Abstract
Purpose
Anticancer-drug efficacy seems to involve the direct interaction with host immune cells. Although topoisomerase I (Top I) inhibitors have been suggested to block LPS-evoked inflammation, the interaction between these drugs and toll-like receptor 4 (TLR4) is unaddressed.
Methods
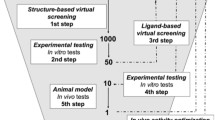
SN-38, the active metabolite of the Top I inhibitor irinotecan, and TLR4 interaction was assessed using the in vitro luciferase nuclear factor-κB reporter assay, neutrophil migration to murine air-pouch, in silico simulation, and the thermal shift assay (TSA). Topotecan was used as a positive anti-inflammatory control.
Results
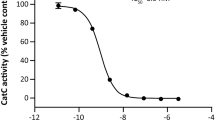
Non-cytotoxic concentrations of SN-38 attenuated LPS (a TLR4 agonist)-driven cell activation without affecting peptidoglycan (a TLR2 agonist)-activating response. Similarly, topotecan also prevented LPS-induced inflammation. Conversely, increasing concentrations of LPS reversed the SN-38 inhibitory effect. In addition, SN-38 abrogated LPS-dependent neutrophil migration and reduced TNF-α, IL-6, and keratinocyte chemoattractant levels in the air-pouch model, but failed to inhibit zymosan (a TLR2 agonist)-induced cell migration. A two-step molecular docking analysis indicated two potential binding sites for the SN-38 in the MD-2/TLR4 complex, the hydrophobic MD-2 pocket (binding energy of − 8.1 kcal/mol) and the rim of the same molecule (− 6.9 kcal/mol). The topotecan also bound to the MD-2 pocket. In addition, not only the lactone forms, but also the carboxylate conformations of both Top I inhibitors interacted with the MD-2 molecule. Furthermore, the TSA suggested the interaction of SN-38 with MD-2.
Conclusions
Therefore, SN-38 inhibits acute inflammation by blocking LPS-driven TLR4 signaling. This mechanism seems to be shared by other Top I inhibitors.



Similar content being viewed by others
Abbreviations
- AP-1:
-
Activator protein 1
- COX-2:
-
Cyclooxygenase-2
- DAMP:
-
Danger-associated molecular patterns
- DMSO:
-
Dimethyl sulfoxide
- HTAB:
-
Hexadecyltrimethyl-ammonium bromide
- IL-1β:
-
Interleukin-1 beta
- IL-6:
-
Interleukin-6
- IL-8:
-
Interleukin-8
- iNOS:
-
Inducible nitric oxide synthase
- KC:
-
Keratinocyte chemoattractant
- LPS:
-
Lipopolysaccharide
- MD-2:
-
Myeloid differentiation-2
- MPO:
-
Myeloperoxidase
- MyD88:
-
Myeloid differentiation primary response 88
- NF-κB:
-
Nuclear factor-κappa B
- PAMP:
-
Pathogen-associated molecular patterns
- PBS:
-
Phosphate buffered saline
- PGN:
-
Peptidoglycan
- PMA:
-
Phorbol 12-myristate 13-acetate
- SN-38:
-
7-Ethyl-10-hydroxycamptothecin
- TLR2:
-
Toll-like receptor 4
- TLR4:
-
Toll-like receptor 2
- TLRs:
-
Toll-like receptors
- TNF-α:
-
Tumor necrosis factor-alpha
- Top I:
-
Topoisomerase I
References
Liston A, Masters SL (2017) Homeostasis-altering molecular processes as mechanisms of inflammasome activation. Nat Rev Immunol 17:208–214
O’Neill LAJ, Golenbock D, Bowie AG (2013) The history of Toll-like receptors—redefining innate immunity. Nat Rev Immunol 13:453–460. https://doi.org/10.1038/nri3446
Rosadini CV, Kagan JC (2017) Early innate immune responses to bacterial LPS. Curr Opin Immunol 44:14–19
Wang JQ, Jeelall YS, Ferguson LL, Horikawa K (2014) Toll-like receptors and cancer: MYD88 mutation and inflammation. Front Immunol 5:1–10
Awasthi S (2014) Toll-like receptor-4 modulation for cancer immunotherapy. Front Immunol 5:1–5. https://doi.org/10.3389/fimmu.2014.00328
Shurin MR (2013) Dual role of immunomodulation by anticancer chemotherapy. Nat Med 19:20–22. https://doi.org/10.1038/nm.3045
