Abstract
Objective
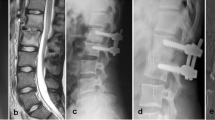
To evaluate the outcomes of debridement fusion surgery between two surgical approaches for one- or two-level lumbar vertebral osteomyelitis (LVO): oblique retroperitoneal approach (ORA) and posterior transpedicular approach (PTA).
Methods
We performed a retrospective study for adult patients with one- or two-level lumbar vertebral pyogenic spondylitis. The primary clinical outcomes included the following: surgery-related information (intra-operative blood loss, operation time, and hospital length of stay), infection control (primary failure and recurrence), and bony fusion. The secondary objective was to determine the differences between groups in mean reduction of pain characters and physical functioning.
Results
The data of 80 patients were collected retrospectively. The duration of follow-up was 27.8 ± 4.7 months (range, 24–42). Intra-operative blood loss, operation time, and hospital length of stay in ORA debridement were significantly lower. Primary failure (2.3% vs 2.7%) was similar between the groups, but recurrence (13.9% vs 5.4%) had difference. Bony fusion (94.6.3% vs 86.1.%) in ORA debridement was higher than those in PTA debridement at the final follow-up. Fusion occurred at six to 14 months (mean 9.8 months). Patients in ORA group had better results in functional and pain scores in the first three months, with similar results at the final follow-up.
Conclusion
In summary, ORA debridement provides a quicker recovery compared with PTA debridement for one- or two-level LVO. As for the infection control and fusion rate, both debridement approaches had similar results.




Similar content being viewed by others
References
Chen WH, Jiang LS, Dai LY (2007) Surgical treatment of pyogenic vertebral osteomyelitis with spinal instrumentation. Eur Spine J 16:1307–1316. https://doi.org/10.1007/s00586-006-0251-4
Si M, Yang ZP, Li ZF, Yang Q, Li JM (2013) Anterior versus posterior fixation for the treatment of lumbar pyogenic vertebral osteomyelitis. Orthopedics 36:831–836. https://doi.org/10.3928/01477447-20130523-33
Lee JS, Moon KP, Kim SJ, Suh KT (2007) Posterior lumbar interbody fusion and posterior instrumentation in the surgical management of lumbar tuberculous spondylitis. J Bone Joint Surg Br 89:210–214. https://doi.org/10.1302/0301-620X.89B2.17849
Wang LJ, Zhang HQ, Tang MX, Gao QL, Zhou ZH, Yin XH (2017) Comparison of three surgical approaches for thoracic spinal tuberculosis in adult: minimum 5-year follow-up. Spine (Phila Pa 1976) 42:808–817. https://doi.org/10.1097/BRS.0000000000001955
Yang P, Zang Q, Kang J, Li H, He X (2016) Comparison of clinical efficacy and safety among three surgical approaches for the treatment of spinal tuberculosis: a meta-analysis. Eur Spine J 25:3862–3874. https://doi.org/10.1007/s00586-016-4546-9
Agha RA, Borrelli MR, Vella-Baldacchino M, Thavayogan R, Orgill DP, STROCSS Group (2017) The STROCSS statement: strengthening the reporting of cohort studies in surgery. Int J Surg 46:198–202. https://doi.org/10.1016/j.ijsu.2017.08.586
Zhu Y, Wu P, Luo W, Zhao Z, Ou Y (2019) Single-stage posterior instrumentation and unilateral transpedicular debridement for the treatment of thoracolumbar tuberculosis: three years of follow-up. World Neurosurg 121:e230–e236. https://doi.org/10.1016/j.wneu.2018.09.085
Khan MH, Smith PN, Rao N, Donaldson WF (2006) Serum C-reactive protein levels correlate with clinical response in patients treated with antibiotics for wound infections after spinal surgery. Spine J 6:311–315. https://doi.org/10.1016/j.spinee.2005.07.006
Park KH, Cho OH, Lee YM et al (2015) Therapeutic outcomes of hematogenous vertebral osteomyelitis with instrumented surgery. Clin Infect Dis 60:1330–1338. https://doi.org/10.1093/cid/civ066
