Abstract
The objective of this study is to explore the clinical features and outcomes of pediatric patients with acute lymphoblastic leukemia (ALL) harboring JAK-STAT signaling pathway genetic abnormalities. This retrospective case series examined the clinical data of pediatric patients diagnosed with ALL harboring JAK-STAT pathway genetic abnormality at the Children’s Hospital of the Capital Institute of Pediatrics between January 2016 and January 2022. Bone marrow next-generation sequencing was used to reveal the JAK pathway abnormalities. Descriptive statistics were used. From 432 children with ALL during the study period, eight had JAK-STAT pathway genetic abnormalities. Regarding immunotyping, there were four patients with common-B cell types and one with pre-B cell type. The three patients with T-ALL had early T-cell precursor(ETP) type, pre-T cell type, and T cell type. Gene mutations were more common than fusion genes. There was no central nervous system involvement in eight patients. All patients were considered at least at intermediate risk before treatments. Four patients underwent hematopoietic stem cell transplantation (HSCT). One child had a comprehensive relapse and died. The child had a severe infection and could not tolerate high-intensity chemotherapy. Another child relapsed 2 years after HSCT and died. Disease-free survival was achieved in six children. JAK-STAT pathway genetic abnormalities in pediatric Ph-like ALL are rare. Special attention should be paid to treatment-related complications, such as infection and combination therapy (chemotherapy, small molecule targeted drugs, immunotherapy, etc.) to reduce treatment-related death and improve long-term quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute lymphoblastic leukemia (ALL) is the most common cancer in children [1]. The overall incidence of ALL in China is 39.34 per million people and 43.33 per million people in children (0–14 years old) [2]. ALL is classified by immunophenotype: 80–85% of pediatric ALL cases are B-cell ALL (B-ALL), while about 15% are T-cell ALL (T-ALL) [3, 4]. Patient characteristics, cytogenetics, and response to initial treatment are prognostic factors and are used in combination with immunophenotype for risk stratification to determine the treatment strategy [1, 3, 4]. The 5-year disease-free survival (DFS) and overall survival (OS) rates of pediatric ALL have been significantly improved by risk stratification and tailored treatments [5, 6]. Chimeric antigen receptor T cell (CAR-T) therapy, monoclonal antibody (mAb)-based therapies, cancer vaccines, adoptive cell therapy (ACT), and oncolytic viruses have created a new era in the treatment of leukemia [7, 8]. Nevertheless, about 20% of the patients display poor treatment efficacy and are prone to relapse [5, 6].
The advances in genome mapping techniques over the past decade (such as transcriptome and whole-genome sequencing) allowed the reproducible identification of several genetic abnormalities with prognostic significance in ALL [9, 10]. Philadelphia chromosome-like (Ph-like) ALL is a group of disorders characterized by molecular abnormalities primarily associated with activating cytokine receptors and kinase signaling pathways, including abnormalities in the JAK kinase pathway [9, 10]. Ph-like ALL represents about 10–15% of standard and high-risk pediatric B-ALL cases [9, 10]. The involvement of the JAK-STAT signaling in Ph-like ALL includes JAK2 gene rearrangements with at least 10 possible fusion partners and point mutations in CRLF2, JAK1, and JAK2, all leading to JAK-STAT signaling activation [9, 10]. Constitutive JAK-STAT activation promotes ALL development and progression [11]. Most cytokine receptors involved in regulating hematopoiesis rely on JAK for triggering downstream cellular signaling. Ligand binding to cytokine receptors activates the receptor-associated JAKs and leads to phosphorylation and activation of the signal transducers and activators of transcription STAT1–6 transcription factors and cytokine-specific gene responses [12]. The aberrant regulation of the JAK-STAT pathway is involved in several malignancies [13]. About 140 different JAK mutations have been linked to different types of leukemia, demonstrating the role of JAKs in leukemogenesis. The pseudokinase (JH2) domain is a critical regulator of JAK activity, with positive and negative regulatory functions. Many JAK2 mutations in JH2 result in JAK pathway hyperactivation, leading to various malignancies [14]. Activating JAK2 or JAK1 point mutations occur in about half of CRLF2-R ALL cases. The most common mutation is R683G in the JAK2 pseudokinase domain. CRLF2 overexpression and JAK2 mutations induce transformation in vitro through the constitutive activation of JAK-STAT signaling [15,16,17,18,19,20].
Mutations and gene rearrangements all represent opportunities for precision medicine. A wide variety of point mutations and gene rearrangements have been described, and owing to the complex relationships between mutant JAK2 and cytokine receptors, not all mutations and rearrangements will impact prognosis similarly. Therefore, there is a need to improve the knowledge about the genetic landscape of ALL with JAK-STAT pathway genetic abnormalities. Hence, this study aimed to explore the clinical features and outcomes of pediatric patients with ALL with JAK-STAT pathway genetic abnormalities. The results could help improve the management and prognosis of pediatric ALL with JAK-STAT pathway genetic abnormalities.
Methods
Study design and patients
This retrospective case series examined the clinical data of children diagnosed with ALL with JAK-STAT pathway genetic abnormality at the Hematology Department of the Children’s Hospital of the Capital Institute of Pediatrics between January 2016 and January 2022. This study was approved by the Ethics Committee of the Capital Institute of Pediatrics. As a retrospective study, the requirement for informed patient consent was waived by the committee.
The inclusion criteria were (1) newly diagnosed patients aged 0–16 years; (2) diagnosed and classified as ALL meeting the World Health Organization (WHO) 2016 bone marrow morphological criteria by morphology, immunophenotype, cytogenetics, and molecular biology (MICM); and (3) bone marrow next-generation sequencing (NGS) revealed JAK-STAT pathway gene mutation or fusion gene. The exclusion criteria were (1) did not receive induction therapy at the study hospital, (2) incomplete clinical data, or (3) have any prior treatment.
