Abstract
Purpose
To evaluate the accuracy of the usual MRI diagnostic patterns of primary liver lesions applied to the diagnosis of pathologically proven fat-containing liver lesions.
Materials and Methods
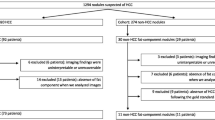
This monocentric IRB approved retrospective study included all patients with pathologically proven focal liver lesions and documented intra-tumoral fat on pathology and who underwent preoperative liver MRI for characterization. Both liver morphology and usual lesion MRI features were analyzed and their distribution correlated to the final pathological result (Khi-2 or Fisher exact tests, Student t-test or Mann–Whitney U test, as appropriate). The Sensitivity (Se) and Specificity (Sp) of MRI patterns known to be associated to both Hepatocellular Carcinoma (HCC), Focal Nodular Hyperplasia (FNH), and Hepatocellular Adenoma (HCA) subtypes were evaluated.
Results
Between March 2014 and November 2021, 66 lesions were included, corresponding to: 26 HCC, 32 HCA, 6 FNH and 2 hepatic angiomyolipoma (HAML). All lesions developed on a dysmorphic liver were HCC. A non-rim arterial phase hyperenhancement with a washout and an enhancing capsule had a 98% specificity for HCC diagnosis; A homogeneous dropout of signal on the opposed phase had a sensitivity of 92% and a specificity of 89% for the diagnosis of HNF1alpha inactivated subtype of HCA (HHCA). The FNH pattern was specific at 100% for the diagnosis of FNH with a 40% Se. Finally, the accuracy of inflammatory hepatocellular adenoma (IHCA) pattern had a low 60% Se but a high 89% Sp for IHCA diagnosis.
Conclusion
Known MRI patterns remain reliable for the accurate diagnosis of primary liver tumors on MRI even in fat-containing lesions.
Graphical abstract






Similar content being viewed by others
References
Prasad, S.R., et al., Fat-containing lesions of the liver: radiologic-pathologic correlation. Radiographics, 2005. 25(2): p. 321-31.
Hamer, O.W., et al., Fatty liver: imaging patterns and pitfalls. Radiographics, 2006. 26(6): p. 1637-53.
Chung, A.D., Fat-Containing Lesions of the Liver: A Review of Differential Diagnoses. Can Assoc Radiol J, 2020. 71(1): p. 12-18.
Costa, A.F., et al., Fat-Containing Liver Lesions on Imaging: Detection and Differential Diagnosis. AJR Am J Roentgenol, 2018. 210(1): p. 68-77.
Tekath, M., et al., Fat-containing lesions of the liver: a pictorial essay. Diagn Interv Imaging, 2015. 96(2): p. 201-11.
Vij, M. and J. Calderaro, Pathologic and molecular features of hepatocellular carcinoma: An update. World J Hepatol, 2021. 13(4): p. 393-410.
Nault, J.C., et al., Molecular Classification of Hepatocellular Adenoma Associates With Risk Factors, Bleeding, and Malignant Transformation. Gastroenterology, 2017. 152(4): p. 880-894.e6.
Bello, H.R., et al., Hepatocellular Carcinoma With Atypical Imaging Features: Review of the Morphologic Hepatocellular Carcinoma Subtypes With Radiology-Pathology Correlation. J Magn Reson Imaging, 2021.
Nault, J.C., et al., Molecular classification of hepatocellular adenoma in clinical practice. J Hepatol, 2017. 67(5): p. 1074-1083.
European Association for the Study of the Liver. Electronic address, e.e.e. and L. European Association for the Study of the, EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol, 2018. 69(1): p. 182–236.
Chernyak, V., et al., Liver Imaging Reporting and Data System (LI-RADS) Version 2018: Imaging of Hepatocellular Carcinoma in At-Risk Patients. Radiology, 2018. 289(3): p. 816-830.
Lee, S.J., et al., Hepatic Angiomyolipoma Versus Hepatocellular Carcinoma in the Noncirrhotic Liver on Gadoxetic Acid-Enhanced MRI: A Diagnostic Challenge. AJR Am J Roentgenol, 2016. 207(3): p. 562-70.
Ronot, M., et al., Hepatocellular adenomas: accuracy of magnetic resonance imaging and liver biopsy in subtype classification. Hepatology, 2011. 53(4): p. 1182-91.
Laumonier, H., et al., Hepatocellular adenomas: magnetic resonance imaging features as a function of molecular pathological classification. Hepatology, 2008. 48(3): p. 808-18.
Ronot, M., et al., MR findings of steatotic focal nodular hyperplasia and comparison with other fatty tumours. Eur Radiol, 2013. 23(4): p. 914-23.
Calderaro, J., et al., Histological subtypes of hepatocellular carcinoma are related to gene mutations and molecular tumour classification. J Hepatol, 2017. 67(4): p. 727-738.
Cree, I.A.C.i.d.r.s.l.c.O.m.d.l.s., WHO classification of tumours of the digestive system. 2019.
Brunt, E.M., et al., NAFLD: Reporting Histologic Findings in Clinical Practice. Hepatology, 2021. 73(5): p. 2028-2038.
Krishna, M., Histological Grading and Staging of Chronic Hepatitis. Clin Liver Dis (Hoboken), 2021. 17(4): p. 222-226.
Lafortune, M., et al., Segment 4 (the quadrate lobe): a barometer of cirrhotic liver disease at US. Radiology, 1998. 206(1): p. 157-60.
Awaya, H., et al., Cirrhosis: modified caudate-right lobe ratio. Radiology, 2002. 224(3): p. 769-74.
Bise, S., et al., New MRI features improve subtype classification of hepatocellular adenoma. Eur Radiol, 2019. 29(5): p. 2436-2447.
Ronot, M. and V. Vilgrain, Imaging of benign hepatocellular lesions: current concepts and recent updates. Clin Res Hepatol Gastroenterol, 2014. 38(6): p. 681-8.
Koo, T.K. and M.Y. Li, A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med, 2016. 15(2): p. 155-63.
Cassidy, F.H., et al., Fatty liver disease: MR imaging techniques for the detection and quantification of liver steatosis. Radiographics, 2009. 29(1): p. 231-60.
Rajlawot, K., et al., Accuracies of Chemical Shift In/Opposed Phase and Chemical Shift Encoded Magnetic Resonance Imaging to Detect Intratumoral Fat in Hepatocellular Carcinoma. J Magn Reson Imaging, 2021. 53(6): p. 1791-1802.
Marrero, J.A., et al., Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology, 2018. 68(2): p. 723-750.
Silva, A.C., et al., MR imaging of hypervascular liver masses: a review of current techniques. Radiographics, 2009. 29(2): p. 385-402.
Nakayama, T., et al., Fat in liver metastasis from renal cell carcinoma detected by chemical shift MR imaging. Abdom Imaging, 2003. 28(5): p. 657-9.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Reizine, E., Meurgey, A., Amaddeo, G. et al. Fat in mass in primary liver lesions: are usual MRI diagnostic criteria of both malignant and benign liver lesions still applicable?. Abdom Radiol 47, 2347–2355 (2022). https://doi.org/10.1007/s00261-022-03561-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-022-03561-x