Ding AH, Porteu F, Sanchez E, Nathan CF (1990) Shared actions of endotoxin and taxol on TNF receptors and TNF release. Science 248:370–372. https://doi.org/10.1126/Science.1970196
Kawasaki K, Akashi S, Shimazu R et al (2000) Mouse toll-like receptor 4.MD-2 complex mediates lipopolysaccharide-mimetic signal transduction by Taxol. J Biol Chem 275:2251–2254. https://doi.org/10.1074/jbc.275.4.2251
Wanderley CW, Colon DF, Luiz JPM et al (2018) Paclitaxel reduces tumor growth by reprogramming tumor-associated macrophages to an M1-profile in a TLR4-dependent manner. Cancer Res 78:5891–5900. https://doi.org/10.1158/0008-5472.CAN-17-3480
Rialdi A, Campisi L, Zhao N et al (2016) Topoisomerase 1 inhibition suppresses inflammatory genes and protects from death by inflammation. Science 352:7993. https://doi.org/10.1126/science.aad7993
Adams D (2005) The impact of tumor physiology on camptothecin-based drug development. Curr Med Chem Agents 5:1–13. https://doi.org/10.2174/1568011053352596
Danos O, Davies K, Lehn P, Mulligan R (2010) The ARRIVE guidelines, a welcome improvement to standards for reporting animal research. J Gene Med 12:559–560. https://doi.org/10.1002/jgm.1472
Gao H, Zhang X, Chen Y et al (2005) Synthesis and antitumor activity of 7-ethyl-9-alkyl derivatives of camptothecin. Bioorganic Med Chem Lett 15:2003–2006. https://doi.org/10.1016/j.bmcl.2005.02.072
Wang M, Wang L, Guo Y et al (2015) The broad pattern recognition spectrum of the Toll-like receptor in mollusk Zhikong scallop Chlamys farreri. Dev Comp Immunol 52:192–201. https://doi.org/10.1016/j.dci.2015.05.011
Busuttil V, Bottero V, Frelin C et al (2002) Blocking NF-κB activation in Jurkat leukemic T cells converts the survival agent and tumor promoter PMA into an apoptotic effector. Oncogene 21:3213–3224. https://doi.org/10.1038/sj/onc/1205433
Skehan P, Storeng R, Scudiero D et al (1990) New colorimetric cytotoxicity assay for anticancer-drug screening. J Natl Cancer Inst 82:1107–1112. https://doi.org/10.1093/jnci/82.13.1107
Wittmann M, Penzkofer A (1993) Concentration-dependent absorption and emission behaviour of sulforhodamine B in ethylene glycol. Chem Phys 172:339–348. https://doi.org/10.1016/0301-0104(93)80128-V
Boyd MR, Paull KD (1995) Some practical considerations and applications of the national cancer institute in vitro anticancer drug discovery screen. Drug Dev Res 34:91–109. https://doi.org/10.1002/ddr.430340203
Sin Y, Sedgwick A, Chea EP, Willoughby D (1986) Mast cells in newly formed lining tissue during acute inflammation: a six day air pouch model in the mouse. Ann Rheum Dis 45:873–877. https://doi.org/10.1136/ard.45.10.873
Leite ACRM, Cunha FQ, Dal-Secco D et al (2009) Effects of nitric oxide on neutrophil influx depends on the tissue: role of leukotriene B4 and adhesion molecules. Br J Pharmacol 156:818–825. https://doi.org/10.1111/j.1476-5381.2008.00094.x
Dornelas-Filho AF, Pereira VBM et al (2018) Neutrophils contribute to the pathogenesis of hemorrhagic cystitis induced by ifosfamide. Int Immunopharmacol 62:96–108. https://doi.org/10.1016/j.intimp.2018.06.031
Morris G, Huey R, Lindstrom W et al (2009) AutoDock4 and AutoDockTools4: automated docking with selective receptor flexibility. J Comput Chem 30:2785–2791. https://doi.org/10.1002/jcc.21256.AutoDock4
Pettersen EF, Goddard TD, Huang CC et al (2004) UCSF Chimera—a visualization system for exploratory research and analysis. J Comput Chem 25:1605–1612. https://doi.org/10.1002/jcc.20084
Andreotti G, Monticelli M, Cubellis MV (2015) Looking for protein stabilizing drugs with thermal shift assay. Drug Test Anal 7:831–834. https://doi.org/10.1002/dta.1798
