Abstract
Purpose
To determine the effect of native tibia valga on intramedullary nail (IMN) fixation of tibial shaft fractures.
Methods
Retrospective comparative cohort analysis of 110 consecutive patients with tibial shaft fractures undergoing IMN fixation at an urban level one trauma centre was performed. Medical records and radiographs were reviewed for demographics, tibia centre of rotation of angulation (CORA), nail starting point, incidence of varus malreduction, and nail/canal proportional fit.
Results
Tibia valga (CORA of ≥ 3 degrees) was present in 37 (33.6%) patients. The anatomic nail starting point distance (in relation to the lateral tibial spine) was significantly greater in the tibia valga group (12.0 mm vs. 5.0 mm, mean difference: 7.1 mm, 95% CI: 5.8 to 8.3 mm, p < 0.0001). Varus malreduction was more common in the tibia valga group (10.8% vs. 1.4%, proportional difference: 9.4%, 95% CI: − 1.0 to 21.3%, p = 0.04). Varus malreduction in the tibia valga group was associated with a decreased nail width/inner canal width proportion on multivariate analysis (OR = 0.683, 95% CI: 0.468 to 0.995, p = 0.0004).
Conclusion
Native tibia valga is common, and the use of a standard coronal IMN starting point with poor nail fit can lead to iatrogenic varus malreduction. In patients with tibia valga, maximizing nail fit or utilization of a medial starting point should be considered.





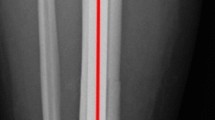
taken from the most distal aspect of the proximal fracture fragment. With inadequate nail fit, a lateral starting point in patients with tibia valga results in a nail with a medial trajectory that can induce varus malreduction upon insertion
Similar content being viewed by others
Availability of data and material
The data used in this study is not publicly available but can be made available upon reasonable request.
Code availability
The code for this study is not publicly available but can be made available upon reasonable request.
References
Zelle B, Boni G (2015) Safe surgical technique: intramedullary nail fixation of tibial shaft fractures. Patient Saf Surg 9:40. https://doi.org/10.1186/S13037-015-0086-1
Tornetta P, Riina J, Geller J, Purban W (1999) Intraarticular anatomic risks of tibial nailing. J Orthop Trauma 13:247–251. https://doi.org/10.1097/00005131-199905000-00004
McConnell T, Tornetta P, Tilzey J, Casey D (2001) Tibial portal placement: the radiographic correlate of the anatomic safe zone. J Orthop Trauma 15:207–209. https://doi.org/10.1097/00005131-200103000-00010
Byun S, Maher M, Mauffrey C, Parry J (2020) The standard sagittal starting point and entry angle for tibia intramedullary nails results in malreduction of proximal tibial fractures. Eur J Orthop Surg Traumatol 30:1057–1060. https://doi.org/10.1007/S00590-020-02669-4
Weninger P, Tschabitscher M, Traxler H et al (2010) Intramedullary nailing of proximal tibia fractures–an anatomical study comparing three lateral starting points for nail insertion. Injury 41:220–225. https://doi.org/10.1016/J.INJURY.2009.10.014
Maslow J, Joseph H, Hong D et al (2020) Radiographic evaluation of the tibial intramedullary nail entry point. J Am Acad Orthop Surg 28:e810–e814. https://doi.org/10.5435/JAAOS-D-19-00557
Alghamdi A, Rahmé M, Lavigne M et al (2014) Tibia valga morphology in osteoarthritic knees: importance of preoperative full limb radiographs in total knee arthroplasty. J Arthroplasty 29:1671–1676. https://doi.org/10.1016/j.arth.2014.03.001
Palanisami D, George MJ, Hussain AM et al (2019) Tibial bowing and tibial component placement in primary total knee arthroplasty in valgus knees: are we overlooking? J Orthop Surg 27:1–9. https://doi.org/10.1177/2309499019867006
Paley D, Bhave A, Gage J et al (2002) Principles of deformity correction, 1st edn. Springer-Verlag, Berlin, Heidelberg
Herzenberg JE, Standard SC, Conway JD et al (2013) The art of limb alignment, 2nd edn. Sinai Hospital of Baltimore, Baltimore
Tucker NJ, Mauffrey C, Parry JA (2021) Are pre- and postoperative true translational and angular displacement predictive of nonunion after intramedullary nail fixation of tibial shaft fractures? Eur J Orthop Surg Traumatol. https://doi.org/10.1007/S00590-021-03154-2
Vallier HA, Cureton BA, Patterson BM (2011) Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures. J Orthop Trauma 25:736–741. https://doi.org/10.1097/BOT.0b013e318213f709
Strage K, Parry J, Mauffrey C (2021) Standardizing statistics and data reporting in orthopaedic research. Eur J Orthop Surg Traumatol 31:1–6. https://doi.org/10.1007/S00590-020-02843-8
Donegan DJ, Akinleye S, Taylor RM et al (2016) Intramedullary nailing of tibial shaft fractures: size matters. J Orthop Trauma 30:377–380. https://doi.org/10.1097/BOT.0000000000000555
Keltz E, Dreyfuss D, Ginesin E et al (2019) Preoperative evaluation of intramedullary tibial nail measurements—a review of the literature and a new technique using contralateral radiographs and digital planning. J Am Acad Orthop Surg Glob Res Rev 3:e015. https://doi.org/10.5435/JAAOSGLOBAL-D-19-00015
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to this work and give explicit consent for submission. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval
Institutional Review Board approval was obtained prior to initiating this study. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to participate
Due to the retrospective nature of this work, informed consent was waived.
Consent for publication
Due to the retrospective and de-identified nature of this work, consent to publish was waived.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of Evidence: Level III, Retrospective cohort study
Rights and permissions
About this article
Cite this article
Tucker, N.J., Hadeed, M.M., Mauffrey, C. et al. Native tibia valga: a potential source of varus malreduction during intramedullary tibial nail fixation of tibial shaft fractures. International Orthopaedics (SICOT) 46, 1165–1173 (2022). https://doi.org/10.1007/s00264-022-05356-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05356-7