Data collection
The baseline data of the patients were collected from the medical records, including age, sex, peripheral white blood cell (WBC) counts at disease onset, diagnosis, immunological typing, gene mutation, Ph-like fluorescence in situ hybridization (FISH), fusion gene, chromosome karyotype, risk ratio at first diagnosis, moderate-to-high risk factors at initial diagnosis, bone marrow cytology (day 15 and 33), minimal residual disease (MRD) (day 15 and 33), adjusted risk stratification, risk assessment after remission, causes of risk stratification adjustment, bone marrow cytology before consolidation, hematopoietic stem cell transplantation (HSCT), and survival. Genomic DNA and NGS were used to assess the percentage of progenitor cells in the bone marrow and gene mutation. Bone marrow cytology on day 15 and 33 and MRD was analyzed by flow cytology. All children were treated using the regimens recommended by the Chinese Children’s Leukemia Group (CCLG)-ALL (Supplementary Tables S1 and S2).
Statistical analysis
Only descriptive statistics were used. Continuous data with a normal distribution were described using means ± standard deviations. Continuous data with a skewed distribution were described as median (range). Categorical data were described as n (%).
Results
Clinical features
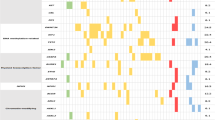
This study included eight pediatric patients with ALL harboring JAK-STAT pathway genetic abnormalities. The characteristics of the patients are shown in Table 1. The patients were aged between 5 and 11 years. There were five males and three females. None of the patients had central nervous system leukemia. Six patients had high WBC counts. All patients with B-ALL showed high WBC counts, while T-ALL started with an obvious neck mass. Regarding the immunotyping of B-ALL, there were four common-B cell types and one pre-B cell type. The three patients with T-ALL had early T-cell precursor ALL (ETP-ALL), pre-T cell ALL, and T cell ALL, respectively. All patients were considered at least medium risk before treatment (#1 because of age and high WBC; #2 and #3 because of high WBC; #4 because of age and T-ALL; #5 because of high WBC; #6 was because of WBC and T-ALL; #7 because of high WBC and age; #8 because of age and T-ALL) (Table 1). Seven patients had gene mutations in the JAK-STAT pathway, all of which were somatic mutations, and the mutation types were all missense mutations. Three patients had JAK1 gene mutations, and the other four had JAK2 gene mutations. One patient had a JAK1 K911N mutation not reported in the literature but was found to have CRLF2 deletion by FISH. The JAK1/2 mutations in the remaining six patients have been reported and shown to increase JAK2 activity or STAT5 phosphorylation. One patient with no mutation in the JAK-STAT pathway gene had a PCM1-JAK2 fusion gene with JAK2 gene rearrangement that might lead to constitutive activation of the JAK2 kinase domain (Table 1). Unfortunately, these patients were not tested for STAT5 phosphorylation levels or protein effects. Patient #3 underwent transcriptome testing, and the corresponding JAK2 gene mutation was found.
Treatment features
All patients were newly diagnosed. Initial treatment for all patients was started on the CCLG-ALL regimen. Initial induction therapy included four doses of vindesine 3 mg/m2 (day 8, 15, 22, and 29), four doses of daunorubicin 30 mg/m2 (day 8, 15, 22, and 29), two doses of pegaspargase 2500 IU/m2 (day 9 and 23), and 35 days of prednisone 60 mg/m2 (B-ALL) or dexamethasone 6 mg/m2 (T-ALL). Patient #2 was insensitive to prednisone induction, and cytarabine 100 mg/m2 each time was added for debulking treatment; in addition, daunorubicin was replaced by idarubicin to enhance the intensity of chemotherapy. According to the CCLG risk stratification criteria, all patients were at least intermediate risk on day 15 of remission induction (patients #2, #3, #4, and #8 were high risk). The risk stratification based on treatment responses showed that not all patients were at high risk: four patients were elevated to high risk (patients #2, #3, #4, and #8). Specifically, the bone marrow cytology of patients #2, #3, and #8 showed no remission, and flow cytometry showed MRD > 10−1 on day 15; thus, the patients were classified as high risk. Flow cytometry showed MRD > 10−2 in patient #4 on day 33 and > 10−2 in patients #2 and #8 on day 33. Four patients were still intermediate risk (patients #1, #5, #6, and #7), and flow cytometry showed MRD > 10−3 in patients #1, #5, and #7 on day 15 to the bone marrow reexamination on day 15. The drug therapy was only prednisone/dexamethasone once a day, one dosing of anthracycline (daunorubicin or idarubicin), one dosing of vindesine (day 8), and one dosing of pegaspargase (day 9). Chemotherapy on day 15 was started after reexamination.
The most major complication was an infection. Three of the eight patients (patients #1, #2, and #6) had very severe infections during the induction therapy, directly influencing the subsequent treatments. Patient #1 had a recurrent fever and intra-abdominal infection during induction chemotherapy. The detected pathogens were Escherichia coli and Klebsiella pneumoniae. The blood, cerebrospinal fluid, and bronchoalveolar lavage fluid of patient #2 successively showed Elizabethkingia anophelis infection and Candida infection during induction chemotherapy. Patient #2 presented severe pneumonia, central nervous system infection, abdominal infection, and systemic fungal infection, resulting in septic shock and respiratory failure. Patient #2 received intensive care unit (ICU) treatment for more than 1 month before his condition improved. Patient #6 developed pneumococcal sepsis and meningitis during induction therapy. Patient #6 also developed septic shock requiring ICU treatment.
Survival and prognosis
In this study, two patients died, and six survived. Three children received regular chemotherapy and achieved good outcomes. Patient #1 could not tolerate regular high-intensity chemotherapy due to severe infections. The family abandoned delayed intensive and maintenance treatment and turned to Traditional Chinese Medicine (TCM) therapy. Patient #1 died of relapse 9 months after the initial diagnosis. Chemotherapy intensity had to be reduced in patient #6 by using pegaspargase once less in the second chemotherapy. Patient #6 subsequently received regular chemotherapy and is currently on maintenance therapy. One patient who received transplantation group experienced relapse and died, and three patients achieved long-term survival. Patients #2 and #5 had grade IV acute graft versus host disease (GVHD). Patient #2 experienced a relapse and died 23 months after transplantation. Patient #5 had moderate chronic GVHD, with clinical manifestations of extensive skin depigmentation, nausea, dyspepsia, wheezing, and limited physical activity. Lung computed tomography (CT) showed small airway lesions, and pulmonary function tests showed obstructive ventilation dysfunction. Patient #5 was treated with oral montelukast, nebulized budesonide, and intermittent oral low-dose azithromycin and methylprednisolone. He still has limited physical activity, cannot perform exercise, and his quality of life is affected (Table 2).