Lee CK, Vessa P, Lee JK (1995) Chronic disabling low back pain syndrome caused by internal disc derangements: the results of disc excision and posterior lumbar interbody fusion. Spine (Phila Pa 1976) 20:356–361. https://doi.org/10.1097/00007632-199502000-00018
Papuga MO, Mesfin A, Molinari R, Rubery PT (2016) Correlation of PROMIS physical function and pain CAT instruments with Oswestry Disability Index and Neck Disability Index in spine patients. Spine (Phila Pa 1976) 41:1153–1159. https://doi.org/10.1097/BRS.0000000000001518
Rayes M, Colen CB, Bahgat DA, Higashida T, Guthikonda M, Rengachary S, Eltahawy HA (2010) Safety of instrumentation in patients with spinal infection. J Neurosurg Spine 12:647–659. https://doi.org/10.3171/2009.12.SPINE09428
Hodgson AR, Stock FE, Fang HS, Ong GB (1960) Anterior spinal fusion: the operative approach and pathological findings in 412 patients with Pott’s disease of the spine. Br J Surg 48:172–178. https://doi.org/10.1002/bjs.18004820819
Jensen AG, Espersen F, Skinhøj P, Frimodt-Møller N (1998) Bacteremic Staphylococcus aureus spondylitis. Arch Intern Med 158:509–517. https://doi.org/10.1001/archinte.158.5.509
Kim CJ, Song KH, Park WB, Kim ES, Park SW, Kim HB, Oh MD, Kim NJ (2012) Microbiologically and clinically diagnosed vertebral osteomyelitis: impact of prior antibiotic exposure. Antimicrob Agents Chemother 56:2122–2124. https://doi.org/10.1128/AAC.05953-11
Carragee EJ, Kim D, van der Vlugt T, Vittum D (1997) The clinical use of erythrocyte sedimentation rate in pyogenic vertebral osteomyelitis. Spine (Phila Pa 1976) 22:2089–2093. https://doi.org/10.1097/00007632-199709150-00005
Arnold R, Rock C, Croft L, Gilliam BL, Morgan DJ (2014) Factors associated with treatment failure in vertebral osteomyelitis requiring spinal instrumentation. Antimicrob Agents Chemother 58:880–884. https://doi.org/10.1128/AAC.01452-13
Lall RR, Wong AP, Lall RR, Lawton CD, Smith ZA, Dahdaleh NS (2015) Evidence-based management of deep wound infection after spinal instrumentation. J Clin Neurosci 22(2):238–242. https://doi.org/10.1016/j.jocn.2014.07.010
Panjabi MM (2003) Clinical spinal instability and low back pain. J Electromyogr Kinesiol 13:371–379. https://doi.org/10.1016/s1050-6411(03)00044-0
O’Sullivan PB (2000) Lumbar segmental ‘instability’: clinical presentation and specific stabilizing exercise management. Man Ther 5:2–12. https://doi.org/10.1054/math.1999.0213
Colmenero JD, Jiménez-Mejías ME, Sánchez-Lora FJ, Reguera JM, Palomino-Nicás J, Martos F, García de las Heras J, Pachón J (1997) Pyogenic, tuberculous, and brucellar vertebral osteomyelitis: a descriptive and comparative study of 219 cases. Ann Rheum Dis 56:709–715. https://doi.org/10.1136/ard.56.12.709
Leone A, Guglielmi G, Cassar-Pullicino VN, Bonomo L (2007) Lumbar intervertebral instability: a review. Radiology 245:62–77. https://doi.org/10.1148/radiol.2451051359
O’Daly BJ, Morris SF, O’Rourke SK (2008) Long-term functional outcome in pyogenic spinal infection. Spine (Phila Pa 1976) 33:E246–E253. https://doi.org/10.1097/BRS.0b013e31816b8872
Author information
Authors and Affiliations
Contributions
W.L and Y.O. conceived and designed the study. X.D collected the data. X.D. and B.W. analyzed the data. B.W. performed the statistical analyses. W.L. wrote the manuscript. All authors reviewed and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethical approval
This study was approved by the Institutional Review Board of The First Affiliated Hospital of Chongqing Medical University.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luo, W., Ou, Ys., Du, X. et al. Anterior oblique retroperitoneal approach vs posterior transpedicular approach for the treatment of one- or two-level lumbar vertebral osteomyelitis: a retrospective cohort study. International Orthopaedics (SICOT) 44, 2349–2356 (2020). https://doi.org/10.1007/s00264-020-04650-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04650-6