Abstract
Purpose
Reverse shoulder arthroplasty (RSA) has shown improvement in clinical outcomes for various conditions, although some authors expressed concern about the restoration of active internal rotation (AIR). The current study assesses preoperative and intraoperative predictive factors of AIR in patients having a Grammont-style RSA with a minimum five year follow-up.
Methods
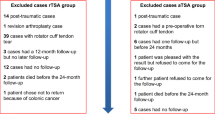
We conducted a retrospective multicentric study, including patients operated on with a 155° Grammont-style RSA for cuff-related pathology or primary osteoarthritis with posterior subluxation or an associated cuff tear. Patients were clinically evaluated at a minimum of five year follow-up. Patients with previous surgery or those who had a tendon transfer with the RSA were excluded. Demographic parameters, BMI, preoperative notes, and operative reports were obtained from medical records. AIR was graded according to the constant score system from 0 to 10.
Results
A total of 280 shoulders in 269 patients (mean age at surgery, 74.9 ± 5.9 years) met the inclusion criteria and were analyzed. The average follow-up was 8.1 years (range, 5–16 years). Overall, AIR increased from 4.2 (SD 2.5, range 0 to 10) preoperatively to 5.9 (SD 2.6, range 0 to 10) at final follow-up. At the last follow-up, AIR increased in 56% of cases, was unchanged in 26% and decreased in 18%. In 188 shoulders (67%), internal rotation was functional and allowed patients to reach the level of L3 or higher. Multivariable linear regression found the following preoperative clinical factors predictive of worse AIR after RSA: male gender (ß = −1.25 [−2.10; −0.40]; p = 0.0042) and higher values of BMI (ß = −0.085 [−0.17; −0.0065]; p = 0.048). Two surgical factors were associated with better AIR after RSA: glenoid lateralization with BIO-RSA technique (ß = 0.80 [0.043; 1.56]; p = 0.039) and subscapularis repair (ß = 1.16 [0.29; 2.02]; p = 0.0092).
Conclusions
With a mean of eight year follow-up (5 to 16 years), internal rotation was functional (≥ L3 level) in 67% of operated shoulders after Grammont-style RSA; however, two patients out of ten had decreased AIR after surgery. Male patients and those with higher BMIs had worse AIR, with glenoid lateralization (using the BIO-RSA technique) and subscapularis repair, as they are predictive of increased AIR after RSA.
Level of evidence
Case series, Level IV

Similar content being viewed by others

Data availability
Data is available upon reasonable request and in respect of applicable privacy regulations.
References
Kennedy J, Klifto CS, Ledbetter L, Bullock GS (2021) Reverse total shoulder arthroplasty clinical and patient-reported outcomes and complications stratified by preoperative diagnosis: a systematic review. J Shoulder Elbow Surg 30:929–941. https://doi.org/10.1016/j.jse.2020.09.028
Coscia AC, Matar RN, Espinal EE et al (2021) Does preoperative diagnosis impact patient outcomes following reverse total shoulder arthroplasty? A systematic review. J Should Elbow Surg 30:1458–1470. https://doi.org/10.1016/j.jse.2020.10.003
Galvin J, Kim R, Ment A et al (2022) Outcomes and complications of primary reverse shoulder arthroplasty with minimum of two-years follow-up: a systematic review and meta-analysis. J Shoulder Elbow Surg:S1058274622005699. https://doi.org/10.1016/j.jse.2022.06.005
Petrillo S, Longo UG, Papalia R, Denaro V (2017) Reverse shoulder arthroplasty for massive irreparable rotator cuff tears and cuff tear arthropathy: a systematic review. Musculoskelet Surg 101:105–112. https://doi.org/10.1007/s12306-017-0474-z
Wright T, Samitier G, Alentorn-Geli E, Torrens C (2015) Reverse shoulder arthroplasty. Part 1: systematic review of clinical and functional outcomes. Int J Shoulder Surg 9:24. https://doi.org/10.4103/0973-6042.150226
Kim MS, Jeong HY, Kim JD et al (2019) Difficulty in performing activities of daily living associated with internal rotation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 29:86–94. https://doi.org/10.1016/j.jse.2019.05.031
Stevens CG, Struk AM, Wright TW (2014) The functional impact of bilateral reverse total shoulder arthroplasty. J Shoulder Elbow Surg 23:1341–1348. https://doi.org/10.1016/j.jse.2013.12.012
Wirth B, Kolling C, Schwyzer H-K et al (2016) Risk of insufficient internal rotation after bilateral reverse shoulder arthroplasty: clinical and patient-reported outcome in 57 patients. J Shoulder Elbow Surg 25:1146–1154. https://doi.org/10.1016/j.jse.2015.11.010
Collin P, Rol M, Muniandy M et al (2021) Relationship between postoperative integrity of subscapularis tendon and functional outcome in reverse shoulder arthroplasty. J Shoulder Elbow Surg:S1058274621005231. https://doi.org/10.1016/j.jse.2021.05.024
Dedy NJ, Gouk CJ, Taylor FJ et al (2018) Sonographic assessment of the subscapularis after reverse shoulder arthroplasty: impact of tendon integrity on shoulder function. J Shoulder Elbow Surg 27:1051–1056. https://doi.org/10.1016/j.jse.2017.12.008
Eichinger JK, Rao MV, Lin JJ et al (2021) The effect of body mass index on internal rotation and function following anatomic and reverse total shoulder arthroplasty. J Shoulder Elbow Surg 30:265–272. https://doi.org/10.1016/j.jse.2020.06.008
Lauria M, Hastings M, DiPaola MJ et al (2022) Factors affecting internal rotation following total shoulder arthroplasty. JSES Rev Rep Techn:S2666639122000876. https://doi.org/10.1016/j.xrrt.2022.08.003