Discussion
This study aimed to explore the clinical features and outcomes of pediatric ALL harboring JAK-STAT signaling pathway genetic abnormalities. The results suggest that, in a limited sample, the number of survivors who received a transplant or chemotherapy was the same. Neither of the two patients who died received regular or complete treatment. The patients who received regular treatment all survived. The completion of chemotherapy might be an important factor affecting prognosis. FISH is helpful for the early detection of molecular biological abnormalities because test results are available faster than NGS. For children with a poor early response, how to adjust treatment (e.g., JAK inhibitors, berintuozumab, or combination therapy) to avoid infection, organ toxicity, and other complications and to achieve a given intensity of chemotherapy will have to be explored.
The frequency of JAK-STAT pathway genetic abnormalities is about 3–5% in children and up to 16% in adults with ALL [31]. The frequency of JAK-STAT genetic abnormalities can reach 10.7% in patients with BCR-ABL1-negative, high-risk pediatric ALL [32]. In the present study, only eight patients were identified over 6 years at a tertiary hospital specializing in pediatric hematological malignancies, indicating that it is rare in children. Steeghs et al. [33] analyzed the JAK2 mutation status in 461 newly diagnosed BCP-ALL cases, revealing that 3.5% (16/461) of these BCP-ALL cases harbored JAK2 mutations. JAK1 mutations are more common in T-ALL and were identified in approximately 20% of adult T-ALL cases, with a much lower frequency in childhood T-ALL [26]. Previous studies suggested a predominance of JAK-STAT abnormalities in B-ALL, with only a few rare cases in T-ALL [34]. At a Lithuanian hospital, Norvilas et al. [35] identified four patients with JAK-STAT fusions and 10 with other JAK-STAT pathway mutations abnormalities out of 122 children and 38 adults with BCR-ABL1-negative B-ALL. Other groups reported relatively low frequencies of JAK-STAT abnormalities in ALL [32, 36,37,38,39,40]. Similar to the literature, the present study showed that the frequency of genetic abnormalities in the JAK-STAT pathway is very low in children with ALL, but no conclusion can be drawn regarding a possible association with JAK-STAT pathway genetic abnormalities because of the small sample size.
Previous studies showed that genetic abnormalities in the JAK-STAT pathway are associated with a poor prognosis of patients with leukemia [18, 28, 29, 39], but only limited data are available about patients with JAK-STAT abnormalities. Two molecular abnormalities in the JAK-STAT pathway found in this study were unreported. In the study by Norvilas et al. [35], all four patients had poor MRD responses after NOPHO ALL-2008 regimens and were categorized as high-risk, and the patients with JAK-STAT fusions had a poor prognosis compared with patients without JAK-STAT fusions. In the NOPHO ALL-2008 regimen, the induction therapy is vincristine, doxorubicin, and glucocorticosteroids. In the CCLG-ALL regimen, the induction therapy has two additional doses of pegaspargase, the first dose being on day 9. O’Connor et al. [41] observed that, among 44 B-ALL patients with induction failure, four patients harbored a CRLF2 rearrangement (PR2Y8-CRLF2, n = 3; and IGH-CRLF2, n = 1). The induction therapy of the standard risk regimen in the UKALL2003 regimen does not contain daunorubicin, and the dose of pegaspargase is 1000 IU/m2 in every risk regimen, which is less than the 2500 IU/m2 of the CCLG-ALL regimen. Mullingham et al. [16] reported poor event-free survival in pediatric patients with JAK-activating mutations. The 4-year cumulative incidence of events (relapse, death, or second malignancy) was 78.2% for patients with both a JAK mutation and IKZF1 alteration, compared with 54.4% for IKZF1 alteration only, 33.3% for JAK mutation only, and 24.3% for neither lesion [16]. The study used an augmented intensive regimen of post-induction chemotherapy. The most important difference from the CCLG-ALL regimen is using 6000 IU/m2 asparaginase. In the present study, all patients were treated with the CCLG-ALL strategy. No induction failure occurred, and a low MRD was achieved after induction. The molecular mechanisms leading to the different responses to treatment are unclear. Differences in regimens could explain, at least in part, the discrepancies among studies. Still, the treatment process was not smooth, and many patients experienced complications that led to delayed or lower-dose treatments, and the early remission rates were poor. Even though the prognosis was relatively good, there is room for improvement in the treatment strategies.
Infections are a major issue in patients treated for ALL. Indeed, infections (bacterial and/or fungal) are responsible for an important part of morbidity and mortality in children treated for ALL [42, 43]. ALL itself results in quantitative and qualitative deficits in lymphocytes, hypogammaglobulinemia, and reduced immunity, leading to a higher risk of infections and greater difficulties for the body to get rid of the infection [44]. Treatments for ALL can also result in neutropenia and disrupt the barrier functions of mucosal membranes, further increasing the risk of infections [44, 45]. Hence, infections are responsible for treatment delays, interruptions, terminations, or decreased dosages [45, 46], leading to a poor prognosis. In the present study, six patients had infectious events, and one of the eight patients had infections that prevented the normal course of treatment. That patient relapsed even after transplantation and died from ALL, probably because the early stages of therapy were of insufficient intensity because of the infections. Hence, infections during the early stages of ALL management can compromise the success of transplantation. Still, the frequency of infections was reported to be low with the CCLG-2008 strategy [47]. In the present study, three patients were treated with the CCLG-2008 strategy (all three with infection events) and five with CCLG-2018 (three had infections), but the sample size is too small to draw any conclusions. Nevertheless, infections remain a source of concern during ALL treatments and should be actively prevented to improve patient prognosis. Indeed, a study revealed that infection-related mortality represented 30% of deaths in pediatric patients with ALL participating in clinical trials [48].