Ribeiro-Filho HV, Videira NB, Bridi AV et al (2018) Screening for PPAR non-agonist ligands followed by characterization of a hit, AM-879, with additional no-adipogenic and cdk5-mediated phosphorylation inhibition properties. Front Endocrinol (Lausanne) 9:1–12. https://doi.org/10.3389/fendo.2018.00011
Videira NB, Batista FAH, Torres Cordeiro A, Figueira ACM (2018) Cellular and biophysical pipeline for the screening of peroxisome proliferator-activated receptor beta/delta agonists: avoiding false positives. PPAR Res 2018:3681590. https://doi.org/10.1155/2018/3681590
Holden NS, Squires PE, Kaur M et al (2008) Phorbol ester-stimulated NF-kappaB-dependent transcription: roles for isoforms of novel protein kinase C. Cell Signal 20:1338–1348. https://doi.org/10.1016/j.cellsig.2008.03.001
Huang Z, Zhao C, Chen Y et al (2014) Recombinant human hyaluronidase PH20 does not stimulate an acute inflammatory response and inhibits lipopolysaccharide-induced neutrophil recruitment in the air pouch model of inflammation. J Immunol 192:5285–5295. https://doi.org/10.4049/jimmunol.1303060
Mancuso F, Calignano A, Cozzolino A et al (1996) Inhibition of zymosan-induced air-pouch inflammation by rat seminal vesicle protein and by its spermidine derivative. Eur J Pharmacol 312:327–332. https://doi.org/10.1016/0014-2999(96)00394-9
Aomatsu K, Kato T, Fujita H et al (2008) Toll-like receptor agonists stimulate human neutrophil migration via activation of mitogen-activated protein kinases. Immunology 123:171–180. https://doi.org/10.1111/j.1365-2567.2007.02684.x
Lima-Júnior RCP, Freitas HC, Wong DVT et al (2014) Targeted inhibition of IL-18 attenuates irinotecan-induced intestinal mucositis in mice. Br J Pharmacol 171:2335–2350. https://doi.org/10.1111/bph.12584
Leite CAVG, Alencar VTL, Melo DLR et al (2015) Target inhibition of IL-1 receptor prevents ifosfamide induced hemorrhagic cystitis in mice. J Urol 194:1777–1786. https://doi.org/10.1016/j.juro.2015.07.088
Wong DVT, Lima-júnior RCP, Carvalho CBM (2015) The Adaptor Protein Myd88 Is a Key Signaling Molecule in the Pathogenesis of Irinotecan-Induced Intestinal Mucositis 10:e0139985. https://doi.org/10.1371/journal.pone.0139985
Pachman DR, Qin R, Seisler D et al (2016) Comparison of oxaliplatin and paclitaxel-induced neuropathy (Alliance A151505). Support Care Cancer 24:5059–5068. https://doi.org/10.1007/s00520-016-3373-1
Bao T, Basal C, Seluzicki C et al (2016) Long-term chemotherapy-induced peripheral neuropathy among breast cancer survivors: prevalence, risk factors, and fall risk. Breast Cancer Res Treat 159:327–333. https://doi.org/10.1007/s10549-016-3939-0
Byrd-Leifer CA, Block EF, Takeda K et al (2001) The role of MyD88 and TLR4 in the LPS-mimetic activity of Taxol. Eur J Immunol 31:2448–2457. https://doi.org/10.1002/1521-4141(200108)31:8%3c2448:AID-IMMU2448%3e3.0.CO;2-N
Li Y, Zhang H, Zhang H et al (2014) Toll-like receptor 4 signaling contributes to Paclitaxel-induced peripheral neuropathy. J Pain 15:712–725. https://doi.org/10.1016/j.jpain.2014.04.001
Underhill DM, Ozinsky A, Hajjar AM et al (1999) The Toll-like receptor 2 is recruited to macrophage phagosomes and discriminates between pathogens. Nature 401:811–815. https://doi.org/10.1038/44605
Billod JM, Lacetera A, Guzmán-Caldentey J, Martín-Santamaría S (2016) Computational approaches to Toll-like receptor 4 modulation. Molecules. https://doi.org/10.3390/molecules21080994
Kuzmich N, Sivak K, Chubarev V, et al (2017) TLR4 Signaling Pathway Modulators as Potential Therapeutics in Inflammation and Sepsis. Vaccines. https://doi.org/10.3390/vaccines5040034
