Abstract
Purpose
The purpose of the study was to retrospectively analyze whether double-echo gradient-echo (GRE) chemical shift imaging (CSI) can differentiate between pancreatic metastases from clear cell renal cell carcinoma (PM-ccRCC) and pancreatic neuroendocrine tumor (pNET).
Methods
Institutional review board approval and informed consent were waived. CSI, T2WI, DWI, and DCE magnetic resonance imaging (MRI) were performed in patients with PM-ccRCC and pNET. Eleven patients with PM-ccRCC and 24 patients with pNET were enrolled into this retrospective study. The signal intensity was measured in the pancreatic tumor and spleen on in-phase and opposed-phase images. The signal intensity index (SII) and tumor-to-spleen ratio (TSR) in PM-ccRCC and pNET were calculated and compared. Receiver operating characteristic (ROC) analysis was performed to evaluate the diagnostic accuracy of SII and TSR in the differentiation between PM-ccRCC and pNET.
Results
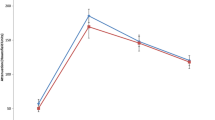
The SII between PM-ccRCC and pNET (20.3% ± 16.8% vs. − 3.2% ± 11.4%) was significantly different (P < 0.001), as was the TSR (− 19.2% ± 16.6% vs. 6.0% ± 13.8%) (P < 0.001). The area under the ROC curve was 0.917 for the SII and 0.902 for the TSR. Additionally, an SII threshold value of 8.1% permitted the differentiation of PM-ccRCC from pNET with a sensitivity of 90.9%, a specificity of 91.7%, a positive predictive value of 90.1%, a negative predictive value of 91.7%, and an accuracy of 91.4%. A TSR cut-off value of − 4.7% enabled the differentiation of the two groups with a sensitivity of 79.2%, a specificity of 90.9%, a positive predictive value of 90.9%, a negative predictive value of 79.2% and an accuracy of 82.9%.
Conclusion
Double-echo GRE chemical shift MR imaging can accurately differentiate between PM-ccRCC and pNET.






Similar content being viewed by others
References
Crippa S, Angelini C, Mussi C, et al. (2006) Surgical treatment of metastatic tumors to the pancreas: a single center experience and review of the literature. World J Surg 30(8):1536–1542. https://doi.org/10.1007/s00268-005-0464-4
Zerbi A, Ortolano E, Balzano G, et al. (2008) Pancreatic metastasis from renal cell carcinoma: which patients benefit from surgical resection? Ann Surg Oncol 15(4):1161–1168. https://doi.org/10.1245/s10434-007-9782-0
Ballarin R, Spaggiari M, Cautero N, et al. (2011) Pancreatic metastases from renal cell carcinoma: the state of the art. World J Gastroenterol 17(43):4747–4756. https://doi.org/10.3748/wjg.v17.i43.4747
Klein KA, Stephens DH, Welch TJ (1998) CT characteristics of metastatic disease of the pancreas. Radiographics 18(2):369–378. https://doi.org/10.1148/radiographics.18.2.9536484
Sperti C, Moletta L, Patane G (2014) Metastatic tumors to the pancreas: the role of surgery. World J Gastroint Oncol 6(10):381–392. https://doi.org/10.4251/wjgo.v6.i10.381
Tsitouridis I, Diamantopoulou A, Michaelides M, Arvanity M, Papaioannou S (2010) Pancreatic metastases: CT and MRI findings. Diag Interven Radiol 16(1):45–51. https://doi.org/10.4261/1305-3825.DIR.1996-08.1
Hijioka S, Hifumi M, Mekky MA, et al. (2010) Total pancreatectomy for metastatic renal cell carcinoma with marked extension into the main pancreatic duct. Intern Med 49(6):557–562
Thompson LD, Heffess CS (2000) Renal cell carcinoma to the pancreas in surgical pathology material. Cancer 89(5):1076–1088
