Abstract
Background
We investigated the combined effects of sarcopenia and inflammation on outcomes in patients with HCC treated with nivolumab.
Materials and Methods
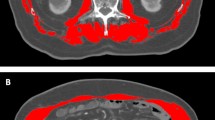
We reviewed 102 patients treated with nivolumab between 2017 and 2018. Sarcopenia was diagnosed when the L3 skeletal muscle indices were < 42 cm2/m2 and < 38 cm2/m2 in men and women, respectively. Baseline neutrophil-to-lymphocyte ratio (NLR) and absolute lymphocyte count were used as surrogate markers of inflammation and immune cell reservoir. High NLR (hNLR) was defined as NLR ≥ 3, and severe lymphopenia (sLP) was defined as lymphocyte < 800/μL. The overall survival (OS) and progression-free survival (PFS) were analyzed.
Results
With a median follow-up of 21.9 (interquartile range, 8.3–58.3) months, patients with sarcopenia showed shorter OS than those without sarcopenia (median, 2.9 vs. 7.5 months, respectively). Patients with either hNLR or sLP exhibited inferior survival than those without risk factor (median OS, 2.8 vs. 14.5 months; median PFS, 1.3 vs. 3.7 months, respectively). Among 70 patients treated with RT, benefit of RT was observed in patients with sarcopenia or those without hNLR/sLP (all p < 0.05). After multivariable analysis, RT, hNLR/sLP, albumin–bilirubin (ALBI) grade, and alpha-fetoprotein were significantly associated with OS (all p < 0.05), and hNLR/sLP was also associated with decreased PFS together with ALBI grade, alpha-fetoprotein, and RT (all p < 0.05).
Conclusion
The current study hypothetically demonstrated that the risk group stratified by hNLR/sLP outweighs the significance of sarcopenia in predicting outcomes after nivolumab. Furthermore, patients with sarcopenia might benefit from RT, especially those without risk factors of hNLR/sLP.



Similar content being viewed by others
Data availability
Data availability is limited due to institutional data protection law and confidentiality of patient data.
Abbreviations
- ALBI:
-
Albumin–bilirubin
- HCC:
-
Hepatocellular carcinoma
- hNLR:
-
High neutrophil-to-lymphocyte ratio
- HR:
-
Hazard ratio
- ICB:
-
Immune checkpoint blockade
- IQR:
-
Interquartile range
- NLR:
-
Neutrophil-to-lymphocyte ratio
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- RT:
-
Radiation therapy
- sLP:
-
Severe lymphopenia
- SMI:
-
Skeletal muscle index
References
El-Khoueiry AB, Sangro B, Yau T, Crocenzi TS, Kudo M, Hsu C et al (2017) Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet 389(10088):2492–2502. https://doi.org/10.1016/s0140-6736(17)31046-2
Yau T, Park JW, Finn RS, Cheng AL, Mathurin P, Edeline J et al (2019) CheckMate 459: A randomized, multi-center phase III study of nivolumab (NIVO) vs sorafenib (SOR) as first-line (1L) treatment in patients (pts) with advanced hepatocellular carcinoma (aHCC). Ann Oncol 30:v874–v875. https://doi.org/10.1093/annonc/mdz394.029
Roubenoff R (2003) Sarcopenia: effects on body composition and function. J Gerontol A Biol Sci Med Sci 58(11):1012–1017. https://doi.org/10.1093/gerona/58.11.m1012
Bilen MA, Martini DJ, Liu Y, Shabto JM, Brown JT, Williams M et al (2019) Combined effect of sarcopenia and systemic inflammation on survival in patients with advanced stage cancer treated with immunotherapy. Oncologist. https://doi.org/10.1634/theoncologist.2019-0751
Dercle L, Ammari S, Champiat S, Massard C, Ferté C, Taihi L et al (2016) Rapid and objective CT scan prognostic scoring identifies metastatic patients with long-term clinical benefit on anti-PD-1/-L1 therapy. Eur J Cancer 65:33–42. https://doi.org/10.1016/j.ejca.2016.05.031
Yu JI, Lee SJ, Lee J, Lim HY, Paik SW, Yoo GS, Choi C, Park HC (2019) Clinical significance of radiotherapy before and/or during nivolumab treatment in hepatocellular carcinoma. Cancer Med 8(16):6986–6994. https://doi.org/10.1002/cam4.2570
Kim N, Cheng J, Jung I, Liang J, Shih YL, Huang WY et al (2020) Stereotactic body radiation therapy vs. radiofrequency ablation in Asian patients with hepatocellular carcinoma. J Hepatol. https://doi.org/10.1016/j.jhep.2020.03.005
Korean Liver Cancer A, National Cancer C (2019) 2018 Korean liver cancer association-national cancer center korea practice guidelines for the management of hepatocellular carcinoma. Gut Liver 13(3):227–299. https://doi.org/10.5009/gnl19024
