Abstract
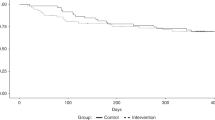
Beside many risk factors in patients considered for alloHCT, only body mass index (BMI) as a broad marker of nutritional status has prognostic value in these patients. This is the first prospective study to investigate the validity of further nutritional markers: adjusted BMI, normalized for gender and age; Subjective Global Assessment questionnaire and standardized phase angle, normalized for gender, age and BMI in 105 patients as independent risk factors for outcomes [overall survival (OS), non-relapse mortality (NRM), relapse mortality (RM), progression-free survival (PFS)] until 2 years after alloHCT. In Cox proportional-hazards regression models, we included a variety of accepted risk factors. The two most influential pre-transplant risk factors identified and associated with similarly increased hazard ratios (HR) for OS, RM, and PFS were a low-standardized phase angle (HR = 1.97, P = 0.043; HR = 3.18, P = 0.017, and HR = 1.91, P = 0.039) and advanced disease. Under- and overweight according BMI percentiles (≤10th; ≥90th) revealed associations with increased risk of NRM (HR = 2.90, P = 0.018; HR = 3.02, P = 0.062), although only low BMI was weakly associated with OS (HR = 1.82, P = 0.09). In conclusion, our results demonstrate that pre-transplant phase angle is an independent predictor for 2-year outcomes in these patients. Further investigation is necessary to demonstrate whether the theoretically modifiable phase angle can be increased by physical training combined with nutritional support, and if this improves outcome after alloHCT.


Similar content being viewed by others
References
Bearman SI, Appelbaum FR, Back A, Petersen FB, Buckner CD, Sullivan KM, Schoch HG, Fisher LD, Thomas ED (1989) Regimen-related toxicity and early posttransplant survival in patients undergoing marrow transplantation for lymphoma. J Clin Oncol 7(9):1288–1294
Bertz H, Illerhaus G, Veelken H, Finke J (2002) Allogeneic hematopoetic stem-cell transplantation for patients with relapsed or refractory lymphomas: comparison of high-dose conventional conditioning versus fludarabine-based reduced-intensity regimens. Ann Oncol 13(1):135–139
Bevans MF, Mitchell SA, Marden S (2008) The symptom experience in the first 100 days following allogeneic hematopoietic stem cell transplantation (HSCT). Support Care Cancer 16(11):1243–1254
Hansen JA, Gooley TA, Martin PJ, Appelbaum F, Chauncey TR, Clift RA, Petersdorf EW, Radich J, Sanders JE, Storb RF, Sullivan KM, Anasetti C (1998) Bone marrow transplants from unrelated donors for patients with chronic myeloid leukemia. N Engl J Med 338(14):962–968
Le Blanc K, Ringden O, Remberger M (2003) A low body mass index is correlated with poor survival after allogeneic stem cell transplantation. Haematologica 88(9):1044–1052
Lenssen P, Sherry ME, Cheney CL, Nims JW, Sullivan KM, Stern JM, Moe G, Aker SN (1990) Prevalence of nutrition-related problems among long-term survivors of allogeneic marrow transplantation. J Am Diet Assoc 90(6):835–842
Nikolousis E, Nagra S, Paneesha S, Delgado J, Holder K, Bratby L, Chaganti S, Lovell R, Milligan D (2010) Allogeneic transplant outcomes are not affected by body mass index (BMI) in patients with haematological malignancies. Ann Hematol 89(11):1141–1145
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, Storer B (2005) Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood 106(8):2912–2919
Correia MI, Waitzberg DL (2003) The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr 22(3):235–239
Gupta D, Lis CG, Dahlk SL, Vashi PG, Grutsch JF, Lammersfeld CA (2004) Bioelectrical impedance phase angle as a prognostic indicator in advanced pancreatic cancer. Br J Nutr 92(6):957–962
