Abstract
Purpose
Implanted venous access devices (IVADs) are often used in patients who require long-term intravenous drug administration. The most common causes of device dysfunction include occlusion by fibrin sheath and/or catheter adherence to the vessel wall. We present percutaneous endovascular salvage techniques to restore function in occluded catheters. The aim of this study was to evaluate the feasibility, safety, and efficacy of these techniques.
Methods and Materials
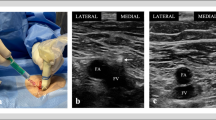
Through a femoral or brachial venous access, a snare is used to remove fibrin sheath around the IVAD catheter tip. If device dysfunction is caused by catheter adherences to the vessel wall, a new “mechanical adhesiolysis” maneuver was performed. IVAD salvage procedures performed between 2005 and 2013 were analyzed. Data included clinical background, catheter tip position, success rate, recurrence, and rate of complication.
Results
Eighty-eight salvage procedures were performed in 80 patients, mostly women (52.5 %), with a mean age of 54 years. Only a minority (17.5 %) of evaluated catheters were located at an optimal position (i.e., cavoatrial junction ±1 cm). Mechanical adhesiolysis or other additional maneuvers were used in 21 cases (24 %). Overall technical success rate was 93.2 %. Malposition and/or vessel wall adherences were the main cause of technical failure. No complications were noted.
Conclusion
These IVAD salvage techniques are safe and efficient. When a catheter is adherent to the vessel wall, mechanical adhesiolysis maneuvers allow catheter mobilization and a greater success rate with no additional risk. In patients who still require long-term use of their IVAD, these procedures can be performed safely to avoid catheter replacement.






Similar content being viewed by others
References
Yeste Sanchez L, Galbis Caravajal JM, Fuster Diana CA, Moledo Eiras E (2006) Protocol for the implantation of a venous access device (Port-A-Cath System). The complications and solutions found in 560 cases. Clin Transl Oncol 8(10):735–741
Walser EM (2012) Venous access ports: Indications, implantation technique, follow-up, and complications. Cardiovasc Intervent Radiol 35(4):751–764
Bassi KK, Giri AK, Pattanayak M, Abraham SW, Pandey KK (2012) Totally implantable venous access ports: Retrospective review of long-term complications in 81 patients. Indian J Cancer 49(1):114–118
Baskin JL, Pui CH, Reiss U, Wilimas JA, Metzger ML, Ribeiro RC et al (2009) Management of occlusion and thrombosis associated with long-term indwelling central venous catheters. Lancet 374(9684):159–169
Vardy J, Engelhardt K, Cox K, Jacquet J, McDade A, Boyer M et al (2004) Long-term outcome of radiological-guided insertion of implanted central venous access port devices (CVAPD) for the delivery of chemotherapy in cancer patients: institutional experience and review of the literature. Br J Cancer 91:1045
Stevens B, Barton SE, Brechbill M, Moenter S, Lou Piel A, Shankle D (2000) A randomized, prospective trial of conventional vascular ports vs. the vortex “clear-flow” reservoir port in adult oncology patients. J Vasc Access Devices 5(2):37–44
Gray RJ, Levitin A, Buck D, Brown LC, Sparling YH, Jablonski KA et al (2000) Percutaneous fibrin sheath stripping versus transcatheter urokinase infusion for malfunctioning well-positioned tunneled central venous dialysis catheters: a prospective, randomized trial. J Vasc Interv Radiol 11(9):1121–1129
Crain MR, Mewissen MW, Ostrowski GJ, Paz-Fumagalli R, Beres RA, Wertz RA (1996) Fibrin sleeve stripping for salvage of failing hemodialysis catheters: technique and initial results. Radiology 198(1):41–44
Heye S, Maleux G, Goossens GA, Vaninbroukx J, Jerome M, Stas M (2012) Feasibility and safety of endovascular stripping of totally implantable venous access devices. Cardiovasc Intervent Radiol 35(3):607–612
Qanadli SD, Mesurolle B, Sissakian JF, Chagnon S, Lacombe P (2000) Implanted central venous catheter-related acute superior vena cava syndrome: management by metallic stent and endovascular repositioning of the catheter tip. Eur Radiol 10(8):1329–1331
