Abstract
Purpose
The purpose of this study was to evaluate the ability of MRI images to reveal foraminal ligaments at levels L1–L5 by comparing the results with those of anatomical studies.
Methods
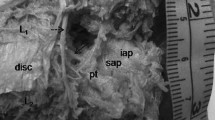
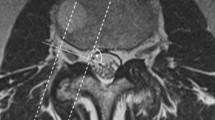
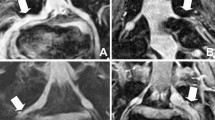
Eighty lumbar foramina were studied. First, the best MRI scanning parameters were selected, and the transverse and sagittal axes of each lumbar foramina were scanned to identify and record the ligament-like structures in each lumbar foramen. Then, the cadaveric specimens were anatomically studied, and all ligament structures in the lumbar foramina were retained. The number, morphology and distribution of ligaments under anatomical and MRI scanning were observed. Histological staining of the dissected ligament structures was performed to confirm that they were ligamentous tissues. Finally, the accuracy of ligament recognition in MRI images was statistically analyzed.
Results
A total of 233 foraminal ligaments were identified in 80 lumbar intervertebral foramina through cadaveric anatomy. The radiating ligaments (176, 75.5%) were found to be attached from the nerve root to the surrounding osseous structures, while the transforaminal ligaments (57, 24.5%) traversed the intervertebral foramina without any connection to the nerve roots. A total of 42 transforaminal ligament signals and 100 radiating ligament signals were detected in the MRI images of the 80 intervertebral foramina.
Conclusion
The MRI can identify the lumbar foraminal ligament, and the recognition rate of the transforaminal ligament is higher than that of the radiating ligament. This study provides a new method for the clinical diagnosis of the relationship between the lumbar foraminal ligament and radicular pain.







Similar content being viewed by others
Data availability
Data is available for reviewing upon request.
References
Amonoo-Kuofi HS, el-Badawi MG, Fatani JA (1988) Ligaments associated with lumbar intervertebral foramina 1. L1 to L4. J Anat 156:177–183
Arslan M, Açar Hİ, Cömert A (2017) Cervical extraforaminal ligaments: an anatomical study. Surg Radiol Anat 39(12):1377–1383. https://doi.org/10.1007/s00276-017-1896-x
Cinotti G, De Santis P, Nofroni I, Postacchini F (2002) Stenosis of lumbar intervertebral foramen: anatomic study on predisposing factors. Spine (Phila Pa 1976) 27(3):223–229. https://doi.org/10.1097/00007632-200202010-00002
Cramer GD, Skogsbergh DR, Bakkum BW, Winterstein JF, Yu S, Tuck NR Jr (2002) Evaluation of transforaminal ligaments by magnetic resonance imaging. J Manipulative Physiol Ther 25(4):199–208. https://doi.org/10.1067/mmt.2002.123174
Golub BS, Silverman B (1969) Transforaminal ligaments of the lumbar spine. J Bone Joint Surg Am 51(5):947–956
Grimes PF, Massie JB, Garfin SR (2000) Anatomic and biomechanical analysis of the lower lumbar foraminal ligaments. Spine (Phila Pa 1976) 25(16):2009–2014. https://doi.org/10.1097/00007632-200008150-00002
Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, Woolf A, Vos T, Buchbinder R (2012) A systematic review of the global prevalence of low back pain. Arthritis Rheum 64(6):2028–2037. https://doi.org/10.1002/art.34347
Kraan GA, Delwel EJ, Hoogland PV, van der Veen MR, Wuisman PI, Stoeckart R, Kleinrensink GJ, Snijders CJ (2005) Extraforaminal ligament attachments of human lumbar nerves. Spine (Phila Pa 1976) 30(6):601–605. https://doi.org/10.1097/01.brs.0000155403.85582.39
Kunogi J, Hasue M (1991) Diagnosis and operative treatment of intraforaminal and extraforaminal nerve root compression. Spine (Phila Pa 1976) 16(11):1312–1320. https://doi.org/10.1097/00007632-199111000-00012
Li J, Shi B, Qiu S, Ding Z, Wang L (2017) A controlled study on the anatomy of cervical extraforaminal ligaments and three-dimensional fast-imaging employing a steady-state acquisition sequence. Eur Spine J 26(4):1039–1046. https://doi.org/10.1007/s00586-016-4823-7
