Abstract
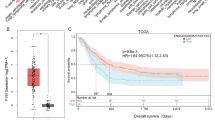
The transcription factor interferon regulatory factor 8 (IRF8), as a member of the IRF family, is essential for myeloid cell differentiation. However, the precise role of IRF8 in the pathogenesis of acute myeloid leukemia (AML) remains unknown. By using multivariate analysis, we discovered that high IRF8 expression was an independent poor predictor of overall survival (OS) in AML patients from our clinical follow-up study. The proliferation of three AML cell lines was significantly inhibited by shRNA-mediated knockdown of IRF8, owing to cell cycle S-phase arrest. Furthermore, we demonstrated that knocking down IRF8 could suppress the expression of CyclinA and CyclinB1, resulting in a shift in cell cycle distribution. Loss of IRF8 in AML cells decreased the expression of STAT3 and phosphor-STAT3 (pSTAT3), which are key factors in JAK/STAT signal pathway and are important for AML progression. Using a xenograft mouse model, we discovered the antiproliferative effect of losing IRF8 in vivo. In conclusion, this study found that IRF8 may play a prognostic factor and therapeutic target in AML.





Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Newell LF, Cook RJ (2021) Advances in acute myeloid leukemia. BMJ 375:n2026. https://doi.org/10.1136/bmj.n2026
Kirtonia A, Pandya G, Sethi G, Pandey AK, Das BC, Garg M (2020) A comprehensive review of genetic alterations and molecular targeted therapies for the implementation of personalized medicine in acute myeloid leukemia. J Mol Med (Berl) 98(8):1069–1091. https://doi.org/10.1007/s00109-020-01944-5
Infante MS, Piris MA, Hernandez-Rivas JA (2018) Molecular alterations in acute myeloid leukemia and their clinical and therapeutical implications. Med Clin (Barc) 151(9):362–367. https://doi.org/10.1016/j.medcli.2018.05.002
Kayser S, Levis MJ (2019) Clinical implications of molecular markers in acute myeloid leukemia. Eur J Haematol 102(1):20–35. https://doi.org/10.1111/ejh.13172
Estey EH (2020) Acute myeloid leukemia: 2021 update on risk-stratification and management. Am J Hematol 95(11):1368–1398. https://doi.org/10.1002/ajh.25975
Cai SF, Levine RL (2019) Genetic and epigenetic determinants of AML pathogenesis. Semin Hematol 56(2):84–89. https://doi.org/10.1053/j.seminhematol.2018.08.001
Wang H, Lee CH, Qi C, Tailor P, Feng J, Abbasi S et al (2008) IRF8 regulates B-cell lineage specification, commitment, and differentiation. Blood 112(10):4028–4038. https://doi.org/10.1182/blood-2008-01-129049
Wang H, Yan M, Sun J, Jain S, Yoshimi R, Abolfath SM et al (2014) A reporter mouse reveals lineage-specific and heterogeneous expression of IRF8 during lymphoid and myeloid cell differentiation. J Immunol 193(4):1766–1777. https://doi.org/10.4049/jimmunol.1301939
Kurotaki D, Osato N, Nishiyama A, Yamamoto M, Ban T, Sato H et al (2013) Essential role of the IRF8-KLF4 transcription factor cascade in murine monocyte differentiation. Blood 121(10):1839–1849. https://doi.org/10.1182/blood-2012-06-437863
Lee KY, Geng H, Ng KM, Yu J, van Hasselt A, Cao Y et al (2008) Epigenetic disruption of interferon-gamma response through silencing the tumor suppressor interferon regulatory factor 8 in nasopharyngeal, esophageal and multiple other carcinomas. Oncogene 27(39):5267–5276. https://doi.org/10.1038/onc.2008.147
Luo X, Xiong X, Shao Q, Xiang T, Li L, Yin X et al (2017) The tumor suppressor interferon regulatory factor 8 inhibits beta-catenin signaling in breast cancers, but is frequently silenced by promoter methylation. Oncotarget 8(30):48875–88. https://doi.org/10.18632/oncotarget.16511
Tshuikina M, Jernberg-Wiklund H, Nilsson K, Oberg F (2008) Epigenetic silencing of the interferon regulatory factor ICSBP/IRF8 in human multiple myeloma. Exp Hematol 36(12):1673–1681. https://doi.org/10.1016/j.exphem.2008.08.001
Slager SL, Achenbach SJ, Asmann YW, Camp NJ, Rabe KG, Goldin LR et al (2013) Mapping of the IRF8 gene identifies a 3’UTR variant associated with risk of chronic lymphocytic leukemia but not other common non-Hodgkin lymphoma subtypes. Cancer Epidemiol Biomarkers Prev 22(3):461–466. https://doi.org/10.1158/1055-9965.EPI-12-1217
