Abstract
Background
There is still no specific real-world data regarding the clinical activity of immune checkpoint inhibitors in the elderly with liver cancer. Our study aimed to compare the efficacy and safety of immune checkpoint inhibitors between patients aged ≥ 65 years and the younger group, while exploring their differences in genomic background and tumor microenvironment.
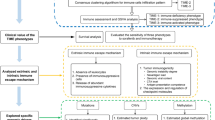
Methods
This retrospective study was conducted at two hospitals in China and included 540 patients treated with immune checkpoint inhibitors for primary liver cancer between January 2018 and December 2021. Patients’ medical records were reviewed for clinical and radiological data and oncologic outcomes. The genomic and clinical data of patients with primary liver cancer were extracted and analyzed from TCGA-LIHC, GSE14520, and GSE140901 datasets.
Results
Ninety-two patients were classified as elderly and showed better progression-free survival (P = 0.027) and disease control rate (P = 0.014). No difference was observed in overall survival (P = 0.69) or objective response rate (P = 0.423) between the two age groups. No significant difference was reported concerning the number (P = 0.824) and severity (P = 0.421) of adverse events. The enrichment analyses indicated that the elderly group was linked to lower expression of oncogenic pathways, such as PI3K-Akt, Wnt, and IL-17. The elderly had a higher tumor mutation burden than younger patients.
Conclusions
Our results indicated that immune checkpoint inhibitors might exhibit better efficacy in the elderly with primary liver cancer, with no increased adverse events. Differences in genomic characteristics and tumor mutation burden may partially explain these results.



Similar content being viewed by others
Data availability
Due to the privacy of patients, the data related to patients cannot be available for public access but can be obtained from the corresponding author on reasonable request approved by the institutional review board of all enrolled centers.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249
Zheng R, Zhang S, Zeng H, Wang S, Sun K, Chen R et al (2022) Cancer incidence and mortality in China, 2016. J Natl Cancer Cent 2:1–9
Villanueva A (2019) Hepatocellular carcinoma. N Engl J Med 380:1450–1462
Vogel A, Martinelli E, Committee EG (2021) Updated treatment recommendations for hepatocellular carcinoma (HCC) from the ESMO clinical practice guidelines. Ann Oncol 32:801–805
Kulik L, El-Serag HB (2019) Epidemiology and management of hepatocellular carcinoma. Gastroenterology 156:477-491.e471
Yau T, Park JW, Finn RS, Cheng AL, Mathurin P, Edeline J et al (2022) Nivolumab versus sorafenib in advanced hepatocellular carcinoma (CheckMate 459): a randomised, multicentre, open-label, phase 3 trial. Lancet Oncol 23:77–90
Lian J, Yue Y, Yu W, Zhang Y (2020) Immunosenescence: a key player in cancer development. J Hematol Oncol 13:151
Hurez V, Padron AS, Svatek RS, Curiel TJ (2017) Considerations for successful cancer immunotherapy in aged hosts. Clin Exp Immunol 187:53–63
Ren Z, Xu J, Bai Y, Xu A, Cang S, Du C et al (2021) Sintilimab plus a bevacizumab biosimilar (IBI305) versus sorafenib in unresectable hepatocellular carcinoma (ORIENT-32): a randomised, open-label, phase 2–3 study. Lancet Oncol 22:977–990
Qin S, Ren Z, Meng Z, Chen Z, Chai X, Xiong J et al (2020) Camrelizumab in patients with previously treated advanced hepatocellular carcinoma: a multicentre, open-label, parallel-group, randomised, phase 2 trial. Lancet Oncol 21:571–580
Finn RS, Qin S, Ikeda M, Galle PR, Ducreux M, Kim TY et al (2020) Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med 382:1894–1905
