Abstract
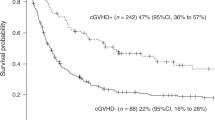
Patients with relapsed and refractory acute myeloid leukemia (R-R AML), especially those in non-remission (NR) have a poor prognosis after allogeneic hematopoietic stem cell transplantation (allo-HSCT). In order to optimize the entire allo-HSCT process for R-R AML patients and identify potential factors affecting clinical outcomes after HSCT, we retrospectively analyzed 44 adult patients with R-R AML who underwent salvage allo-HSCT while in NR or with concomitant extramedullary leukemia at the Institute of Hematology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology from 2013 to 2022. The 1-year and 2-year overall survival (OS) of the 44 patients were 55.3% (95% confidence interval [CI], 41.1%-74.3%) and 44.4% (95%CI, 30.2%-65.4%), respectively. The 1-year and 2-year cumulative incidence of relapse (CIR) were 39.4% (95%CI, 38.0%-40.7%) and 53.0% (95%CI, 51.0%-55.1%), respectively, and the 1-year and 2-year leukemia-free survival (LFS) were 37.8% (95%CI, 24.8%-57.7%) and 20.3% (95%CI, 9.1%-45.3%), respectively. The 100-day, 1-year and 2-year treatment-related mortality (TRM) was 13.8% (95%CI, 13.3%-14.4%), 22.8% (95%CI, 21.9%-23.7%) and 26.7% (95%CI, 25.5%-27.8%), respectively. Multivariate analysis revealed that patients who developed chronic graft-versus-host disease (cGVHD) after transplantation had lower relapse rate. Our analysis also indicated that patients with blast counts in bone marrow (BM) <20% and those with ≥20% had comparable clinical outcomes after allo-HSCT. In conclusion, our study demonstrated that R-R AML patients in NR or with concomitant extramedullary leukemia can benefit from allo-HSCT, regardless of leukemia burden at the time of transplantation. Patients who experience cGVHD after allo-HSCT may have lower relapse rate due to enhanced graft-versus-leukemia (GVL) effects, but cGVHD should be controlled at mild to moderate level to avoid life-threatening complications.



Similar content being viewed by others
References
Löwenberg B, Downing JR, Burnett A (1999) Acute myeloid leukemia. N Engl J Med 341:1051–1062. https://doi.org/10.1056/NEJM199909303411407
Döhner H, Estey EH, Amadori S et al (2010) Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood 115:453–474. https://doi.org/10.1182/blood-2009-07-235358
Othus M, Appelbaum FR, Petersdorf SH et al (2015) Fate of patients with newly diagnosed acute myeloid leukemia who fail primary induction therapy. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant 21:559–564. https://doi.org/10.1016/j.bbmt.2014.10.025
Estey E (2016) Why are there so few randomized trials for patients with primary refractory acute myeloid leukemia? Best Pract Res Clin Haematol 29:324–328. https://doi.org/10.1016/j.beha.2016.10.003
DeWolf S, Tallman MS (2020) How I treat relapsed or refractory AML. Blood 136:1023–1032. https://doi.org/10.1182/blood.2019001982
Evers G, Beelen DW, Braess J et al (2018) Outcome of Patients with Acute Myeloid Leukemia (AML) Undergoing Allogeneic Hematopoietic Stem Cell Transplantation (HSCT) Beyond First Complete Remission (CR1). Blood 132:4649. https://doi.org/10.1182/blood-2018-99-116964
Yan C-H, Wang Y, Sun Y-Q et al (2022) Optimized therapeutic strategy for patients with refractory or relapsed acute myeloid leukemia: long-term clinical outcomes and health-related quality of life assessment. Cancer Commun Lond Engl 42:1387–1402. https://doi.org/10.1002/cac2.12376
Estey EH (2000) Treatment of relapsed and refractory acute myelogenous leukemia. Leukemia 14:476–479. https://doi.org/10.1038/sj.leu.2401568
Ciftciler R, Demiroglu H, Buyukasık Y et al (2019) Efficacy and Feasibility of Allogeneic Hematopoietic Stem-Cell Transplantation in the Treatment of Refractory Acute Myeloid Leukemia. Clin Lymphoma Myeloma Leuk 19:177–182. https://doi.org/10.1016/j.clml.2018.11.016
Duval M, Klein JP, He W et al (2010) Hematopoietic stem-cell transplantation for acute leukemia in relapse or primary induction failure. J Clin Oncol 28:3730–3738. https://doi.org/10.1200/JCO.2010.28.8852