Horsley P, Bauer J, Gallagher B (2005) Poor nutritional status prior to peripheral blood stem cell transplantation is associated with increased length of hospital stay. Bone Marrow Transpl 35(11):1113–1116
Isenring E, Cross G, Daniels L, Kellett E, Koczwara B (2006) Validity of the malnutrition screening tool as an effective predictor of nutritional risk in oncology outpatients receiving chemotherapy. Support Care Cancer 14(11):1152–1156
Barbosa-Silva MC, Barros AJ (2005) Bioelectrical impedance analysis in clinical practice: a new perspective on its use beyond body composition equations. Curr Opin Clin Nutr Metab Care 8(3):311–317
Norman K, Stobaus N, Zocher D, Bosy-Westphal A, Szramek A, Scheufele R, Smoliner C, Pirlich M (2010) Cutoff percentiles of bioelectrical phase angle predict functionality, quality of life, and mortality in patients with cancer. Am J Clin Nutr 92(3):612–619
Faisy C, Rabbat A, Kouchakji B, Laaban JP (2000) Bioelectrical impedance analysis in estimating nutritional status and outcome of patients with chronic obstructive pulmonary disease and acute respiratory failure. Intensive Care Med 26(5):518–525
Gupta D, Lammersfeld CA, Burrows JL, Dahlk SL, Vashi PG, Grutsch JF, Hoffman S, Lis CG (2004) Bioelectrical impedance phase angle in clinical practice: implications for prognosis in advanced colorectal cancer. Am J Clin Nutr 80(6):1634–1638
Gupta D, Lammersfeld CA, Vashi PG, King J, Dahlk SL, Grutsch JF, Lis CG (2008) Bioelectrical impedance phase angle as a prognostic indicator in breast cancer. BMC Cancer 8:249
Toso S, Piccoli A, Gusella M, Menon D, Bononi A, Crepaldi G, Ferrazzi E (2000) Altered tissue electric properties in lung cancer patients as detected by bioelectric impedance vector analysis. Nutrition 16(2):120–124
Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson RA, Jeejeebhoy KN (1987) What is subjective global assessment of nutritional status? JPEN J Parenter Enteral Nutr 11(1):8–13
Detsky AS, Baker JP, Mendelson RA, Wolman SL, Wesson DE, Jeejeebhoy KN (1984) Evaluating the accuracy of nutritional assessment techniques applied to hospitalized patients: methodology and comparisons. JPEN J Parenter Enteral Nutr 8(2):153–159
Read JA, Choy ST, Beale PJ, Clarke SJ (2006) Evaluation of nutritional and inflammatory status of advanced colorectal cancer patients and its correlation with survival. Nutr Cancer 55(1):78–85
Hemmelmann C, Brose S, Vens M, Hebebrand J, Ziegler A (2010) [Percentiles of body mass index of 18-80-year-old German adults based on data from the Second National Nutrition Survey]. Dtsch Med Wochenschr 135(17):848–852
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gomez JM, Heitmann BL, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, Schols AM, Pichard C (2004) Bioelectrical impedance analysis–part I: review of principles and methods. Clin Nutr 23(5):1226–1243
Baumgartner RN, Chumlea WC, Roche AF (1988) Bioelectric impedance phase angle and body composition. Am J Clin Nutr 48(1):16–23
Fredrix EW, Saris WH, Soeters PB, Wouters EF, Kester AD, von Meyenfeldt MF, Westerterp KR (1990) Estimation of body composition by bioelectrical impedance in cancer patients. Eur J Clin Nutr 44(10):749–752
Paiva SI, Borges LR, Halpern-Silveira D, Assuncao MC, Barros AJ, Gonzalez MC (2011) Standardized phase angle from bioelectrical impedance analysis as prognostic factor for survival in patients with cancer. Support Care Cancer 19(2):187–192