Hurria A, Levit LA, Dale W, Mohile SG, Muss HB, Fehrenbacher L et al (2015) Improving the evidence base for treating older adults with cancer: American society of clinical oncology statement. J Clin Oncol 33:3826–3833
Nemoto Y, Ishihara H, Nakamura K, Tachibana H, Fukuda H, Yoshida K et al (2022) Efficacy and safety of immune checkpoint inhibitors in elderly patients with metastatic renal cell carcinoma. Int Urol Nephrol 54:47–54
Saleh K, Auperin A, Martin N, Borcoman E, Torossian N, Iacob M et al (2021) Efficacy and safety of immune checkpoint inhibitors in elderly patients (>/=70 years) with squamous cell carcinoma of the head and neck. Eur J Cancer 157:190–197
Grossi F, Crinò L, Logroscino A, Canova S, Delmonte A, Melotti B et al (2018) Use of nivolumab in elderly patients with advanced squamous non-small-cell lung cancer: results from the Italian cohort of an expanded access programme. Eur J Cancer 100:126–134
Perier-Muzet M, Gatt E, Péron J, Falandry C, Amini-Adlé M, Thomas L et al (2018) Association of immunotherapy with overall survival in elderly patients with melanoma. JAMA Dermatol 154:82–87
Kugel CH 3rd, Douglass SM, Webster MR, Kaur A, Liu Q, Yin X et al (2018) Age correlates with response to anti-PD1, reflecting age-related differences in intratumoral effector and regulatory T-cell populations. Clin Cancer Res 24:5347–5356
Storm BN, Abedian Kalkhoran H, Wilms EB, Brocken P, Codrington H, Houtsma D et al (2022) Real-life safety of PD-1 and PD-L1 inhibitors in older patients with cancer: an observational study. J Geriatr Oncol 13(7):997–1002
Wildiers H, Heeren P, Puts M, Topinkova E, Janssen-Heijnen ML, Extermann M et al (2014) International society of geriatric oncology consensus on geriatric assessment in older patients with cancer. J Clin Oncol 32:2595–2603
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247
Mayakonda A, Lin DC, Assenov Y, Plass C, Koeffler HP (2018) Maftools: efficient and comprehensive analysis of somatic variants in cancer. Genome Res 28:1747–1756
Elias R, Giobbie-Hurder A, McCleary NJ, Ott P, Hodi FS, Rahma O (2018) Efficacy of PD-1 & PD-L1 inhibitors in older adults: a meta-analysis. J Immunother Cancer 6:26
Poropatich K, Fontanarosa J, Samant S, Sosman JA, Zhang B (2017) Cancer immunotherapies: Are they as effective in the elderly? Drugs Aging 34:567–581
Corbaux P, Maillet D, Boespflug A, Locatelli-Sanchez M, Perier-Muzet M, Duruisseaux M et al (2019) Older and younger patients treated with immune checkpoint inhibitors have similar outcomes in real-life setting. Eur J Cancer 121:192–201
Wu Q, Wang Q, Tang X, Xu R, Zhang L, Chen X et al (2019) Correlation between patients’ age and cancer immunotherapy efficacy. Oncoimmunology 8:e1568810
Finn RS, Ryoo BY, Merle P, Kudo M, Bouattour M, Lim HY et al (2020) Pembrolizumab as second-line therapy in patients with advanced hepatocellular carcinoma in KEYNOTE-240: a randomized, double-blind, phase III trial. J Clin Oncol 38:193–202
Shenoy P, Harugeri A (2015) Elderly patients’ participation in clinical trials. Perspect Clin Res 6:184–189
Li R, Zheng C, Wang Q, Bi E, Yang M, Hou J et al (2021) Identification of an immunogenic DKK1 long peptide for immunotherapy of human multiple myeloma. Haematologica 106:838–846
Li H, Cui ML, Chen TY, Xie HY, Cui Y, Tu H et al (2015) Serum DLK1 is a potential prognostic biomarker in patients with hepatocellular carcinoma. Tumour Biol 36:8399–8404
Pittaway JFH, Lipsos C, Mariniello K, Guasti L (2021) The role of delta-like non-canonical Notch ligand 1 (DLK1) in cancer. Endocr Relat Cancer 28:R271-r287