Sellner F, Tykalsky N, De Santis M, Pont J, Klimpfinger M (2006) Solitary and multiple isolated metastases of clear cell renal carcinoma to the pancreas: an indication for pancreatic surgery. Ann Surg Oncol 13(1):75–85. https://doi.org/10.1245/ASO.2006.03.064
Palmowski M, Hacke N, Satzl S, et al. (2008) Metastasis to the pancreas: characterization by morphology and contrast enhancement features on CT and MRI. Pancreatology 8(2):199–203. https://doi.org/10.1159/000128556
Kang TW, Kim SH, Lee J, et al. (2015) Differentiation between pancreatic metastases from renal cell carcinoma and hypervascular neuroendocrine tumour: use of relative percentage washout value and its clinical implication. Eur J Radiol 84(11):2089–2096. https://doi.org/10.1016/j.ejrad.2015.08.007
Lee LC, Grant CS, Salomao DR, et al. (2012) Small, nonfunctioning, asymptomatic pancreatic neuroendocrine tumors (PNETs): role for nonoperative management. Surgery 152(6):965–974. https://doi.org/10.1016/j.surg.2012.08.038
Rosenberg AM, Friedmann P, Del Rivero J, Libutti SK, Laird AM (2016) Resection versus expectant management of small incidentally discovered nonfunctional pancreatic neuroendocrine tumors. Surgery 159(1):302–309. https://doi.org/10.1016/j.surg.2015.10.013
Ozkan E, Soydal C, Ucak Semirgin S, et al. (2016) Early Response to Everolimus Therapy Detected on 68 Ga-DOTATATE PET/CT in a Patient With Pancreatic Neuroendocrine Tumor. Clin Nucl Med 41(7):561–563. https://doi.org/10.1097/RLU.0000000000001242
Soler A, Figueiredo AM, Castel P, et al. (2016) Therapeutic benefit of selective inhibition of p110alpha PI3-kinase in pancreatic neuroendocrine tumors. Clin Cancer Res . https://doi.org/10.1158/1078-0432.CCR-15-3051
Cros J, Hentic O, Rebours V, et al. (2016) MGMT expression predicts response to temozolomide in pancreatic neuroendocrine tumors. Endocr Relat Cancer 23(8):625–633. https://doi.org/10.1530/ERC-16-0117
Cheng SK, Chuah KL (2016) Metastatic renal cell carcinoma to the pancreas: a review. Arch Pathol Lab Med 140(6):598–602. https://doi.org/10.5858/arpa.2015-0135-RS
Reddy S, Edil BH, Cameron JL, et al. (2008) Pancreatic resection of isolated metastases from nonpancreatic primary cancers. Ann Surg Oncol 15(11):3199–3206. https://doi.org/10.1245/s10434-008-0140-7
Tanis PJ, van der Gaag NA, Busch OR, van Gulik TM, Gouma DJ (2009) Systematic review of pancreatic surgery for metastatic renal cell carcinoma. Br J Surg 96(6):579–592. https://doi.org/10.1002/bjs.6606
Hosokawa Y, Kinouchi T, Sawai Y, et al. (2002) Renal angiomyolipoma with minimal fat. Int J Clin Oncol 7(2):120–123. https://doi.org/10.1007/s101470200016
Jhaveri KS, Elmi A, Hosseini-Nik H, et al. (2015) Predictive value of chemical-shift MRI in distinguishing clear cell renal cell carcinoma from non-clear cell renal cell carcinoma and minimal-fat angiomyolipoma. AJR Am J Roentgenol 205(1):W79–86. https://doi.org/10.2214/AJR.14.13245
Haider MA, Ghai S, Jhaveri K, Lockwood G (2004) Chemical shift MR imaging of hyperattenuating (> 10 HU) adrenal masses: does it still have a role? Radiology 231(3):711–716. https://doi.org/10.1148/radiol.2313030676
Jackson A, O’Connor JP, Parker GJ, Jayson GC (2007) Imaging tumor vascular heterogeneity and angiogenesis using dynamic contrast-enhanced magnetic resonance imaging. Clin Cancer Res 13(12):3449–3459. https://doi.org/10.1158/1078-0432.CCR-07-0238
Maurea S, Imbriaco M, D’Angelillo M, et al. (2006) Diagnostic accuracy of chemical-shift MR imaging to differentiate between adrenal adenomas and non adenoma adrenal lesions. Radiol Med 111(5):674–686. https://doi.org/10.1007/s11547-006-0065-9