Furthermore, the constitutive activation of the JAK-STAT pathway can induce an inflammatory response [49, 50]. In such a systemic pro-inflammatory condition, infection events can easily induce a cytokine storm, leading to increased organ damage after infection [51]. In sepsis models, the JAK/STAT pathway is involved in endotoxin shock, organ damage, and myocardial vascular permeability [52]. It is impossible to determine whether a JAK-STAT-activated proinflammatory environment or a cytokine storm was involved in the patients who died from infection-related complications. Still, this hypothesis could be considered for managing patients with ALL and JAK-STAT abnormalities in the future. Inhibiting the JAK-STAT pathway has been suggested to prevent the cytokine storm in patients with COVID-19 [53].
Inhibiting the JAK-STAT pathway appears to be a promising precision medicine strategy for patients with JAK-STAT activating mutations. JAK inhibitors do not eliminate the malignant clone [54], and the response to single-agent therapy is poor. Combination chemotherapy can be used as a therapeutic direction, with reports of successful cases [55]. Ruxolitinib exerted synergy with standard-of-care drugs used in treating ALL and enhanced the in vivo efficacy of an induction-type regimen consisting of vincristine, dexamethasone, and L-asparaginase in CRLF2-rearranged Ph-like ALL xenografts. Glucocorticoids constituted the major class of drugs showing potent combination effects with ruxolitinib. Ruxolitinib significantly decreased the expression of characteristic genes of Ph-like ALL and showed strong inhibitory effects on STAT5 phosphorylation in vitro. In addition, both phosphoproteomics and kinase array analyses found that ruxolitinib and dexamethasone, both as single agents and in combination, decreased tyrosine phosphorylation of proteins involved in the JAK-STAT signaling pathway [13].
However, research also suggests that mutations in alternative survival pathways and microenvironment-induced resistance can compromise the effect of JAK inhibition. Furthermore, inhibitors induce the accumulation of phosphorylated JAK2Y1007, resulting in a profound re-activation of JAK2 signaling upon release of the inhibitors. This preclinical evidence implies that further optimization and evaluation of JAK inhibitors are necessary prior to their clinical integration in pediatric ALL [33]. A clinical trial of phase 1/2 trial of ruxolitinib for acute leukemia (NCT01251965) was stopped by the principal investigators due to unsatisfactory clinical benefits, even in patients treated at the highest dose, after studying 13 patients. A phase 2 trial (NCT02723994) is being conducted to evaluate the safety and efficacy of ruxolitinib with chemotherapy in children with Ph-like ALL. The clinical trial demonstrated the safety and tolerability of ruxolitinib in combination with intensive multi-agent chemotherapy. Pharmacodynamic studies demonstrated a dose-dependent inhibition of target phosphoproteins and sustained inhibition of phosphorylated STAT5 with continuous ruxolitinib dosing at 40 mg/m2/dose each 28-day cycle [56]. Most patients demonstrated a marked decrement in MRD from the end of induction to the end of consolidation with ruxolitinib and consolidation chemotherapy. The optimal duration of JAK inhibitor therapy and potential response rates remain undefined [57]. Whether JAK-STAT inhibitors can improve the prognosis of patients with ALL harboring JAK-STAT pathway genetic abnormalities remains to be determined. Whether there is an increased rate of infections or secondary malignancies also remains to be determined in large patient cohorts. Such treatments might be particularly useful in patients unable to receive high-intensity chemotherapy. Ruxolitinib has also been reported in combination with CAR-T and hematopoietic stem cell therapy in patients with refractory relapse [58, 59]. Hence, increasing the intensity of chemotherapy may not be the best adjustment to the current hematologic tumor treatment strategy. Instead, attention should be paid to treatment-related complications, such as infection and organ toxicity, and combination therapy (chemotherapy, small molecule targeted drugs, immunotherapy, etc.) to reduce treatment-related death and improve long-term quality of life. From the perspective of treatment, the survival of chemotherapy and transplantation is comparable (one out of the four patients with regular chemotherapy died, and the death was due to the recurrence of infection due to failure to continue regular treatment; one out of the four patients with transplantation died, which may be due to insufficient chemotherapy intensity before transplantation). If regular chemotherapy can be guaranteed, transplantation may not be needed, or survival may be better. The main finding of this study is that early infection is a prominent issue (patients #1, #2, and #6). The common point of the two patients who died was that the infection prevailed. Both patients had systemic disseminated infections that occurred in the early stage of treatment, and the death was due to the recurrence caused by the failure of regular treatment. Therefore, attention should be paid to infection in such patients, which will compromise the treatment plan. Whether the incidence of infection increases in patients with ALL harboring JAK-STAT pathway genetic abnormalities needs to be further studied in large sample sizes. Still, how to reduce complications and ensure chemotherapy to achieve long-term survival remains an open question. Rapid initial molecular diagnosis and immediate introduction of JAK inhibitors after identifying JAK-STAT pathway genetic abnormalities could be an option to achieve better responses. A strategy based on chemotherapy plus a JAK inhibitor or chemotherapy plus immunotherapy should be explored to ensure regular, sustainable, and appropriate intensity chemotherapy. Thus, the efficacy of chemotherapy could be improved, the intensity of chemotherapy would be reduced (theoretically leading to a lower risk of infection and organ toxicity), and the transplantation requirements would be reduced. Indeed, according to these eight cases, transplantation appears to fail to solve the recurrence problem of this case.
This study had limitations. It was a case series from a single hospital during a limited period. The study period started in 2016 because NGS was not available before. Therefore, only eight patients could be identified, preventing any in-depth statistical analyses regarding treatment outcomes, prognosis, and treatments. In addition, the follow-up data were limited since all cases were relatively contemporary. This study used NGS to detect gene mutations and fusion genes affecting the JAK-STAT pathway, but no further analyses or simulations were performed to try to determine how they affected the JAK-STAT pathway. Some mutations had not been reported before or documented in gene banks. The mutations only occurred at the JAK gene or upstream of the JAK-STAT pathway. Therefore, it will be necessary to perform additional studies to examine the pathogenicity of the identified mutations. Multicenter studies could help increase the sample size for some rare mutations and help in their characterization.
