Abstract
Purpose
Management of stroke secondary to septic emboli (SE) remains challenging, due to both the lack of specific recommendations and the gravity of the underlying pathology.The aim of this study is to describe the presence of SE in a series of mechanical thrombectomies (MT), analyzing technical complexity and outcomes with respect to the patients by means of histological analysis and microbiological study of the clot.
Methods
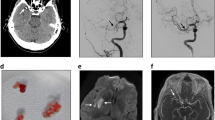
All the retrieved clots were studied under an established protocol, including histopathological and bacteriological study with hematoxylin–eosin, Gram and Gomori trichrome staining.Technical complexity in SE with respect to the series was evaluated by analyzing time of the procedures, number of passes and use of intracranial definitive stents.
Results
Over a 24-month period, bacteria were detected in the retrieved clot of four out of 65 patients (incidence 6.2%). Two cases were eventually diagnosed with infective endocarditis, while the remaining two were diagnosed with urinary tract infection and respiratory septicemia, respectively. Three of the four patients (75%) required an intracranial definitive stent in order to achieve successful recanalization.These procedures were significantly longer (137.7 vs. 59.8 min, p < 0.001), needed a higher number of passes (5.8 vs. 2.2, p < 0.001), and delivery of an intracranial stent more frequently (75% vs. 1.6%, p = 0.008), with respect to the rest of the series.
Conclusions
In our series, systematic histopathological and bacteriological study of the MT samples allowed a higher proportion of SE diagnosis in comparison with previous reports.






Similar content being viewed by others
References
Esenwa CC, Elkind MS. Inflammatory risk factors, biomarkers and associated therapy in ischaemic stroke. Nat Rev Neurol. 2016;12:594–604.
Grau AJ, Urbanek C, Palm F. Common infections and the risk of stroke. Nat Rev Neurol. 2010;6:681–94.
Derex L, Bonnefoy E, Delahaye F. Impact of stroke on therapeutic decision making in infective endocarditis. J Neurol. 2010;257:315–21.
Toni D, Sacco RL, Brainin M, et al. In: Mohr JP, Wolf PA, Grotta JC, et al. Stroke–Pathophysiology, Diagnosis, and Management. 5th ed. Elsevier Saunders; Philadelphia: Classification of Ischemic Stroke. 2011;293–306.
Kim JM, Jeon JS, Kim YW, Kang DH, Hwang YH, Kim YS. Forced arterial suction thrombectomy of septic embolic middle cerebral artery occlusion due to infective endocarditis: an illustrative case and review of the literature. Neurointervention. 2014;9:101–5.
Sveinsson O, Herrman L, Holmin S. Intra-arterial mechanical thrombectomy: an effective treatment for ischemic stroke caused by endocarditis. Case Rep Neurol. 2016;8:229–33.
Toeg HD, Al-Atassi T, Kalidindi N, Iancu D, Zamani D, Giaccone R, et al. Endovascular treatment for cerebral septic embolic stroke. J Stroke Cerebrovasc Dis. 2014;23:375–7.
Bendok BR, Arnaout O. Intracranial retrievable stenting for septic emboli. World Neurosurg. 2012;77:470–1.
Kang G, Yang TK, Choi JH, Heo ST. Effectiveness of mechanical embolectomy for septic embolus in the cerebral artery complicated with infective endocarditis. J Korean Med Sci. 2013;28:1244–7.
Salinas P, Moreno R, Frutos R, Lopez-Sendon JL. Neurovascular rescue for thrombus-related embolic stroke during transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2013;6:981–2.
Bain MD, Hussain MS, Gonugunta V, Katzan I, Gupta R. Successful recanalization of a septic embolus with a balloon mounted stent after failed mechanical thrombectomy. J Neuroimaging. 2011;21:170–2.
Kan P, Webb S, Siddiqui AH, Levy EI. First reported use of retrievable stent technology for removal of a large septic embolus in the middle cerebral artery. World Neurosurg. 2012;77(3):591.e1-5.
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of org 10172 in acute stroke treatment. Stroke. 1993;24:35–41.
Alonso de Leciñana M, Egido JA, Casado I, Ribó M, Dávalos A, Masjuan J, et al. Guidelines for the treatment of acute ischaemic stroke. Neurologia. 2014;29:102–22.
Asaithambi G, Adil MM, Qureshi AI. Thrombolysis for ischemic stroke associated with infective endocarditis: results from the nationwide inpatient sample. Stroke. 2013;44:2917–9.
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriver thrombectomy after intravenous t-PA vs. t-PA alone in stroke. NEJM. 2015;372:2285–95.
Brownlee WJ, Anderson NE, Barber PA. Intravenous thrombolysis is unsafe in stroke due to infective endocarditis. Intern Med J. 2014;44:195–7.
Ladner TR, Davis BJ, He L, Kirshner HS, Froehler MT, Mocco J. Complex decision-making in stroke: preoperative mechanical thrombectomy of septic embolus for emergency cardiac valve surgery. J Neurointerv Surg. 2015;7:e41.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest.
Ethical Standard
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Hernández-Fernández, F., Rojas-Bartolomé, L., García-García, J. et al. Histopathological and Bacteriological Analysis of Thrombus Material Extracted During Mechanical Thrombectomy in Acute Stroke Patients. Cardiovasc Intervent Radiol 40, 1851–1860 (2017). https://doi.org/10.1007/s00270-017-1718-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-017-1718-x