Rim CH, Seong J (2016) Application of radiotherapy for hepatocellular carcinoma in current clinical practice guidelines. Radiat Oncol J 34(3):160–167. https://doi.org/10.3857/roj.2016.01970
Choi C, Yoo GS, Cho WK, Park HC (2019) Optimizing radiotherapy with immune checkpoint blockade in hepatocellular carcinoma. World J Gastroenterol 25(20):2416–2429. https://doi.org/10.3748/wjg.v25.i20.2416
Nishikawa H, Shiraki M, Hiramatsu A, Moriya K, Hino K, Nishiguchi S (2016) Japan Society of Hepatology guidelines for sarcopenia in liver disease (1st edition): recommendation from the working group for creation of sarcopenia assessment criteria. Hepatol Res 46(10):951–963. https://doi.org/10.1111/hepr.12774
Templeton AJ, McNamara MG, Šeruga B, Vera-Badillo FE, Aneja P, Ocaña A et al (2014) Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst 106(6):dju124. https://doi.org/10.1093/jnci/dju124
Feliciano EMC, Kroenke CH, Meyerhardt JA, Prado CM, Bradshaw PT, Kwan ML et al (2017) Association of systemic inflammation and sarcopenia with survival in nonmetastatic colorectal cancer: results from the C SCANS study. JAMA Oncol 3(12):e172319. https://doi.org/10.1001/jamaoncol.2017.2319
Daly LE, Power DG, O’Reilly Á, Donnellan P, Cushen SJ, O’Sullivan K, Twomey M, Woodlock DP, Redmond HP, Ryan AM (2017) The impact of body composition parameters on ipilimumab toxicity and survival in patients with metastatic melanoma. Br J Cancer 116(3):310–317. https://doi.org/10.1038/bjc.2016.431
Heidelberger V, Goldwasser F, Kramkimel N, Jouinot A, Huillard O, Boudou-Rouquette P et al (2017) Sarcopenic overweight is associated with early acute limiting toxicity of anti-PD1 checkpoint inhibitors in melanoma patients. Invest New Drugs 35(4):436–441. https://doi.org/10.1007/s10637-017-0464-x
Shiroyama T, Nagatomo I, Koyama S, Hirata H, Nishida S, Miyake K et al (2019) Impact of sarcopenia in patients with advanced non-small cell lung cancer treated with PD-1 inhibitors: a preliminary retrospective study. Sci Rep 9(1):2447. https://doi.org/10.1038/s41598-019-39120-6
Cortellini A, Bozzetti F, Palumbo P, Brocco D, Di Marino P, Tinari N et al (2020) Weighing the role of skeletal muscle mass and muscle density in cancer patients receiving PD-1/PD-L1 checkpoint inhibitors: a multicenter real-life study. Sci Rep 10(1):1456. https://doi.org/10.1038/s41598-020-58498-2
Cortellini A, Verna L, Porzio G, Bozzetti F, Palumbo P, Masciocchi C et al (2019) Predictive value of skeletal muscle mass for immunotherapy with nivolumab in non-small cell lung cancer patients: a “hypothesis-generator” preliminary report. Thorac Cancer 10(2):347–351. https://doi.org/10.1111/1759-7714.12965
Waning DL, Mohammad KS, Reiken S, Xie W, Andersson DC, John S et al (2015) Excess TGF-β mediates muscle weakness associated with bone metastases in mice. Nat Med 21(11):1262–1271. https://doi.org/10.1038/nm.3961
Flint TR, Janowitz T, Connell CM, Roberts EW, Denton AE, Coll AP, Jodrell DI, Fearon DT (2016) Tumor-Induced IL-6 reprograms host metabolism to suppress anti-tumor immunity. Cell Metab 24(5):672–684. https://doi.org/10.1016/j.cmet.2016.10.010
Mariathasan S, Turley SJ, Nickles D, Castiglioni A, Yuen K, Wang Y et al (2018) TGFβ attenuates tumour response to PD-L1 blockade by contributing to exclusion of T cells. Nature 554(7693):544–548. https://doi.org/10.1038/nature25501
Tsukamoto H, Fujieda K, Miyashita A, Fukushima S, Ikeda T, Kubo Y, Senju S, Ihn H, Nishimura Y, Oshiumi H (2018) Combined blockade of IL6 and PD-1/PD-L1 signaling abrogates mutual regulation of their immunosuppressive effects in the tumor microenvironment. Cancer Res 78(17):5011–5022. https://doi.org/10.1158/0008-5472.Can-18-0118
Elias R, Hartshorn K, Rahma O, Lin N, Snyder-Cappione JE (2018) Aging, immune senescence, and immunotherapy: a comprehensive review. Semin Oncol 45(4):187–200. https://doi.org/10.1053/j.seminoncol.2018.08.006
Nelke C, Dziewas R, Minnerup J, Meuth SG, Ruck T (2019) Skeletal muscle as potential central link between sarcopenia and immune senescence. EBioMedicine 49:381–388. https://doi.org/10.1016/j.ebiom.2019.10.034
Dodson S, Baracos VE, Jatoi A, Evans WJ, Cella D, Dalton JT, Steiner MS (2011) Muscle wasting in cancer cachexia: clinical implications, diagnosis, and emerging treatment strategies. Annu Rev Med 62:265–279. https://doi.org/10.1146/annurev-med-061509-131248