In conclusion, JAK-STAT pathway abnormalities in pediatric Ph-like ALL are uncommon. Actively enhanced chemotherapy intensity and transplantation might be the keys to successful treatment. Still, attention to infection should be increased to prevent treatment-related mortality. The genetic map of ALL should be extensively investigated to improve the treatment effects in high-risk patients.
Data availability
All data generated or analyzed during this study are included in this article and its supplementary information file.
References
PDQ Pediatric Treatment Editorial Board (2022) Childhood acute lymphoblastic leukemia treatment (PDQ®): Patient version. In PDQ Cancer Information Summaries. National Cancer Institute (US)
Ni X, Li Z, Li X, Zhang X, Bai G, Liu Y, Zheng R, Zhang Y, Xu X, Liu Y, Jia C, Wang H, Ma X, Zheng H, Su Y, Ge M, Zeng Q, Wang S, Zhao J, Zeng Y, Feng G, Xi Y, Deng Z, Guo Y, Yang Z, Zhang J (2022) Socioeconomic inequalities in cancer incidence and access to health services among children and adolescents in China: a cross-sectional study. Lancet 400:1020–1032. https://doi.org/10.1016/S0140-6736(22)01541-0
Onciu M (2009) Acute lymphoblastic leukemia. Hematol Oncol Clin North Am 23:655–674. https://doi.org/10.1016/j.hoc.2009.04.009
Nazemi KJ, Malempati S (2009) Emergency department presentation of childhood cancer. Emerg Med Clin North Am 27:477–495. https://doi.org/10.1016/j.emc.2009.04.008
Neaga A, Jimbu L, Mesaros O, Bota M, Lazar D, Cainap S, Blag C, Zdrenghea M (2021) Why do children with acute lymphoblastic leukemia fare better than adults? Cancers (Basel) 13. https://doi.org/10.3390/cancers13153886
Capria S, Molica M, Mohamed S, Bianchi S, Moleti ML, Trisolini SM, Chiaretti S, Testi AM (2020) A review of current induction strategies and emerging prognostic factors in the management of children and adolescents with acute lymphoblastic leukemia. Expert Rev Hematol 13:755–769. https://doi.org/10.1080/17474086.2020.1770591
Safarzadeh Kozani P, Safarzadeh Kozani P, Rahbarizadeh F (2021) Optimizing the clinical impact of CAR-T cell therapy in B-cell acute lymphoblastic leukemia: looking back while moving forward. Front Immunol 12:765097. https://doi.org/10.3389/fimmu.2021.765097
Safarzadeh Kozani P, Safarzadeh Kozani P, Rahbarizadeh F (2021) CAR-T cell therapy in T-cell malignancies: is success a low-hanging fruit? Stem Cell Res Ther 12:527. https://doi.org/10.1186/s13287-021-02595-0
Roberts KG (2018) Genetics and prognosis of ALL in children vs adults. Hematol Am Soc Hematol Educ Program 2018:137–145. https://doi.org/10.1182/asheducation-2018.1.137
Mullighan CG (2014) The genomic landscape of acute lymphoblastic leukemia in children and young adults. Hematol Am Soc Hematol Educ Program 2014:174–180. https://doi.org/10.1182/asheducation-2014.1.174
Mullighan CG, Su X, Zhang J, Radtke I, Phillips LA, Miller CB, Ma J, Liu W, Cheng C, Schulman BA, Harvey RC, Chen IM, Clifford RJ, Carroll WL, Reaman G, Bowman WP, Devidas M, Gerhard DS, Yang W, Relling MV, Shurtleff SA, Campana D, Borowitz MJ, Pui CH, Smith M, Hunger SP, Willman CL, Downing JR, Children’s Oncology G (2009) Deletion of IKZF1 and prognosis in acute lymphoblastic leukemia. N Engl J Med 360:470–480. https://doi.org/10.1056/NEJMoa0808253
Kiu H, Nicholson SE (2012) Biology and significance of the JAK/STAT signalling pathways. Growth Factors 30:88–106. https://doi.org/10.3109/08977194.2012.660936
Hammaren HM, Virtanen AT, Raivola J, Silvennoinen O (2019) The regulation of JAKs in cytokine signaling and its breakdown in disease. Cytokine 118:48–63. https://doi.org/10.1016/j.cyto.2018.03.041
Raivola J, Haikarainen T, Abraham BG, Silvennoinen O (2021) Janus kinases in leukemia. Cancers (Basel) 13. https://doi.org/10.3390/cancers13040800
Mullighan CG, Collins-Underwood JR, Phillips LA, Loudin MG, Liu W, Zhang J, Ma J, Coustan-Smith E, Harvey RC, Willman CL, Mikhail FM, Meyer J, Carroll AJ, Williams RT, Cheng J, Heerema NA, Basso G, Pession A, Pui CH, Raimondi SC, Hunger SP, Downing JR, Carroll WL, Rabin KR (2009) Rearrangement of CRLF2 in B-progenitor- and Down syndrome-associated acute lymphoblastic leukemia. Nat Genet 41:1243–1246. https://doi.org/10.1038/ng.469
Mullighan CG, Zhang J, Harvey RC, Collins-Underwood JR, Schulman BA, Phillips LA, Tasian SK, Loh ML, Su X, Liu W, Devidas M, Atlas SR, Chen IM, Clifford RJ, Gerhard DS, Carroll WL, Reaman GH, Smith M, Downing JR, Hunger SP, Willman CL (2009) JAK mutations in high-risk childhood acute lymphoblastic leukemia. Proc Natl Acad Sci USA 106:9414–9418. https://doi.org/10.1073/pnas.0811761106