Gaillard C, Surianarayanan S, Bentley T, Warr MR, Fitch B, Geng H et al (2018) Identification of IRF8 as a potent tumor suppressor in murine acute promyelocytic leukemia. Blood Adv 2(19):2462–2466. https://doi.org/10.1182/bloodadvances.2018018929
Xu Y, Jiang L, Fang J, Fang R, Morse HC 3rd, Ouyang G et al (2015) Loss of IRF8 Inhibits the Growth of Diffuse Large B-cell Lymphoma. J Cancer 6(10):953–961. https://doi.org/10.7150/jca.12067
Harada T, Heshmati Y, Kalfon J, Perez MW, Xavier Ferrucio J, Ewers J et al (2022) A distinct core regulatory module enforces oncogene expression in KMT2A-rearranged leukemia. Genes Dev 36(5–6):368–389. https://doi.org/10.1101/gad.349284.121
Cao Z, Budinich KA, Huang H, Ren D, Lu B, Zhang Z et al (2021) ZMYND8-regulated IRF8 transcription axis is an acute myeloid leukemia dependency. Mol Cell 81(17):3604-3622.e10. https://doi.org/10.1016/j.molcel.2021.07.018
Pogosova-Agadjanyan EL, Kopecky KJ, Ostronoff F, Appelbaum FR, Godwin J, Lee H et al (2013) The prognostic significance of IRF8 transcripts in adult patients with acute myeloid leukemia. PLoS One 8(8):e70812. https://doi.org/10.1371/journal.pone.0070812
Liss F, Frech M, Wang Y, Giel G, Fischer S, Simon C et al (2021) IRF8 is an AML-specific susceptibility factor that regulates signaling pathways and proliferation of AML cells. Cancers (Basel) 13(4). https://doi.org/10.3390/cancers13040764
Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A et al (2009) The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood 114(5):937–951. https://doi.org/10.1182/blood-2009-03-209262
Tallman MS, Wang ES, Altman JK, Appelbaum FR, Bhatt VR, Bixby D et al (2019) Acute myeloid leukemia, version 3.2019, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 17(6):721–49. https://doi.org/10.6004/jnccn.2019.0028
Liehr T (2021) International System for Human Cytogenetic or Cytogenomic Nomenclature (ISCN): some thoughts. Cytogenet Genome Res 161(5):223–224. https://doi.org/10.1159/000516654
Dohner K, Thiede C, Jahn N, Panina E, Gambietz A, Larson RA et al (2020) Impact of NPM1/FLT3-ITD genotypes defined by the 2017 European LeukemiaNet in patients with acute myeloid leukemia. Blood 135(5):371–380. https://doi.org/10.1182/blood.2019002697
Grimwade D, Jovanovic JV, Hills RK, Nugent EA, Patel Y, Flora R et al (2009) Prospective minimal residual disease monitoring to predict relapse of acute promyelocytic leukemia and to direct pre-emptive arsenic trioxide therapy. J Clin Oncol: Off J Am Soc Clin Oncol 27(22):3650–3658. https://doi.org/10.1200/JCO.2008.20.1533
Sanz MA, Fenaux P, Tallman MS, Estey EH, Lowenberg B, Naoe T et al (2019) Management of acute promyelocytic leukemia: updated recommendations from an expert panel of the European LeukemiaNet. Blood 133(15):1630–1643. https://doi.org/10.1182/blood-2019-01-894980
Porazzi P, Petruk S, Pagliaroli L, De Dominici M, Deming D 2nd, Puccetti MV et al (2022) Targeting chemotherapy to decondensed H3K27me3-marked chromatin of AML cells enhances leukemia suppression. Cancer Res 82(3):458–471. https://doi.org/10.1158/0008-5472.CAN-21-1297
Kamli H, Zaman GS, Shaikh A, Mobarki AA, Rajagopalan P (2022) A combined chemical, computational, and in vitro approach identifies SBL-105 as novel DHODH inhibitor in acute myeloid leukemia cells. Oncol Res 28(9):899–911. https://doi.org/10.3727/096504021X16281573507558
Chu X, Zhong L, Yu L, Xiong L, Li J, Dan W et al (2020) GSK-J4 induces cell cycle arrest and apoptosis via ER stress and the synergism between GSK-J4 and decitabine in acute myeloid leukemia KG-1a cells. Cancer Cell Int 20:209. https://doi.org/10.1186/s12935-020-01297-6
Joe AK, Liu H, Suzui M, Vural ME, Xiao D, Weinstein IB (2002) Resveratrol induces growth inhibition, S-phase arrest, apoptosis, and changes in biomarker expression in several human cancer cell lines. Clin Cancer Res: Off J Am Assoc Cancer Res 8(3):893–903
Grana X, Reddy EP (1995) Cell cycle control in mammalian cells: role of cyclins, cyclin dependent kinases (CDKs), growth suppressor genes and cyclin-dependent kinase inhibitors (CKIs). Oncogene 11(2):211–219