Werner BC, Lederman E, Gobezie R, Denard PJ (2021) Glenoid lateralization influences active internal rotation after reverse shoulder arthroplasty. J Shoulder Elbow Surg 30:2498–2505. https://doi.org/10.1016/j.jse.2021.02.021
Rol M, Favard L, Berhouet J (2019) Factors associated with internal rotation outcomes after reverse shoulder arthroplasty. Orthop Traumatol: Surg Res 105:1515–1519. https://doi.org/10.1016/j.otsr.2019.07.024
Boileau P, Moineau G, Roussanne Y, O’Shea K (2011) Bony increased-offset reversed shoulder arthroplasty: minimizing scapular impingement while maximizing glenoid fixation. Clin Orthop Relat Res 469:2558–2567. https://doi.org/10.1007/s11999-011-1775-4
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Goutallier D, Postel JM, Bernageau J et al (1994) Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 304:78–83
Fuchs B, Weishaupt D, Zanetti M et al (1999) Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg 8:599–605
Kumar V, Schoch BS, Allen C et al (2021) Using machine learning to predict internal rotation after anatomic and reverse total shoulder arthroplasty. J Shoulder Elbow Surg:S1058274621008119. https://doi.org/10.1016/j.jse.2021.10.032
Torrens C, Guirro P, Santana F (2016) The minimal clinically important difference for function and strength in patients undergoing reverse shoulder arthroplasty. J Shoulder Elbow Surg 25:262–268. https://doi.org/10.1016/j.jse.2015.07.020
Hochreiter B, Hasler A, Hasler J et al (2021) Factors influencing functional internal rotation after reverse total shoulder arthroplasty. JSES Int 5:679–687. https://doi.org/10.1016/j.jseint.2021.03.005
Kalscheur JA, Costello PS, Emery LJ (2004) Gender differences in range of motion in older adults. Phys Occup Ther Geriatr 22:77–89. https://doi.org/10.1080/J148v22n01_05
Levy JC, Ashukem MT, Formaini NT (2016) Factors predicting postoperative range of motion for anatomic total shoulder arthroplasty. J Shoulder Elbow Surg 25:55–60. https://doi.org/10.1016/j.jse.2015.06.026
Krämer M, Bäunker A, Wellmann M et al (2016) Implant impingement during internal rotation after reverse shoulder arthroplasty. The effect of implant configuration and scapula anatomy: a biomechanical study. Clin Biomech 33:111–116. https://doi.org/10.1016/j.clinbiomech.2016.02.015
Keener JD, Patterson BM, Orvets N et al (2018) Optimizing reverse shoulder arthroplasty component position in the setting of advanced arthritis with posterior glenoid erosion: a computer-enhanced range of motion analysis. J Shoulder Elbow Surg 27:339–349. https://doi.org/10.1016/j.jse.2017.09.011
Li X, Knutson Z, Choi D et al (2013) Effects of glenosphere positioning on impingement-free internal and external rotation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 22:807–813. https://doi.org/10.1016/j.jse.2012.07.013
Boileau P, Morin-Salvo N, Bessière C et al (2020) Bony increased-offset–reverse shoulder arthroplasty: 5 to 10 years’ follow-up. J Shoulder Elbow Surg:S1058274620302093. https://doi.org/10.1016/j.jse.2020.02.008
Friedman RJ, Flurin P-H, Wright TW et al (2017) Comparison of reverse total shoulder arthroplasty outcomes with and without subscapularis repair. J Shoulder Elbow Surg 26:662–668. https://doi.org/10.1016/j.jse.2016.09.027
Oh JH, Sharma N, Rhee SM, Park JH (2020) Do individualized humeral retroversion and subscapularis repair affect the clinical outcomes of reverse total shoulder arthroplasty? J Shoulder Elbow Surg 29:821–829. https://doi.org/10.1016/j.jse.2019.08.016
Boutsiadis A, Lenoir H, Denard PJ et al (2018) The lateralization and distalization shoulder angles are important determinants of clinical outcomes in reverse shoulder arthroplasty. J Shoulder Elbow Surg 27:1226–1234. https://doi.org/10.1016/j.jse.2018.02.036
Triplet JJ, Kurowicki J, Berglund DD et al (2018) Loss of functional internal rotation following various combinations of bilateral shoulder arthroplasty. Surg Technol Int 33:326–331
Acknowledgements
We are grateful to the surgeons who participated in the data collection of some of their cases: Nicolas Bonnevialle, Nicolas Brassart, Philippe Clavert, Philippe Collin, Nicolas Jacquot, Gregory Moineau, Daniel Molé, and Christophe Trojani.
Sylvain Teissier and Agnes Uranovicz for their help in the management of this study.
Sophie Plantier for her help with retrieving data in medical records.
Author information
Authors and Affiliations
Contributions
• Study conception and design: all authors
• Material preparation and data analysis: MC
• Data collection: all authors
• Writing: MC
• Reviewing: all authors
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional review board: IRB ICR-SR-10-02. This study was performed in line with the principles of the Declaration of Helsinki.
Informed consent was obtained from all individual participants included in the study.
Competing interests
Gilles Walch, Lionel Neyton, Christophe Lévigne, Luc Favard, and Pascal Boileau are paid consultants or have been paid consultants for Tornier. Other authors do not have conflicts of interest related to this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chelli, M., Walch, G., Azar, M. et al. Glenoid lateralization and subscapularis repair are independent predictive factors of improved internal rotation after reverse shoulder arthroplasty. International Orthopaedics (SICOT) 48, 127–132 (2024). https://doi.org/10.1007/s00264-023-06048-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-06048-6