Russell LJ, Capasso M, Vater I, Akasaka T, Bernard OA, Calasanz MJ, Chandrasekaran T, Chapiro E, Gesk S, Griffiths M, Guttery DS, Haferlach C, Harder L, Heidenreich O, Irving J, Kearney L, Nguyen-Khac F, Machado L, Minto L, Majid A, Moorman AV, Morrison H, Rand V, Strefford JC, Schwab C, Tonnies H, Dyer MJ, Siebert R, Harrison CJ (2009) Deregulated expression of cytokine receptor gene, CRLF2, is involved in lymphoid transformation in B-cell precursor acute lymphoblastic leukemia. Blood 114:2688–2698. https://doi.org/10.1182/blood-2009-03-208397
Harvey RC, Mullighan CG, Chen IM, Wharton W, Mikhail FM, Carroll AJ, Kang H, Liu W, Dobbin KK, Smith MA, Carroll WL, Devidas M, Bowman WP, Camitta BM, Reaman GH, Hunger SP, Downing JR, Willman CL (2010) Rearrangement of CRLF2 is associated with mutation of JAK kinases, alteration of IKZF1, Hispanic/Latino ethnicity, and a poor outcome in pediatric B-progenitor acute lymphoblastic leukemia. Blood 115:5312–5321. https://doi.org/10.1182/blood-2009-09-245944
Yoda A, Yoda Y, Chiaretti S, Bar-Natan M, Mani K, Rodig SJ, West N, Xiao Y, Brown JR, Mitsiades C, Sattler M, Kutok JL, DeAngelo DJ, Wadleigh M, Piciocchi A, Dal Cin P, Bradner JE, Griffin JD, Anderson KC, Stone RM, Ritz J, Foa R, Aster JC, Frank DA, Weinstock DM (2010) Functional screening identifies CRLF2 in precursor B-cell acute lymphoblastic leukemia. Proc Natl Acad Sci USA 107:252–257. https://doi.org/10.1073/pnas.0911726107
Hertzberg L, Vendramini E, Ganmore I, Cazzaniga G, Schmitz M, Chalker J, Shiloh R, Iacobucci I, Shochat C, Zeligson S, Cario G, Stanulla M, Strehl S, Russell LJ, Harrison CJ, Bornhauser B, Yoda A, Rechavi G, Bercovich D, Borkhardt A, Kempski H, te Kronnie G, Bourquin JP, Domany E, Izraeli S (2010) Down syndrome acute lymphoblastic leukemia, a highly heterogeneous disease in which aberrant expression of CRLF2 is associated with mutated JAK2: a report from the International BFM Study Group. Blood 115:1006–1017. https://doi.org/10.1182/blood-2009-08-235408
Zhao L, Dong H, Zhang CC, Kinch L, Osawa M, Iacovino M, Grishin NV, Kyba M, Huang LJ (2009) A JAK2 interdomain linker relays Epo receptor engagement signals to kinase activation. J Biol Chem 284:26988–26998. https://doi.org/10.1074/jbc.M109.011387
Hornakova T, Springuel L, Devreux J, Dusa A, Constantinescu SN, Knoops L, Renauld JC (2011) Oncogenic JAK1 and JAK2-activating mutations resistant to ATP-competitive inhibitors. Haematologica 96:845–853. https://doi.org/10.3324/haematol.2010.036350
Li F, Li W, Liu Y, Tong YX, Zhou P, Wang L, Chen C, Zeng LY, Wu QY, Wang XY, Xu KL (2015) Effects of the I682F mutation on JAK2’s activity, structure and stability. Int J Biol Macromol 79:118–125. https://doi.org/10.1016/j.ijbiomac.2015.04.063
Li F, Guo HY, Wang M, Geng HL, Bian MR, Cao J, Chen C, Zeng LY, Wang XY, Wu QY (2013) The effects of R683S (G) genetic mutations on the JAK2 activity, structure and stability. Int J Biol Macromol 60:186–195. https://doi.org/10.1016/j.ijbiomac.2013.05.029
Lahera A, Lopez-Nieva P, Alarcon H, Marin-Rubio JL, Cobos-Fernandez MA, Fernandez-Navarro P, Fernandez AF, Vela-Martin L, Sastre I, Ruiz-Garcia S, Llamas P, Lopez-Lorenzo JL, Cornago J, Santos J, Fernandez-Piqueras J, Villa-Morales M (2023) SOCS3 deregulation contributes to aberrant activation of the JAK/STAT pathway in precursor T-cell neoplasms. Br J Haematol. https://doi.org/10.1111/bjh.18694
Flex E, Petrangeli V, Stella L, Chiaretti S, Hornakova T, Knoops L, Ariola C, Fodale V, Clappier E, Paoloni F, Martinelli S, Fragale A, Sanchez M, Tavolaro S, Messina M, Cazzaniga G, Camera A, Pizzolo G, Tornesello A, Vignetti M, Battistini A, Cave H, Gelb BD, Renauld JC, Biondi A, Constantinescu SN, Foa R, Tartaglia M (2008) Somatically acquired JAK1 mutations in adult acute lymphoblastic leukemia. J Exp Med 205:751–758. https://doi.org/10.1084/jem.20072182
Porcu M, Gielen O, Cools J, De Keersmaecker K (2009) JAK1 mutation analysis in T-cell acute lymphoblastic leukemia cell lines. Haematologica 94:435–437. https://doi.org/10.3324/haematol.13587
Chen IM, Harvey RC, Mullighan CG, Gastier-Foster J, Wharton W, Kang H, Borowitz MJ, Camitta BM, Carroll AJ, Devidas M, Pullen DJ, Payne-Turner D, Tasian SK, Reshmi S, Cottrell CE, Reaman GH, Bowman WP, Carroll WL, Loh ML, Winick NJ, Hunger SP, Willman CL (2012) Outcome modeling with CRLF2, IKZF1, JAK, and minimal residual disease in pediatric acute lymphoblastic leukemia: a Children’s Oncology Group study. Blood 119:3512–3522. https://doi.org/10.1182/blood-2011-11-394221
Herold T, Schneider S, Metzeler KH, Neumann M, Hartmann L, Roberts KG, Konstandin NP, Greif PA, Braundl K, Ksienzyk B, Huk N, Schneider I, Zellmeier E, Jurinovic V, Mansmann U, Hiddemann W, Mullighan CG, Bohlander SK, Spiekermann K, Hoelzer D, Bruggemann M, Baldus CD, Dreyling M, Gokbuget N (2017) Adults with Philadelphia chromosome-like acute lymphoblastic leukemia frequently have IGH-CRLF2 and JAK2 mutations, persistence of minimal residual disease and poor prognosis. Haematologica 102:130–138. https://doi.org/10.3324/haematol.2015.136366