Sacks D, McClenny TE, Cardella JF, Lewis CA (2003) Society of interventional radiology clinical practice guidelines. J Vasc Interv Radiol 14(9 Pt 2):S199–S1202
Bessoud B, de Baere T, Kuoch V, Desruennes E, Cosset MF, Lassau N et al (2003) Experience at a single institution with endovascular treatment of mechanical complications caused by implanted central venous access devices in pediatric and adult patients. AJR Am J Roentgenol 180(2):527–532
Reddy AS, Lang EV, Cutts J, Loh S, Rosen MP (2007) Fibrin sheath removal from central venous catheters: an internal snare manoeuvre. Nephrol Dial Transplant 22(6):1762–1765
Caers J, Fontaine C, Vinh-Hung V, De Mey J, Ponnet G, Oost C et al (2005) Catheter tip position as a risk factor for thrombosis associated with the use of subcutaneous infusion ports. Support Care Cancer 13(5):325–331
Cohn DE, Mutch DG, Rader JS, Farrell M, Awantang R, Herzog TJ (2001) Factors predicting subcutaneous implanted central venous port function: the relationship between catheter tip location and port failure in patients with gynecologic malignancies. Gynecol Oncol 83(3):533–536
Schutz JC, Patel AA, Clark TW, Solomon JA, Freiman DB, Tuite CM et al (2004) Relationship between chest port catheter tip position and port malfunction after interventional radiologic placement. J Vasc Interv Radiol 15(6):581–587
Kuter DJ (2004) Thrombotic complications of central venous catheters in cancer patients. Oncologist 9(2):207–216
Nayeemuddin M, Pherwani AD, Asquith JR (2013) Imaging and management of complications of central venous catheters. Clin Radiol 68(5):529–544
Funaki B, Szymski GX, Hackworth CA, Rosenblum JD, Burke R, Chang T et al (1997) Radiologic placement of subcutaneous infusion chest ports for long-term central venous access. AJR Am J Roentgenol 169(5):1431–1434
Watorek E, Golebiowski T, Letachowicz K, Garcarek J, Kurcz J, Bartosik HA et al (2012) Balloon angioplasty for disruption of tunneled dialysis catheter fibrin sheath. J Vasc Access 13(1):111–114
Janne d’Othee B, Tham JC, Sheiman RG (2006) Restoration of patency in failing tunneled hemodialysis catheters: a comparison of catheter exchange, exchange and balloon disruption of the fibrin sheath, and femoral stripping. J Vasc Interv Radiol 17(6):1011–1015
Besarab A, Pandey R (2011) Catheter management in hemodialysis patients: delivering adequate flow. Clin J Am Soc Nephrol 6(1):227–234
Oliver MJ, Mendelssohn DC, Quinn RR, Richardson EP, Rajan DK, Pugash RA et al (2007) Catheter patency and function after catheter sheath disruption: a pilot study. Clin J Am Soc Nephrol 2(6):1201–1206
Sobolevsky S, Sheiman RG, Faintuch S, Perry L (2007) Femoral-to-port through-and-through wire access to reestablish subcutaneous port function. AJR Am J Roentgenol 188(4):1047–1049
Brismar B, Hardstedt C, Jacobson S (1981) Diagnosis of thrombosis by catheter phlebography after prolonged central venous catheterization. Ann Surg 194(6):779–783
Winn MP, McDermott VG, Schwab SJ, Conlon PJ (1997) Dialysis catheter ‘fibrin-sheath stripping’: a cautionary tale! Nephrol Dial Transpl 12(5):1048–1050
Rockoff MA, Gang DL, Vacanti JP (1984) Fatal pulmonary embolism following removal of a central venous catheter. J Pediatr Surg 19(3):307–309
Conflict of Interest
Stéphane Breault, Frédéric Glauser, Malik Babaker, and Francesco Doenz have no conflict of interest. Salah Dine Qanadli was consultant for Cook Medical Inc. and Cordis Corporation in the last 3 years.
Statement of Informed Consent
For this type of study, formal consent is not required.
Statement of Human and Animal Rights
This does not apply to this type of study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Breault, S., Glauser, F., Babaker, M. et al. Percutaneous Endovascular Salvage Techniques for Implanted Venous Access Device Dysfunction. Cardiovasc Intervent Radiol 38, 642–650 (2015). https://doi.org/10.1007/s00270-014-0968-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-014-0968-0