Abstract
Introduction
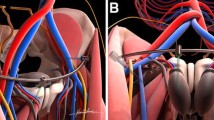
Subcutaneous internal fixation (InFix) has become a valid alternative for anterior fixation of pelvic ring injuries. Complications associated with this technique are lateral femoral cutaneous nerve (LFCN) irritation and anterior thigh pain due to prominent implants. The aim of this study was to identify a configuration of the InFix that causes the least adverse side effects.
Methods
Nineteen patients (6 females, mean age 61 years) with 38 hemipelves were included. Rod-to-bone distance and symphysis-rod distance were measured on AP- and outlet- radiographs. These distances were analyzed in relation to the primary outcomes: early removal of the InFix, post-operative complications and damage of the LFCN.
Results
Regarding rod-to-bone distance, a distance of 20 to 25 mm causes less complications, LFCN damage and no early removals of the InFix. Symphysis-to-rod distance analysis showed the best results regarding LFCN damage and other complications when the rod had a distance of less than 40 mm to the symphysis. A distance more than 40 mm was associated with fewer early removal of the InFix.
Conclusions
Planned optimized configuration of the InFix with a rod-to-bone distance between 20 and 25 mm may reduce postoperative complications. Regarding LFCN damage, the rod-to-symphysis distance should not be more than 40 mm.






Similar content being viewed by others
References
Bates P, Gary J, Singh G, Reinert C, Starr A (2011) Percutaneous treatment of pelvic and acetabular fractures in obese patients. Orthop Clin N Am 42(1):55–67 vi
Miller PR, Moore PS, Mansell E, Meredith JW, Chang MC (2003) External fixation or arteriogram in bleeding pelvic fracture: initial therapy guided by markers of arterial hemorrhage. J Trauma 54(3):437–443
Mason WT, Khan SN, James CL, Chesser TJ, Ward AJ (2005) Complications of temporary and definitive external fixation of pelvic ring injuries. Injury 36(5):599–604
Vaidya R, Colen R, Vigdorchik J, Tonnos F, Sethi A (2012) Treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior fixation: initial clinical series. J Orthop Trauma 26(1):1–8
Scheyerer MJ, Zimmermann SM, Osterhoff G, Tiziani S, Simmen HP, Wanner GA, Werner CM (2014) Anterior subcutaneous internal fixation for treatment of unstable pelvic fractures. BMC Res Notes 7:133
Osterhoff G, Tiziani S, Ferguson SJ, Spreiter G, Scheyerer MJ, Spinas GL, Wanner GA, Simmen HP, Werner CM (2014) Mechanical testing of a device for subcutaneous internal anterior pelvic ring fixation versus external pelvic ring fixation. BMC Musculoskelet Disord 15:111
Fang C, Alabdulrahman H, Pape HC (2017) Complications after percutaneous internal fixator for anterior pelvic ring injuries. Int Orthop 41(9):1785–1790
Hesse D, Kandmir U, Solberg B, Stroh A, Osgood G, Sems SA, Collinge CA (2015) Femoral nerve palsy after pelvic fracture treated with INFIX: a case series. J Orthop Trauma 29(3):138–143
Rudin D, Manestar M, Ullrich O, Erhardt J, Grob K (2016) The anatomical course of the lateral femoral cutaneous nerve with special attention to the anterior approach to the hip joint. J Bone Joint Surg Am 98(7):561–567
Osterhoff G, Aichner EV, Scherer J, Simmen HP, Werner CML, Feigl GC (2017) Anterior subcutaneous internal fixation of the pelvis - what rod-to-bone distance is anatomically optimal? Injury 48(10):2162–2168
Schmitz P, Baumann F, Acklin YP, Gueorguiev B, Nerlich M, Grechenig S, Muller MB (2018) Clinical application of a minimally invasive cement-augmentable Schanz screw rod system to treat pelvic ring fractures. Int Orthop. https://doi.org/10.1007/s00264-018-3988-6
Vaidya R, Nasr K, Feria-Arias E, Fisher R, Kajy M, Diebel LN (2016) INFIX/EXFIX: massive open pelvic injuries and review of the literature. Case Rep Orthop 2016:9468285
Blum L, Hake ME, Charles R, Conlan T, Rojas D, Martin MT, Mauffrey C (2018) Vertical shear pelvic injury: evaluation, management, and fixation strategies. Int Orthop. https://doi.org/10.1007/s00264-018-3883-1
Cai L, Lou Y, Guo X, Wang J (2017) Surgical treatment of unstable pelvic fractures with concomitant acetabular fractures. Int Orthop 41(9):1803–1811
Wu X (2018) A biomechanical comparison of different fixation techniques for fractures of the acetabular posterior wall. Int Orthop 42(3):673–679
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was carried out in accordance with the local institutional ethics committee’s terms of reference (Kantonale Ethikkommission Zürich, Switzerland. BASEC-Nr. 2016-01954).
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Scherer, J., Tiziani, S., Sprengel, K. et al. Subcutaneous internal anterior fixation of pelvis fractures—which configuration of the InFix is clinically optimal?—a retrospective study. International Orthopaedics (SICOT) 43, 2161–2166 (2019). https://doi.org/10.1007/s00264-018-4110-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4110-9