Abstract
Purpose
Periprosthetic hip infection (PHI) is a devastating complication. The association between PHI and bearing surfaces as well as patient-related factors has been recently investigated, with contradictive outcomes. The dataset of Emilia-Romagna region Registry for Orthopaedic Prosthetic Implants (RIPO) has been assessed to investigate, if the bearing choice influenced the risk of septic loosening occurrence.
Methods
RIPO data about 39,206 cementless total hip arthroplasties (THA), collected since 2003, were analysed. Age, gender, BMI, diabetes and bearing surfaces were evaluated. The end point of the study was the revision of at least a single component due to sepsis.
Results
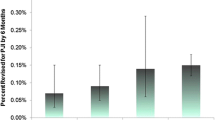
Adjusted and unadjusted survival rates showed that ceramic-on-ceramic (COC) implants had the lower incidence of PHIs, whereas metal-on-metal (MOM) THAs were significantly more prone to infection. In MOM cohort, stemmed implants were involved in 28 out of 30 cases. Among the demographical features and comorbid conditions, only diabetes statistically influenced the rate of sepsis.
Conclusions
Bearing surfaces influenced the rate of PHI; in particular, stemmed MOM implants were at higher risk, probably due to metal debris consequent to taperosis. Despite the preliminary results, stemmed MOM THAs should be used with care, and diabetic patients should be warned about increased septic risks.



Similar content being viewed by others
References
Kuzyk PR, Dhotar HS, Sternheim A, Gross AE, Safir O, Backstein D (2014) Two-stage revision arthroplasty for management of chronic periprosthetic hip and knee infection: techniques, controversies, and outcomes. J Am Acad Orthop Surg 22(3):153–164
Kobayashi S, Kubo T, Iwamoto Y, Fukushima W, Sugano N. (2018) Nationwide multicenter follow-up cohort study of hip arthroplasties performed for osteonecrosis of the femoral head. Int Orthop. 2018 may 12. doi: https://doi.org/10.1007/s00264-018-3980-1
Triantafyllopoulos GK, Soranoglou VG, Memtsoudis SG, Sculco TP, Poultsides LA (2017) Rate and risk factors for periprosthetic joint infection among 36,494 primary total hip arthroplasties. J Arthroplast. https://doi.org/10.1016/j.arth.2017.11.040
Merollini KM, Zheng H, Graves N (2013) Most relevant strategies for preventing surgical site infection after total hip arthroplasty: guideline recommendations and expert opinion. Am J Infect Control 41(3):221–226
Abdelaziz H, Zahar A, Lausmann C, Gehrke T, Fickenscher H, Suero EM, Gebauer M, Citak M (2018) High bacterial contamination rate of electrocautery tips during total hip and knee arthroplasty. Int Orthop 42(4):755–760. https://doi.org/10.1007/s00264-018-3822-1
Lass R, Giurea A, Kubista B, Hirschl AM, Graninger W, Presterl E, Windhager R, Holinka J (2014) Bacterial adherence to different components of total hip prosthesis in patients with prosthetic joint infection. Int Orthop 38(8):1597–1602
Lee YK, Yoon BH, Choi YS, Jo WL, Ha YC, Koo KH (2016) Metal on metal or ceramic on ceramic for cementless total hip arthroplasty: a meta-analysis. J Arthroplasty 31(11):2637–2645.e1
Pitto RP, Sedel L (2016) Periprosthetic joint infection in hip arthroplasty: is there an association between infection and bearing surface type? Clin Orthop Relat Res 474(10):2213–2218
Australian Orthopaedic Association National Joint Replacement Registry. Annual report 2017. https://aoanjrr.sahmri.com/. Accessed 18 Febraury 2018
Nandi S (2016) CORR insights(®): periprosthetic joint infection in hip arthroplasty: is there an association between infection and bearing surface type? Clin Orthop Relat Res 474(10):2219–2220