Schwenk A, Beisenherz A, Romer K, Kremer G, Salzberger B, Elia M (2000) Phase angle from bioelectrical impedance analysis remains an independent predictive marker in HIV-infected patients in the era of highly active antiretroviral treatment. Am J Clin Nutr 72(2):496–501
Bosy-Westphal A, Danielzik S, Dorhofer RP, Later W, Wiese S, Muller MJ (2006) Phase angle from bioelectrical impedance analysis: population reference values by age, sex, and body mass index. JPEN J Parenter Enteral Nutr 30(4):309–316
Barbosa-Silva MC, Barros AJ, Wang J, Heymsfield SB, Pierson RN Jr (2005) Bioelectrical impedance analysis: population reference values for phase angle by age and sex. Am J Clin Nutr 82(1):49–52
Kushner RF, Schoeller DA (1986) Estimation of total body water by bioelectrical impedance analysis. Am J Clin Nutr 44(3):417–424
Lukaski HC, Johnson PE, Bolonchuk WW, Lykken GI (1985) Assessment of fat-free mass using bioelectrical impedance measurements of the human body. Am J Clin Nutr 41(4):810–817
Segal KR, Gutin B, Presta E, Wang J, Van Itallie TB (1985) Estimation of human body composition by electrical impedance methods: a comparative study. J Appl Physiol 58(5):1565–1571
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Manuel Gomez J, Lilienthal Heitmann B, Kent-Smith L, Melchior JC, Pirlich M, Scharfetter H, Schols AMWJ, Pichard C (2004) Bioelectrical impedance analysis-part II: utilization in clinical practice. Clin Nutr 23(6):1430–1453
Marks R, Potthoff K, Hahn J, Ihorst G, Bertz H, Spyridonidis A, Holler E, Finke JM (2008) Reduced-toxicity conditioning with fludarabine, BCNU, and melphalan in allogeneic hematopoietic cell transplantation: particular activity against advanced hematologic malignancies. Blood 112(2):415–425
Dittmar M (2003) Reliability and variability of bioimpedance measures in normal adults: effects of age, gender, and body mass. Am J Phys Anthropol 122(4):361–370
Evans WJ, Morley JE, Argiles J, Bales C, Baracos V, Guttridge D, Jatoi A, Kalantar-Zadeh K, Lochs H, Mantovani G, Marks D, Mitch WE, Muscaritoli M, Najand A, Ponikowski P, Rossi Fanelli F, Schambelan M, Schols A, Schuster M, Thomas D, Wolfe R, Anker SD (2008) Cachexia: a new definition. Clin Nutr 27(6):793–799
Johansen KL, Kaysen GA, Young BS, Hung AM, da Silva M, Chertow GM (2003) Longitudinal study of nutritional status, body composition, and physical function in hemodialysis patients. Am J Clin Nutr 77(4):842–846
Biolo G, Tipton KD, Klein S, Wolfe RR (1997) An abundant supply of amino acids enhances the metabolic effect of exercise on muscle protein. Am J Physiol 273(1 Pt 1):E122–E129
Esmarck B, Andersen JL, Olsen S, Richter EA, Mizuno M, Kjaer M (2001) Timing of postexercise protein intake is important for muscle hypertrophy with resistance training in elderly humans. J Physiol 535(Pt 1):301–311
Levenhagen DK, Carr C, Carlson MG, Maron DJ, Borel MJ, Flakoll PJ (2002) Postexercise protein intake enhances whole-body and leg protein accretion in humans. Med Sci Sports Exerc 34(5):828–837
Wiskemann J, Huber G (2008) Physical exercise as adjuvant therapy for patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transpl 41(4):321–329
Wiskemann J, Dreger P, Schwerdtfeger R, Bondong A, Huber G, Kleindienst N, Ulrich CM, Bohus M (2011) Effects of a partly self-administered exercise program before, during, and after allogeneic stem cell transplantation. Blood 117(9):2604–2613
Baumann FT, Zopf EM, Nykamp E, Kraut L, Schule K, Elter T, Fauser AA, Bloch W (2011) Physical activity for patients undergoing an allogeneic hematopoietic stem cell transplantation: benefits of a moderate exercise intervention. Eur J Haematol 87(2):148–156
