Abstract
Background
Although there is a rationale supporting that preoperative showering with 2% or 4% chlorhexidine gluconate (CHG) would decrease skin bacterial colonization, there is no consensus that this practice reduces the risk of surgical site infection (SSI).
Objectives
Analyze the skin concentration of CHG after preoperative showering associated with the traditional skin preparation with CHG 4% for breast surgery.
Methods
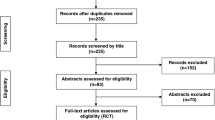
Randomized controlled trial that included 45 patients, all candidates for augmentation mammaplasty, allocated into three groups (A: no preoperative showering; B: one preoperative showering; C: two preoperative showering with CHG 4%) in a 1:1:1 ratio. Skin swabs collection was performed right before the surgical incision. The samples were, then, sent to spectrophotometry in order to determine the skin concentration of CHG at the beginning of surgery.
Results
The age ranged from 18 to 61 years, with a mean of 37 years old. Group C had the lowest median concentration (0.057) followed by group B (0.060) and group A (0.072), however, with no statistical significance. The areola was the place with the lowest median concentration level (0.045), followed by the axilla (0.061) and the inframammary fold (IMF) (0.069). Still, when comparing the distribution of the sites, a statistically significant difference was found only between the axilla and the areola (p = 0.022).
Conclusion
Preoperative showering with CHG 4% did not increase the concentration of this agent on the skin surface right before the surgical incision.
Level of evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
References
Veiga DF, Damasceno CA, Filho VJ et al (2008) Influence of povidone-iodine preoperative showers on skin colonization in elective plastic surgery procedures. Plast Reconstr Surg 121(1):115–8
Edmiston CE (1993) Prosthetic device infections in surgery. In: Nichols RL, Nyhus LM (eds) Update surgical sepsis. J.B. Lippincott Co, Philadelphia
Virden CP, Dobke MK, Stein P et al (1992) Subclinical infection of the silicone breast implant surface as a possible cause of capsular contracture. Aesthetic Plast Surg 16(2):173–179
Pajkos A, Deva AK, Vickery K et al (2003) Detection of subclinical infection in significant breast implant capsules. Plast Reconstr Surg 111(5):1605–1611
Dobke MK, Svahn JK, Vastine VL et al (1995) Characterization of microbial presence at the surface of silicone mammary implants. Ann Plast Surg 34(6):563–569
Mangram AJ, Horan TC, Pearson ML et al (1999) The hospital infection control practice advisory committee, guidelines for the prevention of surgical site infections. Am J Infect Control 27(2):97–132
Edmiston CE, Seabrook GR, Johnson CP et al (2007) Comparative of a new and innovative 2% chlorhexidine gluconate-impregnated cloth with 4% chlorhexidine gluconate as a topical antiseptic for preparation of the skin prior to surgery. Am J Infect Control 35(2):89–96
Rosenberg A, Alatary SD, Peterson AF (1978) Safety and efficacy of antiseptic chlorhexidine gluconate. Surg Gynecol Obstet 143(5):789–792
Ostrander RV, Botte MJ, Brage ME (2005) Efficacy of surgical preparation solution in foot and ankle surgery. J Bone Joint Surg 87(5):980–985
Saltzman MD, Nuber GW, Gryzlo SM et al (2009) Efficacy of surgical preparations in shoulder surgery. J Bone Joint Surg 91:1949–1953
Culligan PJ, Kubik K, Murphy M et al (2005) A randomized trial that compared povidone iodine and chlorhexifine as antiseptics for vaginal hysterectomy. Obstet Gynecol 192:422–425
Savage JW, Weatherford BM, Sugrue PA et al (2012) Efficacy of surgical preparation solution in lumbar surgery. J Bone Joint Surg 94:490–494
Holder C, Zellinger M (2009) Daily bathing with chlorhexidine in the ICU to prevent central line associated infections. J Clin Outcome Manage. 16:509–513
Paulson DS (1993) Efficacy evaluation of a 4% chlorhexidine gluconate as a full-body shower wash. Am J Infect Control 21:205–209
Ferraz ÁAB, Vasconcelos CFM, Santa-Cruz F et al (2019) Surgical site infection in bariatric surgery: results of a care bundle. Rev Col Bras Cir 46(4):e2252
Prabhu AS, Krpata DM, Phillips S et al (2017) Preoperative chlorhexidine gluconate use can increase risk for surgical site infections after ventral hernia repair. J Am Coll Surg 224(3):334–340