Capone M, Giannarelli D, Mallardo D, Madonna G, Festino L, Grimaldi AM et al (2018) Baseline neutrophil-to-lymphocyte ratio (NLR) and derived NLR could predict overall survival in patients with advanced melanoma treated with nivolumab. J Immunother Cancer 6(1):74. https://doi.org/10.1186/s40425-018-0383-1
Ménétrier-Caux C, Ray-Coquard I, Blay JY, Caux C (2019) Lymphopenia in cancer patients and its effects on response to immunotherapy: an opportunity for combination with cytokines? J Immunother Cancer 7(1):85. https://doi.org/10.1186/s40425-019-0549-5
Ho WJ, Yarchoan M, Hopkins A, Mehra R, Grossman S, Kang H (2018) Association between pretreatment lymphocyte count and response to PD1 inhibitors in head and neck squamous cell carcinomas. J Immunother Cancer 6(1):84. https://doi.org/10.1186/s40425-018-0395-x
Diehl A, Yarchoan M, Hopkins A, Jaffee E, Grossman SA (2017) Relationships between lymphocyte counts and treatment-related toxicities and clinical responses in patients with solid tumors treated with PD-1 checkpoint inhibitors. Oncotarget 8(69):114268–114280. https://doi.org/10.18632/oncotarget.23217
Cho Y, Park S, Byun HK, Lee CG, Cho J, Hong MH et al (2019) Impact of treatment-related lymphopenia on immunotherapy for advanced non-small cell lung cancer. Int J Radiat Oncol Biol Phys 105(5):1065–1073. https://doi.org/10.1016/j.ijrobp.2019.08.047
Bagley SJ, Kothari S, Aggarwal C, Bauml JM, Alley EW, Evans TL et al (2017) Pretreatment neutrophil-to-lymphocyte ratio as a marker of outcomes in nivolumab-treated patients with advanced non-small-cell lung cancer. Lung Cancer 106:1–7. https://doi.org/10.1016/j.lungcan.2017.01.013
Dharmapuri S, Özbek U, Lin JY, Schwartz M, Branch A, Ang C (2019) Predictive value of neutrophil–lymphocyte ratio (NLR) and platelet–lymphocyte ratio (PLR) In hepatocellular carcinoma (HCC) patients treated with nivolumab (N). Ann Oncol 30:v285–v286. https://doi.org/10.1093/annonc/mdz247.071
Formenti SC, Demaria S (2009) Systemic effects of local radiotherapy. Lancet Oncol 10(7):718–726. https://doi.org/10.1016/S1470-2045(09)70082-8
Weichselbaum RR, Liang H, Deng L, Fu YX (2017) Radiotherapy and immunotherapy: a beneficial liaison? Nat Rev Clin Oncol 14(6):365–379. https://doi.org/10.1038/nrclinonc.2016.211
Venkatesulu BP, Mallick S, Lin SH, Krishnan S (2018) A systematic review of the influence of radiation-induced lymphopenia on survival outcomes in solid tumors. Crit Rev Oncol Hematol 123:42–51. https://doi.org/10.1016/j.critrevonc.2018.01.003
Kang C, Jeong S-Y, Song SY, Choi EK (2020) The emerging role of myeloid-derived suppressor cells in radiotherapy. Radiat Oncol J 38(1):1–10. https://doi.org/10.3857/roj.2019.00640
Newton JM, Hanoteau A, Liu H-C, Gaspero A, Parikh F, Gartrell-Corrado RD et al (2019) Immune microenvironment modulation unmasks therapeutic benefit of radiotherapy and checkpoint inhibition. J Immunother Cancer 7(1):216–216. https://doi.org/10.1186/s40425-019-0698-6
Funding
This study was partly supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2017R1D1A1B03031275).
Author information
Authors and Affiliations
Contributions
Conception, design, data collection, interpretation, and drafting of the manuscript were performed by NK and JIY. Data collection and interpretation were performed by HCP, GSY, CC, JYH, HYL, JL, and MSC. Statistical analysis and editing of the manuscript were performed by JEL and KK. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval
This study was approved by the Health Institutional Review Boards of Samsung Medical Center (No. 2020–03-012).
Consent to participate
The requirement for informed consent was waived because of the retrospective nature of this study.
Consent for publication
The requirement for informed consent was waived because of the retrospective nature of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kim, N., Yu, J.I., Park, H.C. et al. Incorporating sarcopenia and inflammation with radiation therapy in patients with hepatocellular carcinoma treated with nivolumab. Cancer Immunol Immunother 70, 1593–1603 (2021). https://doi.org/10.1007/s00262-020-02794-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-020-02794-3