Dickson TM, Kusnierz-Glaz CR, Blume KG, Negrin RS, Hu WW, Shizuru JA, Johnston LL, Wong RM, Stockerl-Goldstein KE (1999) Impact of admission body weight and chemotherapy dose adjustment on the outcome of autologous bone marrow transplantation. Biol Blood Marrow Transpl 5(5):299–305
Navarro WH, Loberiza FR Jr, Bajorunaite R, van Besien K, Vose JM, Lazarus HM, Rizzo JD (2006) Effect of body mass index on mortality of patients with lymphoma undergoing autologous hematopoietic cell transplantation. Biol Blood Marrow Transpl 12(5):541–551
Deeg HJ, Seidel K, Bruemmer B, Pepe MS, Appelbaum FR (1995) Impact of patient weight on non-relapse mortality after marrow transplantation. Bone Marrow Transpl 15(3):461–468
Navarro WH, Agovi MA, Logan BR, Ballen K, Bolwell BJ, Frangoul H, Gupta V, Hahn T, Ho VT, Juckett M, Lazarus HM, Litzow MR, Liesveld JL, Moreb JS, Marks DI, McCarthy PL, Pasquini MC, Rizzo JD (2010) Obesity does not preclude safe and effective myeloablative hematopoietic cell transplantation (HCT) for acute myelogenous leukemia (AML) in adults. Biol Blood Marrow Transpl 16(10):1442–1450
Hadjibabaie M, Iravani M, Taghizadeh M, Ataie-Jafari A, Shamshiri AR, Mousavi SA, Alimoghaddam K, Hosseini S, Ghavamzadeh A (2008) Evaluation of nutritional status in patients undergoing hematopoietic SCT. Bone Marrow Transpl 42(7):469–473
Fleming DR, Rayens MK, Garrison J (1997) Impact of obesity on allogeneic stem cell transplant patients: a matched case-controlled study. Am J Med 102(3):265–268
Blouin RA, Warren GW (1999) Pharmacokinetic considerations in obesity. J Pharm Sci 88(1):1–7
Hanley MJ, Abernethy DR, Greenblatt DJ (2010) Effect of obesity on the pharmacokinetics of drugs in humans. Clin Pharmacokinet 49(2):71–87
Jain R, Chung SM, Jain L, Khurana M, Lau SW, Lee JE, Vaidyanathan J, Zadezensky I, Choe S, Sahajwalla CG (2011) Implications of obesity for drug therapy: limitations and challenges. Clin Pharmacol Ther 90(1):77–89
Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH (1999) The disease burden associated with overweight and obesity. JAMA 282(16):1523–1529
Caraco Y, Zylber-Katz E, Berry EM, Levy M (1995) Antipyrine disposition in obesity: evidence for negligible effect of obesity on hepatic oxidative metabolism. Eur J Clin Pharmacol 47(6):525–530
Hingorani P, Seidel K, Krailo M, Mascarenhas L, Meyers P, Marina N, Conrad EU, Hawkins DS (2011) Body mass index (BMI) at diagnosis is associated with surgical wound complications in patients with localized osteosarcoma: a report from the Children's Oncology Group. Pediatr Blood Cancer 57(6):939–942
Scrimshaw NS, SanGiovanni JP (1997) Synergism of nutrition, infection, and immunity: an overview. Am J Clin Nutr 66(2):464S–477S
Bozzetti F, Gianotti L, Braga M, Di Carlo V, Mariani L (2007) Postoperative complications in gastrointestinal cancer patients: the joint role of the nutritional status and the nutritional support. Clin Nutr 26(6):698–709
Paiva SI, Borges LR, Halpern-Silveira D, Assunção MC, Barros AJ, Gonzalez MC (2010) Standardized phase angle from bioelectrical impedance analysis as prognostic factor for survival in patients with cancer. Support Care Cancer 19(2):187–192
Acknowledgments
We are grateful to Carole Cuerten for proofreading this manuscript. P. Urbain was supported by a PhD grant from the National Research Fund, Luxemburg.
Conflict of interst
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Urbain, P., Birlinger, J., Ihorst, G. et al. Body mass index and bioelectrical impedance phase angle as potentially modifiable nutritional markers are independent risk factors for outcome in allogeneic hematopoietic cell transplantation. Ann Hematol 92, 111–119 (2013). https://doi.org/10.1007/s00277-012-1573-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-012-1573-4