RIPO. Annual Report 2015. https://ripo.cineca.it, Accessed 19 February 2018
Ali A, Sundberg M, Robertsson O, Dahlberg LE, Thorstensson CA, Redlund-Johnell I, Kristiansson I, Lindstrand A (2014) Dissatisfied patients after total knee arthroplasty: a registry study involving 114 patients with 8-13 years of followup. Acta Orthop 85(3):229–233
Pedersen AB, Mehnert F, Johnses SP, Sorensen HT (2010) Risk of revision of a total hip replacement in patients with diabetes mellitus. A population-based follow up study. J Bone Joint Surg 92-B:929–934
Tao R, Liu F, Liu YK, Lu Y, Xu H, Cao Y, Zhou ZY, Wang W (2018) A prospective comparative study of hip resurfacing arthroplasty and large-diameter head metal-on-metal total hip arthroplasty in younger patients-a minimum of five year follow-up. Int Orthop. https://doi.org/10.1007/s00264-018-3819-9
Bozic KJ, Ong K, Lau E, Kurtz SM, Vail TP, Rubash HE, Berry DJ (2010) Risk of complication and revision total hip arthroplasty among medicare patients with different bearing surfaces. Clin Orthop Relat Res 468(9):2357–2362
National Joint Registry. Annual report 2017. http://www.njrcentre.org.uk. Accessed 19 February 2018
Grammatopoulos G, Munemoto M, Inagaki Y, Tanaka Y, Athanasou NA (2016) The diagnosis of infection in metal-on-metal hip arthroplasties. J Arthroplast 31(11):2569–2573
Mahendra G, Pandit H, Kliskey K, Murray D, Gill HS, Athanasou N (2009) Necrotic and inflammatory changes in metal-on-metal resurfacing hip arthroplasties. Acta Orthop 80(6):653–659
Huk OL, Catelas I, Mwale F, Antoniou J, Zukor DJ, Petit A (2004) Induction of apoptosis and necrosis by metal ions in vitro. J Arthroplast 19(8 Suppl 3):84–87
Lanting BA, Teeter MG, Howard JL, MacDonald SJ, Van Citters DW (2017) Metal-on-metal compared with metal-on-polyethylene: the effect on trunnion corrosion in total hip arthroplasty. J Arthroplast 32(8):2574–2579
Daniel J, Holland J, Quigley L, Sprague S, Bhandari M (2012) Pseudotumors associated with total hip arthroplasty. J Bone Joint Surg Am 94(1):86–93
Mutimer J, Devane PA, Adams K, Horne JG (2010) Highly crosslinked polyethylene reduces wear in total hip arthroplasty at 5 years. Clin Orthop Relat Res 468(12):3228–3233
Bozic KJ, Ward DT, Lau EC, Chan V, Wetters NG, Naziri Q, Odum S, Fehring TK, Mont MA, Gioe TJ, Della Valle CJ (2014) Risk factors for periprosthetic joint infection following primary total hip arthroplasty: a case control study. J Arthroplast 29(1):154–156
Zhu M, Ravi S, Frampton C, Luey C, Young S (2016) New Zealand Joint Registry data underestimates the rate of prosthetic joint infection. Acta Orthop 87(4):346–350
Whitehouse MR, Endo M, Zachara S, Nielsen TO, Greidanus NV, Masri BA, Garbuz DS, Duncan CP (2015) Adverse local tissue reactions in metal-on-polyethylene total hip arthroplasty due to trunnion corrosion: the risk of misdiagnosis. Bone Joint J 97(8):1024–1030
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The senior author is paid consultant for Zimmer (Warsaw, US), Adler Ortho (Milan, Italy) and CeramTec (Plochingen, Germany). The other authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was not necessary as the registry collects personal data as standard practice and conceals the identity of the patients.
Rights and permissions
About this article
Cite this article
Bordini, B., Stea, S., Castagnini, F. et al. The influence of bearing surfaces on periprosthetic hip infections: analysis of thirty nine thousand, two hundred and six cementless total hip arthroplasties. International Orthopaedics (SICOT) 43, 103–109 (2019). https://doi.org/10.1007/s00264-018-4097-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4097-2