Carucci LR, Siegelman ES, Feldman MD (1999) Pancreatic metastasis from clear cell renal carcinoma: diagnosis with chemical shift MRI. J Comput Assist Tomogr 23(6):934–936
Koyama H, Maruta T, Kudo T, Mayahara H, Yoshida K (2005) Multiple pancreatic metastases from clear cell renal carcinoma: diagnosis with chemical shift magnetic resonance imaging before surgery. Australas Radiol 49(6):493–496. https://doi.org/10.1111/j.1440-1673.2005.01471.x
Kim JK, Kim SH, Jang YJ, et al. (2006) Renal angiomyolipoma with minimal fat: differentiation from other neoplasms at double-echo chemical shift FLASH MR imaging. Radiology 239(1):174–180. https://doi.org/10.1148/radiol.2391050102
Ferre R, Cornelis F, Verkarre V, et al. (2015) Double-echo gradient chemical shift MR imaging fails to differentiate minimal fat renal angiomyolipomas from other homogeneous solid renal tumors. Eur J Radiol 84(3):360–365. https://doi.org/10.1016/j.ejrad.2014.11.040
Wente MN, Kleeff J, Esposito I, et al. (2005) Renal cancer cell metastasis into the pancreas: a single-center experience and overview of the literature. Pancreas 30(3):218–222
Merkle EM, Nelson RC (2006) Dual gradient-echo in-phase and opposed-phase hepatic MR imaging: a useful tool for evaluating more than fatty infiltration or fatty sparing. Radiographics 26(5):1409–1418. https://doi.org/10.1148/rg.265055711
Reuter VE (2006) The pathology of renal epithelial neoplasms. Semin Oncol 33(5):534–543. https://doi.org/10.1053/j.seminoncol.2006.06.009
Reuter VE, Tickoo SK (2010) Differential diagnosis of renal tumours with clear cell histology. Pathology 42(4):374–383. https://doi.org/10.3109/00313021003785746
Charlesworth M, Verbeke CS, Falk GA, et al. (2012) Pancreatic lesions in von Hippel-Lindau disease? A systematic review and meta-synthesis of the literature. J Gastroint Surg 16(7):1422–1428. https://doi.org/10.1007/s11605-012-1847-0
Kassabian A, Stein J, Jabbour N, et al. (2000) Renal cell carcinoma metastatic to the pancreas: a single-institution series and review of the literature. Urology 56(2):211–215
Gala-Lopez BL, Semlacher E, Manouchehri N, Kin T, Shapiro AM (2013) Autologous islet transplantation after total pancreatectomy for renal cell carcinoma metastases. Am J Transplant 13(9):2487–2491. https://doi.org/10.1111/ajt.12354
Bassi C, Butturini G, Falconi M, et al. (2003) High recurrence rate after atypical resection for pancreatic metastases from renal cell carcinoma. Br J Surg 90(5):555–559. https://doi.org/10.1002/bjs.4072
Ascenti G, Visalli C, Genitori A, et al. (2004) Multiple hypervascular pancreatic metastases from renal cell carcinoma: dynamic MR and spiral CT in three cases. Clin Imaging 28(5):349–352. https://doi.org/10.1016/S0899-7071(03)00198-0
Fukukura Y, Shindo T, Higashi M, et al. (2015) Computed tomography and magnetic resonance imaging features of lipid-rich neuroendocrine tumors of the pancreas. World J Gastroenterol 21(34):10008–10017. https://doi.org/10.3748/wjg.v21.i34.10008
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by National Natural Science Foundation of China (Grant No. 81471641).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Lyu, Hl., Cao, Jx., Wang, Hy. et al. Differentiation between pancreatic metastases from clear cell renal cell carcinoma and pancreatic neuroendocrine tumor using double-echo chemical shift imaging. Abdom Radiol 43, 2712–2720 (2018). https://doi.org/10.1007/s00261-018-1539-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1539-7