchison ML, Poxton IR, Govan JR (1998) Burkholderia cepacia produces a hemolysin that is capable of inducing apoptosis and degranulation of mammalian phagocytes. Infect Immun 66(5):2033–2039
Thomson EL, Dennis JJ (2012) A Burkholderia cepacia complex non-ribosomal peptide-synthesized toxin is hemolytic and required for full virulence. Virulence 3(3):286–298. https://doi.org/10.4161/viru.19355
Limoli DH, Whitfield GB, Kitao T, Ivey ML, Davis MR Jr, Grahl N, Hogan DA, Rahme LG, Howell PL, O’Toole GA, Goldberg JB (2017) Pseudomonas aeruginosa alginate overproduction promotes coexistence with Staphylococcus aureus in a model of cystic fibrosis respiratory infection. MBio. https://doi.org/10.1128/mBio.00186-17
Vu B, Chen M, Crawford RJ, Ivanova EP (2009) Bacterial extracellular polysaccharides involved in biofilm formation. Molecules 14(7):2535–2554. https://doi.org/10.3390/molecules14072535
Bhakdi S, Tranum-Jensen J (1991) Alpha-toxin of Staphylococcus aureus. Microbiol Rev 55(4):733–751
Hildebrand A, Pohl M, Bhakdi S (1991) Staphylococcus aureus alpha-toxin. Dual mechanism of binding to target cells. J Biol Chem 266(26):17195–17200
Otto M (2014) Staphylococcus aureus toxins. Curr Opin Microbiol 17:32–37. https://doi.org/10.1016/j.mib.2013.11.004
Tam K, Torres VJ (2019) Staphylococcus aureus secreted toxins and extracellular enzymes. Microbiol Spectr. https://doi.org/10.1128/microbiolspec.GPP3-0039-2018
Acknowledgements
We want to thank Lorena Tuchscherr de Hauschopp for the mutant LS1 Δagr and Jovanka Voyich de Montana for the USA300 Δhla mutant.
Funding
Research reported in this publication was in part supported by the 2019–20 Junior/Senior Intramural Grant 0357019 to M.S.R. and the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (NIH) to M.S.R under Award Numbers SC3GM125556 and to R.A.B. under Award Numbers R01AI100560, R01AI063517, and R01AI072219. This study was also supported in part by funds and/or facilities provided by the Cleveland Department of Veterans Affairs, Award Numbers 1I01BX002872 to K.M.P.-W. and 1I01BX001974 to R.A.B. from the Biomedical Laboratory Research & Development Service of the VA Office of Research and Development, and the Geriatric Research Education and Clinical Center VISN 10. Cystic Fibrosis Foundation #691309 also support the laboratory of KMP-W. D.O.S is a member of the National Research Council of Argentina (CONICET). S.M is recipient of a postdoctoral fellowship from CONICET. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, the Department of Veterans Affairs or the United States Government.
Author information
Authors and Affiliations
Contributions
1) Conception and design of the study: AM, DS, JD, MSR; 2) Acquisition and analysis of data: AM, DS, AH, SM, JD, MSR; 3) Drafting and revision of manuscript: AM, DS, SM, JD, RB, KPW, MSR.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Moriano, A., Serra, D.O., Hoard, A. et al. Staphylococcus aureus Potentiates the Hemolytic Activity of Burkholderia cepacia Complex (Bcc) Bacteria. Curr Microbiol 78, 1864–1870 (2021). https://doi.org/10.1007/s00284-021-02458-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-021-02458-0