Zhang W-P, Yang D, Song X-M et al (2013) Allogeneic Peripheral Blood Stem Cell Transplantation is a Promising and Safe Choice for the Treatment of Refractory/Relapsed Acute Myelogenous Leukemia, Even with a Higher Leukemia Burden. Biol Blood Marrow Transplant 19:653–660. https://doi.org/10.1016/j.bbmt.2013.01.015
Jentzsch M, Grimm J, Bill M et al (2021) ELN risk stratification and outcomes in secondary and therapy-related AML patients consolidated with allogeneic stem cell transplantation. Bone Marrow Transplant 56:936–945. https://doi.org/10.1038/s41409-020-01129-1
Vardiman JW, Thiele J, Arber DA et al (2009) The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood 114:937–951. https://doi.org/10.1182/blood-2009-03-209262
Döhner H, Estey E, Grimwade D et al (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129:424–447. https://doi.org/10.1182/blood-2016-08-733196
Huang Z, Yan H, Teng Y et al (2022) Lower dose of ATG combined with basiliximab for haploidentical hematopoietic stem cell transplantation is associated with effective control of GVHD and less CMV viremia. Front Immunol 13:1017850. https://doi.org/10.3389/fimmu.2022.1017850
Reshef R (2012) Prevention of graft-versus-host disease. Clin Adv Hematol Oncol HO 10:663–665
Wang Y, Liu Q-F, Lin R et al (2021) Optimizing antithymocyte globulin dosing in haploidentical hematopoietic cell transplantation: long-term follow-up of a multicenter, randomized controlled trial. Sci Bull 66:2498–2505. https://doi.org/10.1016/j.scib.2021.06.002
Thomas ED, Storb R, Clift RA et al (1975) Bone-marrow transplantation (second of two parts). N Engl J Med 292:895–902. https://doi.org/10.1056/NEJM197504242921706
Filipovich AH, Weisdorf D, Pavletic S et al (2005) National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant 11:945–956. https://doi.org/10.1016/j.bbmt.2005.09.004
Stelljes M, Krug U, Beelen DW et al (2014) Allogeneic transplantation versus chemotherapy as postremission therapy for acute myeloid leukemia: a prospective matched pairs analysis. J Clin Oncol Off J Am Soc Clin Oncol 32:288–296. https://doi.org/10.1200/JCO.2013.50.5768
Gooley TA, Chien JW, Pergam SA et al (2010) Reduced mortality after allogeneic hematopoietic-cell transplantation. N Engl J Med 363:2091–2101. https://doi.org/10.1056/NEJMoa1004383
Horan JT, Logan BR, Agovi-Johnson M-A et al (2011) Reducing the risk for transplantation-related mortality after allogeneic hematopoietic cell transplantation: how much progress has been made? J Clin Oncol Off J Am Soc Clin Oncol 29:805–813. https://doi.org/10.1200/JCO.2010.32.5001
Devillier R, Crocchiolo R, Etienne A et al (2013) Outcome of relapse after allogeneic stem cell transplant in patients with acute myeloid leukemia. Leuk Lymphoma 54:1228–1234. https://doi.org/10.3109/10428194.2012.741230
Liga M, Triantafyllou E, Tiniakou M et al (2013) High alloreactivity of low-dose prophylactic donor lymphocyte infusion in patients with acute leukemia undergoing allogeneic hematopoietic cell transplantation with an alemtuzumab-containing conditioning regimen. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant 19:75–81. https://doi.org/10.1016/j.bbmt.2012.07.021
Jedlickova Z, Schmid C, Koenecke C et al (2016) Long-term results of adjuvant donor lymphocyte transfusion in AML after allogeneic stem cell transplantation. Bone Marrow Transplant 51:663–667. https://doi.org/10.1038/bmt.2015.234
Oran B, de Lima M, Garcia-Manero G et al (2018) Maintenance with 5-Azacytidine for Acute Myeloid Leukemia and Myelodysplastic Syndrome Patients. Blood 132:971. https://doi.org/10.1182/blood-2018-99-111582
(2018) Measurable residual disease-guided treatment with azacitidine to prevent haematological relapse in patients with myelodysplastic syndrome and acute myeloid leukaemia (RELAZA2): an open-label, multicentre, phase 2 trial. Lancet Oncol 19:1668–1679. 10.1016/S1470-2045(18)30580-1
Burchert A, Bug G, Fritz LV et al (2020) Sorafenib Maintenance After Allogeneic Hematopoietic Stem Cell Transplantation for Acute Myeloid Leukemia With FLT3-Internal Tandem Duplication Mutation (SORMAIN). J Clin Oncol Off J Am Soc Clin Oncol 38:2993–3002. https://doi.org/10.1200/JCO.19.03345