Maher C, Underwood M, Buchbinder R (2017) Non-specific low back pain. Lancet 389(10070):736–747. https://doi.org/10.1016/S0140-6736(16)30970-9
Marić DL, Krstonošić B, Erić M, Marić DM (2015) An anatomical study of the lumbar external foraminal ligaments: appearance at MR imaging. Surg Radiol Anat 37(1):87–91. https://doi.org/10.1007/s00276-014-1320-8
Min JH, Kang SH, Lee JB, Cho TH, Suh JG (2005) Anatomic analysis of the transforaminal ligament in the lumbar intervertebral foramen. Neurosurgery 57(1 Suppl):37–41. https://doi.org/10.1227/01.neu.0000163481.58673.1a
Nowicki BH, Haughton VM (1992) Neural foraminal ligaments of the lumbar spine: appearance at CT and MR imaging. Radiology 183(1):257–264. https://doi.org/10.1148/radiology.183.1.1549683
Park HK, Rudrappa S, Dujovny M, Diaz FG (2001) Intervertebral foraminal ligaments of the lumbar spine: anatomy and biomechanics. Childs Nerv Syst 17(4–5):275–282. https://doi.org/10.1007/pl00013729
Qian Y, Qin A, Zheng MH (2011) Transforaminal ligament may play a role in lumbar nerve root compression of foraminal stenosis. Med Hypotheses 77(6):1148–1149. https://doi.org/10.1016/j.mehy.2011.09.025
Rydevik B, Brown MD, Lundborg G (1984) Pathoanatomy and pathophysiology of nerve root compression. Spine (Phila Pa 1976) 9(1):7–15. https://doi.org/10.1097/00007632-198401000-00004
Shi B, Zheng X, Zhang H, Sun C, Cao Y, Jin A, Ding Z (2015) The morphology and clinical significance of the extraforaminal ligaments at the cervical level. Spine (Phila Pa 1976) 40(1):E9-17. https://doi.org/10.1097/BRS.0000000000000668
Transfeldt EE, Robertson D, Bradford DS (1993) Ligaments of the lumbosacral spine and their role in possible extraforaminal spinal nerve entrapment and tethering. J Spinal Disord 6(6):507–512. https://doi.org/10.1097/00002517-199306060-00006
Vanderlinden RG (1984) Subarticular entrapment of the dorsal root ganglion as a cause of sciatic pain. Spine (Phila Pa 1976) 9(1):19–22. https://doi.org/10.1097/00007632-198401000-00006
Zhao Q, Zhang W, Su Z, Wang M, Yang L, Zhong E, Ding Z, Li Q, Lu H (2018) The morphology and clinical significance of the extraforaminal ligaments at the T1–T12 levels. Spine 43(21):E1241–E1248. https://doi.org/10.1097/BRS.0000000000002675
Zhao Q, Zhong E, Shi B, Li Y, Sun C, Ding Z (2016) The morphology and clinical significance of the intraforaminal ligaments at the L5–S1 levels. Spine J 16(8):1001–1006. https://doi.org/10.1016/j.spinee.2016.03.048
Zhong E, Zhao Q, Shi B, Xie Y, Ding Z, Lv H, Zhong S, Huang W (2018) The morphology and possible clinical significance of the intraforaminal ligaments in the entrance zones of the L1–L5 levels. Pain Physician 21(2):E157–E165
Zhong E, Zhao Q, Shi B, Zheng X, Zhao Q, Tan J, Ding Z, Huang W (2017) Morphology and possible clinical significance of the radiating extraforaminal ligaments at the L1–L5 Levels. Spine (Phila Pa 1976) 42(18):1355–1361. https://doi.org/10.1097/BRS.0000000000002120
Acknowledgements
The authors thank their families for their support of this study and the contributors of human specimens.
Funding
This study has been supported by grants from the Foundation for Basic and Applied Basic Research of Guangzhou (Grant No. 202201011203), Foundation for Basic and Applied Basic Research of Guangzhou (Grant No.SL2022A04J01494) and National Natural Science Foundation of China (Grant No.32200946).
Author information
Authors and Affiliations
Contributions
QH Zhao and QC Li: project development. EY Zhong and QH Zhao: data collection or management, manuscript writing/editing. CH Fan: data analysis.
Corresponding author
Ethics declarations
Conflict of interests
There is no potential conflict of interest-associated biases in the text of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhong, E., Fan, C., Li, Q. et al. A comparative study of the anatomy and MRI images of the lumbar foraminal ligaments at the L1–L5 levels. Surg Radiol Anat 45, 1535–1543 (2023). https://doi.org/10.1007/s00276-023-03251-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-023-03251-3