Kleppe M, Soulier J, Asnafi V, Mentens N, Hornakova T, Knoops L, Constantinescu S, Sigaux F, Meijerink JP, Vandenberghe P, Tartaglia M, Foa R, Macintyre E, Haferlach T, Cools J (2011) PTPN2 negatively regulates oncogenic JAK1 in T-cell acute lymphoblastic leukemia. Blood 117:7090–7098. https://doi.org/10.1182/blood-2010-10-314286
Moorman AV (2016) New and emerging prognostic and predictive genetic biomarkers in B-cell precursor acute lymphoblastic leukemia. Haematologica 101:407–416. https://doi.org/10.3324/haematol.2015.141101
Hubbard SR (2017) Mechanistic insights into regulation of JAK2 tyrosine kinase. Front Endocrinol (Lausanne) 8:361. https://doi.org/10.3389/fendo.2017.00361
Steeghs EMP, Jerchel IS, de Goffau-Nobel W, Hoogkamer AQ, Boer JM, Boeree A, van de Ven C, Koudijs MJ, Besselink NJM, de Groot-Kruseman HA, Zwaan CM, Horstmann MA, Pieters R, den Boer ML (2017) JAK2 aberrations in childhood B-cell precursor acute lymphoblastic leukemia. Oncotarget 8:89923–89938. https://doi.org/10.18632/oncotarget.21027
Downes CE, McClure BJ, McDougal DP, Heatley SL, Bruning JB, Thomas D, Yeung DT, White DL (2022) JAK2 alterations in acute lymphoblastic leukemia: molecular insights for superior precision medicine strategies. Front Cell Dev Biol 10:942053. https://doi.org/10.3389/fcell.2022.942053
Norvilas R, Dirse V, Semaskeviciene R, Mickeviciute O, Gineikiene E, Stoskus M, Vaitkeviciene G, Rascon J, Griskevicius L (2021) Low incidence of ABL-class and JAK-STAT signaling pathway alterations in uniformly treated pediatric and adult B-cell acute lymphoblastic leukemia patients using MRD risk-directed approach - a population-based study. BMC Cancer 21:326. https://doi.org/10.1186/s12885-020-07781-6
Baxter EJ, Scott LM, Campbell PJ, East C, Fourouclas N, Swanton S, Vassiliou GS, Bench AJ, Boyd EM, Curtin N, Scott MA, Erber WN, Green AR, Cancer Genome P (2005) Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet 365:1054–1061. https://doi.org/10.1016/S0140-6736(05)71142-9
James C, Ugo V, Le Couedic JP, Staerk J, Delhommeau F, Lacout C, Garcon L, Raslova H, Berger R, Bennaceur-Griscelli A, Villeval JL, Constantinescu SN, Casadevall N, Vainchenker W (2005) A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature 434:1144–1148. https://doi.org/10.1038/nature03546
Kralovics R, Passamonti F, Buser AS, Teo SS, Tiedt R, Passweg JR, Tichelli A, Cazzola M, Skoda RC (2005) A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med 352:1779–1790. https://doi.org/10.1056/NEJMoa051113
Levine RL, Wadleigh M, Cools J, Ebert BL, Wernig G, Huntly BJ, Boggon TJ, Wlodarska I, Clark JJ, Moore S, Adelsperger J, Koo S, Lee JC, Gabriel S, Mercher T, D’Andrea A, Frohling S, Dohner K, Marynen P, Vandenberghe P, Mesa RA, Tefferi A, Griffin JD, Eck MJ, Sellers WR, Meyerson M, Golub TR, Lee SJ, Gilliland DG (2005) Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell 7:387–397. https://doi.org/10.1016/j.ccr.2005.03.023
Silvennoinen O, Hubbard SR (2015) Molecular insights into regulation of JAK2 in myeloproliferative neoplasms. Blood 125:3388–3392. https://doi.org/10.1182/blood-2015-01-621110
O’Connor D, Moorman AV, Wade R, Hancock J, Tan RM, Bartram J, Moppett J, Schwab C, Patrick K, Harrison CJ, Hough R, Goulden N, Vora A, Samarasinghe S (2017) Use of minimal residual disease assessment to redefine induction failure in pediatric acute lymphoblastic Leukemia. J Clin Oncol 35:660–667. https://doi.org/10.1200/JCO.2016.69.6278
Kocak U, Gursel T, Kaya Z, Aral YZ, Albayrak M, Keskin EY, Belen B, Isik M, Oner N (2012) ALL-BFM 95 treatment in Turkish children with acute lymphoblastic leukemia–experience of a single center. Pediatr Hematol Oncol 29:130–140. https://doi.org/10.3109/08880018.2011.629859
Asim M, Zaidi A, Ghafoor T, Qureshi Y (2011) Death analysis of childhood acute lymphoblastic leukaemia; experience at Shaukat Khanum Memorial Cancer Hospital and Research Centre, Pakistan. J Pak Med Assoc 61:666–670
Logan C, Koura D, Taplitz R (2020) Updates in infection risk and management in acute leukemia. Hematol Am Soc Hematol Educ Program 2020:135–139. https://doi.org/10.1182/hematology.2020000098
Inaba H, Pei D, Wolf J, Howard SC, Hayden RT, Go M, Varechtchouk O, Hahn T, Buaboonnam J, Metzger ML, Rubnitz JE, Ribeiro RC, Sandlund JT, Jeha S, Cheng C, Evans WE, Relling MV, Pui CH (2017) Infection-related complications during treatment for childhood acute lymphoblastic leukemia. Ann Oncol 28:386–392. https://doi.org/10.1093/annonc/mdw557
Graubner UB, Porzig S, Jorch N, Kolb R, Wessalowski R, Escherich G, Janka GE (2008) Impact of reduction of therapy on infectious complications in childhood acute lymphoblastic leukemia. Pediatr Blood Cancer 50:259–263. https://doi.org/10.1002/pbc.21298