Shimazu R, Akashi S, Ogata H et al (1999) MD-2, a molecule that confers lipopolysaccharide responsiveness on Toll-like receptor 4. J Exp Med 189:1777–1782. https://doi.org/10.1084/jem.189.11.1777
Chu M, Ding R, Chu Z et al (2014) Role of berberine in anti-bacterial as a high-affinity LPS antagonist binding to TLR4/MD-2 receptor. BMC Complement Altern Med 14:1–9. https://doi.org/10.1186/1472-6882-14-89
Wang Y, Shan X, Chen G et al (2015) MD-2 as the target of a novel small molecule, L6H21, in the attenuation of LPS-induced inflammatory response and sepsis. Br J Pharmacol 172:4391–4405. https://doi.org/10.1111/bph.13221
Gradisar H, Keber MM, Pristovsek P, Jerala R (2007) MD-2 as the target of curcumin in the inhibition of response to LPS. J Leukoc Biol 82:968–974. https://doi.org/10.1189/jlb.1206727
Teghanemt A, Re F, Prohinar P et al (2008) Novel roles in human MD-2 of phenylalanines 121 and 126 and tyrosine 131 in activation of Toll-like receptor 4 by endotoxin. J Biol Chem 283:1257–1266. https://doi.org/10.1074/jbc.M705994200
Grøftehauge MK, Hajizadeh NR, Swann MJ, Pohl E (2015) Protein-ligand interactions investigated by thermal shift assays (TSA) and dual polarization interferometry (DPI). Acta Crystallogr Sect D Biol Crystallogr 71:36–44. https://doi.org/10.1107/S1399004714016617
Damian L (2013) Isothermal titration calorimetry for studying protein-ligand interactions. Methods Mol Biol 1008:103–118. https://doi.org/10.1007/978-1-62703-398-5_4
Wardill HR, Gibson RJ, Van Sebille YZA et al (2016) Irinotecan-induced gastrointestinal dysfunction and pain are mediated by common TLR4-dependent mechanisms. Mol Cancer Ther 15:1376–1386. https://doi.org/10.1158/1535-7163.MCT-15-0990
Riehl T, Cohn S, Tessner T et al (2000) Lipopolysaccharide is radioprotective in the mouse intestine through a prostaglandin-mediated mechanism. Gastroenterology 118:1106–1116. https://doi.org/10.1016/S0016-5085(00)70363-5
Khan S, Wardill HR, Bowen JM (2018) Role of toll-like receptor 4 (TLR4)-mediated interleukin-6 (IL-6) production in chemotherapy-induced mucositis. Cancer Chemother Pharmacol 82:31–37. https://doi.org/10.1007/s00280-018-3605-9
Acknowledgements
We are grateful to Giuliana Bertozi, Diva Amabile, Ana Katia dos Santos, Sergio Roberto Rosa, Ieda Regina dos Santos, Maria Silvandira Freire Socorro França, and José Olavo Morais for technical assistance.
Funding
This study was supported by CNPq (Conselho Nacional de Desenvolvimento Científico e Tecnológico, Grant numbers: 307143/2014–7 and 428354/2016–5), FUNCAP (Fundação Cearense de Apoio ao Desenvolvimento Científico, Grant number: PR2-0101-00054.01.00/15) and CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior). This manuscript is dedicated to the loving memory of Prof. Dr. Ronaldo Albuquerque Ribeiro (in memoriam).
Author information
Authors and Affiliations
Contributions
Study design: DVTW, CWSW, HVRF, NMNA, FQC, and RCPLJ. Performed the experiments: DVTW, CWSW, HVRF, CAVGL, JBL, ANBA, AGC, GLPB, RHG, KOS, and LPCB. Data analysis: DVTW, CWSW, HVEF, DVW, and TMC. Interpretation of the results: DVTW, NMNA, DVW, TMC, FQC, and RCPLJ. Wrote the paper: DVTW, HVRF, and RCPLJ. All the authors revised and approved the paper.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare they have no financial, personal, or professional interests to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wong, D.V.T., Ribeiro-Filho, H.V., Wanderley, C.W.S. et al. SN-38, the active metabolite of irinotecan, inhibits the acute inflammatory response by targeting toll-like receptor 4. Cancer Chemother Pharmacol 84, 287–298 (2019). https://doi.org/10.1007/s00280-019-03844-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-019-03844-z