Zhou L, Zhu Y (2018) The EpCAM overexpression is associated with clinicopathological significance and prognosis in hepatocellular carcinoma patients: a systematic review and meta-analysis. Int J Surg 56:274–280
Llovet JM, Castet F, Heikenwalder M, Maini MK, Mazzaferro V, Pinato DJ et al (2022) Immunotherapies for hepatocellular carcinoma. Nat Rev Clin Oncol 19:151–172
Ma HY, Yamamoto G, Xu J, Liu X, Karin D, Kim JY et al (2020) IL-17 signaling in steatotic hepatocytes and macrophages promotes hepatocellular carcinoma in alcohol-related liver disease. J Hepatol 72:946–959
Liu C, Liu R, Wang B, Lian J, Yao Y, Sun H et al (2021) Blocking IL-17A enhances tumor response to anti-PD-1 immunotherapy in microsatellite stable colorectal cancer. J Immunother Cancer 9
Wu Y, Zhang Y, Qin X, Geng H, Zuo D, Zhao Q (2020) PI3K/AKT/mTOR pathway-related long non-coding RNAs: roles and mechanisms in hepatocellular carcinoma. Pharmacol Res 160:105195
O’Donnell JS, Massi D, Teng MWL, Mandala M (2018) PI3K-AKT-mTOR inhibition in cancer immunotherapy, redux. Semin Cancer Biol 48:91–103
Chan TA, Yarchoan M, Jaffee E, Swanton C, Quezada SA, Stenzinger A et al (2019) Development of tumor mutation burden as an immunotherapy biomarker: utility for the oncology clinic. Ann Oncol 30:44–56
Gok Yavuz B, Hasanov E, Lee SS, Mohamed YI, Curran MA, Koay EJ et al (2021) Current landscape and future directions of biomarkers for immunotherapy in hepatocellular carcinoma. J Hepatocell Carcinoma 8:1195–1207
Muhammed A, D’Alessio A, Enica A, Talbot T, Fulgenzi CAM, Nteliopoulos G et al (2022) Predictive biomarkers of response to immune checkpoint inhibitors in hepatocellular carcinoma. Expert Rev Mol Diagn 22:253–264
Acknowledgements
We thank all the participants in our study.
Funding
This work was supported by the National Nature Science Foundation of China (No. 81972897, 82172751), China Postdoctoral Science Foundation (No. 2021M701629), Guangzhou Science and Technology Project (No. 202201011183), and Guangdong Natural Science Foundation (No. 2022A1515110656).
Author information
Authors and Affiliations
Contributions
Conceptualisation: LX and LZ; Resources: HD, LX and LL; Investigation and methodology: HC; Data curation: LZ, HZ, JW, QL, and CH; Formal analysis and visualisation: LZ; Validation: RL, and JH; Writing-original draft: LZ, and HZ; Writing-review and editing: LX and YL; Funding acquisition: LL; Supervision: HZ and LL. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
All the authors declare that they have no confict of interest.
Consent to participate
The need for obtaining informed consent was waived owing to the retrospective study design.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study design was approved by the Medical Ethics Committee of Nanfang Hospital, Southern Medical University (approval number: NFEC-2021-048).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
262_2023_3417_MOESM2_ESM.eps
Supplementary Fig. 2 (a-c) GO enrichment analyses of the DEGs identified from TCGA-LIHC (a), GSE14520 (b), and GSE140901 (c). (d) The upregulated and downregulated pathways associated with DEGs of KEGG analysis in GSE140901. GO, Gene Ontology; KEGG, Kyoto Encyclopedia of Genes and Genomes (EPS 10317 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xiao, L., Liao, Y., Wang, J. et al. Efficacy and safety of immune checkpoint inhibitors in elderly patients with primary liver cancer: a retrospective, multicenter, real-world cohort study. Cancer Immunol Immunother 72, 2299–2308 (2023). https://doi.org/10.1007/s00262-023-03417-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-023-03417-3