Perl AE, Larson RA, Podoltsev NA et al (2022) Follow-up of patients with R/R FLT3-mutation-positive AML treated with gilteritinib in the phase 3 ADMIRAL trial. Blood 139:3366–3375. https://doi.org/10.1182/blood.2021011583
Griffin JD, Song Y, Yang H et al (2021) Post-transplant maintenance therapy in patients with FLT3-mutated acute myeloid leukemia: Real-world treatment patterns and outcomes. Eur J Haematol 107:553–565. https://doi.org/10.1111/ejh.13692
Stern M, de Wreede LC, Brand R et al (2014) Sensitivity of hematological malignancies to graft-versus-host effects: an EBMT megafile analysis. Leukemia 28:2235–2240. https://doi.org/10.1038/leu.2014.145
Schneidawind D, Federmann B, Faul C et al (2011) Allogeneic Hematopoietic Cell Transplantation with FLAMSA-RIC Can Overcome the Poor Prognosis of Primary Refractory or Relapsed AML. Blood 118:1938. https://doi.org/10.1182/blood.V118.21.1938.1938
Peters C, Dalle J-H, Locatelli F et al (2021) Total Body Irradiation or Chemotherapy Conditioning in Childhood ALL: A Multinational, Randomized, Noninferiority Phase III Study. J Clin Oncol Off J Am Soc Clin Oncol 39:295–307. https://doi.org/10.1200/JCO.20.02529
Welniak LA, Blazar BR, Murphy WJ (2007) Immunobiology of allogeneic hematopoietic stem cell transplantation. Annu Rev Immunol 25:139–170. https://doi.org/10.1146/annurev.immunol.25.022106.141606
Bakst RL, Tallman MS, Douer D, Yahalom J (2011) How I treat extramedullary acute myeloid leukemia. Blood 118:3785–3793. https://doi.org/10.1182/blood-2011-04-347229
Fianchi L, Quattrone M, Criscuolo M et al (2021) Extramedullary Involvement in Acute Myeloid Leukemia. A Single Center Ten Years’ Experience. Mediterr J Hematol. Infect Dis 13:e2021030. https://doi.org/10.4084/MJHID.2021.030
Goyal SD, Zhang M-J, Wang H-L et al (2015) Allogeneic hematopoietic cell transplant for AML: no impact of pre-transplant extramedullary disease on outcome. Bone Marrow Transplant 50:1057–1062. https://doi.org/10.1038/bmt.2015.82
Lu Y, Zhao Y-L, Zhang J-P et al (2020) Unmanipulated haplo-identical donor transplantation compared with identical sibling donor had better anti-leukemia effect for refractory/relapsed acute myeloid leukemia not in remission status. Ann Hematol 99:2911–2925. https://doi.org/10.1007/s00277-020-04283-0
Wang Y, Chen H, Chen J et al (2018) The consensus on the monitoring, treatment, and prevention of leukemia relapse after allogeneic hematopoietic stem cell transplantation in China. Cancer Lett 438:63–75. https://doi.org/10.1016/j.canlet.2018.08.030
Wang Y, Liu Q-F, Wu D-P et al (2020) Impact of prophylactic/preemptive donor lymphocyte infusion and intensified conditioning for relapsed/refractory leukemia: a real-world study. Sci China Life Sci 63:1552–1564. https://doi.org/10.1007/s11427-019-1610-2
Guo H, Chang Y-J, Hong Y et al (2021) Dynamic immune profiling identifies the stronger graft-versus-leukemia (GVL) effects with haploidentical allografts compared to HLA-matched stem cell transplantation. Cell Mol Immunol 18:1172–1185. https://doi.org/10.1038/s41423-020-00597-1
Acknowledgements
We would like to thank the faculty members who collected the assembled the data.
Funding
National Natural Science Foundation of China, Grant/Award Number: 81974003; Collaborative Innovation Center of Hematology of China.
Author information
Authors and Affiliations
Contributions
Shan Jiang: writing—original draft; Xuan Lu: formal analysis; Ruowen Wei: data collection; Ao Zhang: data collection; Haoran Chen: data collection; Wei Shi: review and editing; Linghui Xia: review and editing.
Corresponding authors
Ethics declarations
This retrospective study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Ethical Committee of Wuhan Union Hospital in China approved this study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 22 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiang, S., Lu, X., Wei, R. et al. Salvage hematopoietic stem cell transplantation for patients with higher leukemia burden in relapsed or refractory acute myeloid leukemia: a ten-year study. Ann Hematol 102, 3205–3216 (2023). https://doi.org/10.1007/s00277-023-05406-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05406-z