Waight JD, Netherby C, Hensen ML, Miller A, Hu Q, Liu S et al (2013) Myeloid-derived suppressor cell development is regulated by a STAT/IRF-8 axis. J Clin Investig 123(10):4464–4478. https://doi.org/10.1172/JCI68189
Biethahn S, Alves F, Wilde S, Hiddemann W, Spiekermann K (1999) Expression of granulocyte colony-stimulating factor- and granulocyte-macrophage colony-stimulating factor-associated signal transduction proteins of the JAK/STAT pathway in normal granulopoiesis and in blast cells of acute myelogenous leukemia. Exp Hematol 27(5):885–894
Stirewalt DL, Meshinchi S, Radich JP (2003) Molecular targets in acute myelogenous leukemia. Blood Rev 17(1):15–23
Rosen DB, Putta S, Covey T, Huang YW, Nolan GP, Cesano A et al (2010) Distinct patterns of DNA damage response and apoptosis correlate with Jak/Stat and PI3kinase response profiles in human acute myelogenous leukemia. PloS One 5(8):e12405. https://doi.org/10.1371/journal.pone.0012405
Benekli M, Xia Z, Donohue KA, Ford LA, Pixley LA, Baer MR et al (2002) Constitutive activity of signal transducer and activator of transcription 3 protein in acute myeloid leukemia blasts is associated with short disease-free survival. Blood 99(1):252–257
Redell MS, Ruiz MJ, Alonzo TA, Gerbing RB, Tweardy DJ (2011) Stat3 signaling in acute myeloid leukemia: ligand-dependent and -independent activation and induction of apoptosis by a novel small-molecule Stat3 inhibitor. Blood 117(21):5701–5709. https://doi.org/10.1182/blood-2010-04-280123
Fuke H, Shiraki K, Sugimoto K, Tanaka J, Beppu T, Yoneda K et al (2007) Jak inhibitor induces S phase cell-cycle arrest and augments TRAIL-induced apoptosis in human hepatocellular carcinoma cells. Biochem Biophys Res Commun 363(3):738–744. https://doi.org/10.1016/j.bbrc.2007.09.049
Shields BJ, Hauser C, Bukczynska PE, Court NW, Tiganis T (2008) DNA replication stalling attenuates tyrosine kinase signaling to suppress S phase progression. Cancer Cell 14(2):166–179. https://doi.org/10.1016/j.ccr.2008.06.003
Fukada T, Ohtani T, Yoshida Y, Shirogane T, Nishida K, Nakajima K et al (1998) STAT3 orchestrates contradictory signals in cytokine-induced G1 to S cell-cycle transition. EMBO J 17(22):6670–6677. https://doi.org/10.1093/emboj/17.22.6670
Koganti S, Hui-Yuen J, McAllister S, Gardner B, Grasser F, Palendira U et al (2014) STAT3 interrupts ATR-Chk1 signaling to allow oncovirus-mediated cell proliferation. Proc Natl Acad Sci USA 111(13):4946–4951. https://doi.org/10.1073/pnas.1400683111
Funding
This study was funded by the Zhejiang Province Traditional Chinese Medicine Science and Technology Project (2023ZL685), Natural Science Foundation of Ningbo (20221JCGY010278) and Ningbo Medical & Health Leading Academic Discipline Project (2022-S05), China.
Author information
Authors and Affiliations
Contributions
Haihui Zhuang, Fenglin Li, and Ying Lu: research design, data methodology, data interpretation, final manuscript writing, and approval. Yulian Xu, Renzhi Pei, Dong Chen, and Xuhui Liu: literature search, data integration, molecular genetic studies, and approval of the final manuscript. Peipei Ye, Jiaojiao Yuan, and Jiaying Lian: data verification, final manuscript discussion, and approval.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Research Ethics Committee of The Affiliated People’s Hospital of Ningbo University. The animal study was approved by the Research Ethics Committee of Ningbo University.
Consent to participate
Written informed consent was obtained from all individual participants included in the current study.
Consent for publication
Participants signed informed consent regarding publishing their data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Haihui Zhuang and Fenglin Li contributed equally to this work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhuang, H., Li, F., Xu, Y. et al. Loss of IRF8 inhibits the growth of acute myeloid leukemia cells. Ann Hematol 102, 1063–1072 (2023). https://doi.org/10.1007/s00277-023-05156-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-023-05156-y