Li SD, Chen YB, Li ZG, Wu RH, Qin MQ, Zhou X, Jiang J, Zhang RD, Xie J, Ma XL, Zhang R, Wang B, Wu Y, Zheng HY, Wu MY (2015) Infections during induction therapy of protocol CCLG-2008 in childhood acute lymphoblastic leukemia: a single-center experience with 256 cases in China. Chin Med J (Engl) 128:472–476. https://doi.org/10.4103/0366-6999.151085
O’Connor D, Bate J, Wade R, Clack R, Dhir S, Hough R, Vora A, Goulden N, Samarasinghe S (2014) Infection-related mortality in children with acute lymphoblastic leukemia: an analysis of infectious deaths on UKALL2003. Blood 124:1056–1061. https://doi.org/10.1182/blood-2014-03-560847
Seif F, Khoshmirsafa M, Aazami H, Mohsenzadegan M, Sedighi G, Bahar M (2017) The role of JAK-STAT signaling pathway and its regulators in the fate of T helper cells. Cell Commun Signal 15:23. https://doi.org/10.1186/s12964-017-0177-y
Morris R, Kershaw NJ, Babon JJ (2018) The molecular details of cytokine signaling via the JAK/STAT pathway. Protein Sci 27:1984–2009. https://doi.org/10.1002/pro.3519
Simkin J, Strange T, Leblanc N, Rivera JC (2021) What is a cytokine storm and should it matter to me? J Am Acad Orthop Surg 29:297–299. https://doi.org/10.5435/JAAOS-D-20-00805
Cai B, Cai JP, Luo YL, Chen C, Zhang S (2015) The specific roles of JAK/STAT signaling pathway in sepsis. Inflammation 38:1599–1608. https://doi.org/10.1007/s10753-015-0135-z
Satarker S, Tom AA, Shaji RA, Alosious A, Luvis M, Nampoothiri M (2021) JAK-STAT pathway inhibition and their implications in COVID-19 therapy. Postgrad Med 133:489–507. https://doi.org/10.1080/00325481.2020.1855921
Quintas-Cardama A, Verstovsek S (2011) New JAK2 inhibitors for myeloproliferative neoplasms. Expert Opin Investig Drugs 20:961–972. https://doi.org/10.1517/13543784.2011.579560
Mayfield JR, Czuchlewski DR, Gale JM, Matlawska-Wasowska K, Vasef MA, Nickl C, Pickett G, Ness SA, Winter SS (2017) Integration of ruxolitinib into dose-intensified therapy targeted against a novel JAK2 F694L mutation in B-precursor acute lymphoblastic leukemia. Pediatr Blood Cancer 64. https://doi.org/10.1002/pbc.26328
Tasian SK, Assad A, Hunter DS, Du Y, Loh ML (2018) A phase 2 study of ruxolitinib with chemotherapy in children with philadelphia chromosome-like acute lymphoblastic leukemia (INCB18424-269/AALL1521): dose-finding results from the part 1 safety phase. Blood 132:565
Tasian SK, Hunter DS, Chen IML, Harvey RC, Carroll AJ, Wagner E, Reshmi SC, Borowitz MJ, Wood BL, Daniel J, Davidas M, Raetz EA, Hunger SP, Assad A, Loh ML (2022) A phase 2 study of ruxolitinib with chemotherapy in children with philadelphia chromosome-like acute lymphoblastic leukemia (AALL1521/INCB18424-269): biologic characteristics and minimal residual disease response of patients with non-CRLF2-rearranged JAK pathway alterations. Blood 140:6117–6118. https://doi.org/10.1182/blood-2022-164699
Chen X, Yuan L, Zhou J, Wang F, Zhang Y, Ma X, Cao P, Fang J, Chen J, Zhou X, Wu Q, Liu M, Liu H (2022) Sustained remission after ruxolitinib and chimeric antigen receptor T-cell therapy bridged to a second allogeneic hematopoietic stem cell transplantation for relapsed Philadelphia chromosome-like B-cell precursor acute lymphoblastic leukemia with novel NPHP3-JAK2 fusion. Genes Chromosomes Cancer 61:55–58. https://doi.org/10.1002/gcc.22995
Rizzuto G, Leoncin M, Imbergamo S, Taurino D, Mico MC, Tosi M, Michelato A, Buklijas K, Spinelli O, Lussana F, Lessi F, Pizzi M, Bonaldi L, Binotto G, Rambaldi A, Gurrieri C (2022) Sequential allogeneic transplantation and ruxolitinib maintenance for a synchronous PCM1-JAK2 positive myeloid sarcoma and acute B-lymphoblastic leukemia. Clin Case Rep 10:e05212. https://doi.org/10.1002/ccr3.5212
Author information
Authors and Affiliations
Contributions
Mengze Hu carried out the studies, participated in collecting data, and drafted the manuscript. Mengze Hu and Rong Liu performed the statistical analysis and participated in its design. Lei Zhang, Juanjuan Li, Jing Cao, Dixiao Zhong, Mei Yue, and Ruihong Tang participated in data acquisition, analysis, and interpretation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This retrospective study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of the Capital Institute of Pediatrics approved this study.
Consent to participate
As a retrospective study, the requirement for informed patient consent was waived by the committee.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hu, M., Liu, R., Li, J. et al. Clinical features and prognosis of pediatric acute lymphocytic leukemia with JAK-STAT pathway genetic abnormalities: a case series. Ann Hematol 102, 2445–2457 (2023). https://doi.org/10.1007/s00277-023-05245-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05245-y