Edmiston CE, Krepel CJ, Seabrook GR et al (2008) Preoperative shower revisited: can high topical antiseptic levels be achieved on the skin surface before surgical admission. J Am Coll Surg 207:233–239
Tamboto H, Vickery K, Deva AK (2010) Subclinical (biofilm) infection causes capsular contracture in porcine model following augmentation mammaplasty. Plast Reconstr Surg 126:835–842
Hu H, Johani K, Almatroudi A et al (2016) Bacterial biofilm infection detectedin breast implant-associated anaplastic large cell lymphoma. Plast Reconstr Surg 137(6):1659–1669
Jacombs A, Tahir S, Hu H et al (2014) In vitro and in vivo investigation of the influence of implant surface on the formation of bacterial biofilm in mammary implants. Plast Reconstr Surg 133:471e-e480
Rieger UM, Mesina J, Kalbermatten DF et al (2013) Bacterial biofilms and capsular contracture in patients with breast implants. Br J Surg 100(6):768–774
Edmiston CE Jr, Lee CJ, Krepel CJ et al (2015) Evidence for a standardized preadmission showering regimen to achieve maximal antiseptic skin surface concentrations of chlorhexidine gluconate 4% in surgical patients. JAMA Surg 150(11):1027–1033
Chlebicki MJP, Safdar N, O’Horo JC, Maki DG (2013) Preoperative chlorhexidine shower or bath for prevention of surgical site infection. Am J Infect Control 41(2):167–173
Webster J, Osborne S (2015) Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev 20(2):CD0044985
Veiga DF, Damasceno CA, Veiga-Filho J et al (2009) Randomized controlled trial of the effectiveness of chlorhexidine showers before elective plastic surgical procedures. Infect Control Hosp Epidemiol 30(1):77–79
Wiener TC (2008) Relationship of incision choice to capsular contracture. Aesth Plat Surg. 32:303–330
Berrios-Torres SI, Umscheid CA, Bratzler DW et al (2017) Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg 152(8):784–791
Allegranzi B, Zayed B, Bischoff P et al (2016) New WHO recommendations on intraoperative and postoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis 16(12):e288–e303
Makhni M, Jegede K, Lombardi J et al (2018) No clear benefit of chlorhexidine use at home before surgical preparation. J Am Acad Orthop Surg 26(2):e39–e47
Rotter ML, Larsen SO, Cooke EM et al (1988) A comparison of the effects of preoperative whole-body bathing with detergent alone and with detergent containing chlorhexidine gluconate on the frequency of wound infections after clean surgery. J Hosp Infect 11(4):310–320
Beier RC, Bischoff KM, Ziprin RL et al (2005) Chlorhexidine susceptibility, virulence factors, and antibiotic resistance of beta-hemolytic Escherichia coli isolated from neonatal swine with diarrhea. Bull Environ Contam Toxicol 75:835–844
Sidhwa F, Itani KM (2015) Skin preparation before surgery: options and evidence. Surg Infect 16(1):14–23
Dumville JC, McFarlane E, Edwards P et al (2013) Preoperative skin antiseptics for preventing surgical wound infections after clean surgery. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD003949.pub3
Edmiston CE Jr, Lee CJ, Krepel CJ, Spencer M et al (2015) Evidence for a standardized preadmission showering regimen to achieve maximal antiseptic skin surface concentrations of chlorhexidine gluconate, 4%. Surg Patients. JAMA Surg. 150(11):1027–1033
Prantl L, Schreml S, Fichtner-Feigl S, Pöppl N, Eisenmann-Klein M, Schwarze H, Füchtmeier B (2007) Clinical and morphological conditions in capsular contracture formed around silicone breast implants. Plast Reconstr Surg 120(1):275–284
Liu X, Zhou L, Pan F, Gao Y, Yuan X, Fan D (2015) Comparison of the postoperative incidence rate of capsular contracture among different breast implants: a cumulative meta-analysis. PLoS One 10(2):e0116071
Funding
The authors declare no financial support for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Campolina, A.C., Maricevich, J.P.B.R., Silva, R.O. et al. Evaluation of Chlorhexidine Concentration on the Skin After Preoperative Surgical Site Preparation in Breast Surgery—A Randomized Controlled Trial. Aesth Plast Surg 46, 1517–1522 (2022). https://doi.org/10.1007/s00266-022-02908-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-022-02908-5