Abstract
Purpose
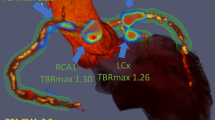
18F-sodium fluoride (18F-NaF) has shown promise in assessing disease activity in coronary arteries, but currently used measures of activity – such as maximum target to background ratio (TBRmax) – are defined by single pixel count values. We aimed to develop a novel coronary-specific measure of 18F-NaF PET reflecting activity throughout the entire coronary vasculature (coronary microcalcification activity [CMA]).
Methods
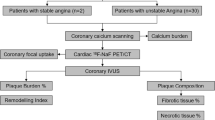
Patients with recent myocardial infarction and multi-vessel coronary artery disease underwent 18F-NaF PET and coronary CT angiography. We assessed the association between coronary 18F-NaF uptake (both TBRmax and CMA) and coronary artery calcium scores (CACS) as well as low attenuation plaque (LAP, attenuation < 30 Hounsfield units) volume.
Results
In 50 patients (64% males, 63 ± 7 years), CMA and TBRmax were higher in vessels with LAP compared to those without LAP (1.09 [0.02, 2.34] versus 0.0 [0.0, 0.0], p < 0.001 and 1.23 [1.16, 1.37] versus 1.04 [0.93, 1.11], p < 0.001). Compared to a TBRmax threshold of 1.25, CMA > 0 had a higher diagnostic accuracy for detection of LAP: sensitivity of 93.1 (83.3–98.1)% versus 58.6 (44.9–71.4)% and a specificity of 95.7 (88.0–99.1)% versus 80.0 (68.7–88.6)% (both p < 0.001).
18F-NaF uptake assessed by CMA correlated more closely with LAP (r = 0.86, p < 0.001) than the CT calcium score (r = 0.39, p < 0.001), with these associations outperforming those observed for TBRmax values (LAP r = 0.63, p < 0.001; CT calcium score r = 0.30, p < 0.001).
Conclusions
Automated assessment of disease activity across the entire coronary vasculature is feasible using 18F-NaF CMA, providing a single measurement that has closer agreement with CT markers of plaque vulnerability than more traditional measures of plaque activity.





Similar content being viewed by others
Abbreviations
- CAD:
-
Coronary artery disease
- CMA:
-
Coronary microcalcification activity
- CI:
-
Confidence intervals
- CT:
-
Computed tomography
- PET:
-
Positron emission tomography
- SD:
-
Standard deviation
- SUVmax:
-
Maximum standard uptake value
- TBRma:
-
Maximum target to background ratio
- 18F-NaF:
-
18F-sodium fluoride
References
Go AS, Mozaffarian D, Roger VL, for theAmerican Heart Association Statistics Committee and Stroke Statistics Subcommittee, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292.
Arbab-Zadeh A, Fuster V. The Myth of the “Vulnerable Plaque”. J Am Coll Cardiol. 2015;65(8):846–55. https://doi.org/10.1016/j.jacc.2014.11.041.
Dweck MR, Aikawa E, Newby DE, Tarkin JM, Rudd JH, Narula J, et al. Noninvasive molecular imaging of disease activity in atherosclerosis. Circ Res. 2016;119:330–40. https://doi.org/10.1161/CIRCRESAHA.116.307971.
Stone GW, Maehara A, Lansky AJ, et al. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364:226–35. https://doi.org/10.1056/NEJMoa1002358.
Calvert PA, Obaid DR, O’Sullivan M, et al. Association between IVUS findings and adverse outcomes in patients with coronary artery disease: the VIVA (VH-IVUS in vulnerable atherosclerosis) study. JACC Cardiovasc Imaging. 2011;4:894–901. https://doi.org/10.1016/j.jcmg.2011.05.005.
Williams MC, Moss AJ, Dweck M, et al. Coronary artery plaque characteristics associated with adverse outcomes in the SCOT-HEART study. J Am Coll Cardiol. 2019;73:291–301.
Ferencik M, Mayrhofer T, Bittner DO, et al. Use of high-risk coronary atherosclerotic plaque detection for risk stratification of patients with stable chest pain: a secondary analysis of the PROMISE randomized clinical trial. JAMA Cardiol. 2018;3:144–52.
Nerlekar N, Ha FJ, Cheshire C, Rashid H, et al. Computed tomographic coronary angiography–derived plaque characteristics predict major adverse cardiovascular events: a systematic review and meta-analysis. Circ Cardiovasc Imaging. 2018;10:e006973. https://doi.org/10.1161/CIRCIMAGING.117.006973.
Rudd JHF, Warburton EA, Fryer TD, et al. Imaging atherosclerotic plaque inflammation with F-18 -fluorodeoxyglucose positron emission tomography. Circulation. 105(23):2708–11. https://doi.org/10.1161/01.cir.0000020548.60110.76.
Tarkin JM, Joshi FR, Evans NR, et al. Detection of Atherosclerotic Inflammation by (68)Ga-DOTATATE PET Compared to [(18)F]FDG PET Imaging. J Am Coll Cardiol. 69(14):1774–91. https://doi.org/10.1016/j.jacc.2017.01.060.
Joshi NV, Vesey AT, Williams MC, et al. F-18-fluoride positron emission tomography for identification of ruptured and high-risk coronary atherosclerotic plaques: a prospective clinical trial. Lancet. 383(9918):705–13. https://doi.org/10.1016/s0140-6736(13)61754-7.
Bellinge JW, Francis RJ, Majeed K, et al. In search of the vulnerable patient or the vulnerable plaque: (18)F-sodium fluoride positron emission tomography for cardiovascular risk stratification. J Nucl Cardiol. 2018. https://doi.org/10.1007/s12350-018-1360-2.
Beheshti M, Saboury B, Mehta N. Detection and global quantification of cardiovascular molecular calcification by fluoro-18-fluoride positron emission tomography/computed tomography—a novel concept. Hell J Nucl Med. 2011;14:114–20.
Blomberg BA, Thomassen A, de Jong PA, et al. Impact of personal characteristics and technical factors on quantification of sodium 18F-fluoride uptake in human arteries: prospective evaluation of healthy subjects. J Nucl Med. 2015;56:1534–40.
Kwiecinski J, Adamson PD, Lassen ML, et al. Feasibility of coronary 18F-sodium fluoride PET assessment with the utilization of previously acquired CT angiography. Circ Cardiovasc Imaging. 2018;11(12):e008325.
Leipsic J, Abbara S, Achenbach S, Cury R, Earls JP, Mancini GJ, et al. SCCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. JCCT. 2014;8:342–58.
Rubeaux M, Joshi N, Dweck MR, et al. Motion correction of 18F-sodium fluoride PET for imaging coronary atherosclerotic plaques. J Nucl Med Soc Nuclear Med. 2015. https://doi.org/10.2967/jnumed.115.162990.
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–32.
Hell MM, Motwani M, Otaki Y, et al. Quantitative global plaque characteristics from coronary computed tomography angiography for the prediction of future cardiac mortality during long-term follow-up. Eur Heart J Cardiovasc Imaging. 2017;18:1331–9.
Massera D, Doris MK, Cadet S, et al. Analytical quantification of aortic valve 18F-sodium fluoride PET uptake. J Nucl Cardiol. 2018. https://doi.org/10.1007/s12350-018-01542-6.
Doris MK, Otaki Y, Krishnan SK, Kwiecinski J, Rubeaux M, Alessio A et al. Optimization of reconstruction and quantification of motion-corrected coronary PET-CT. J Nucl Cardiol 2018.
Rahim MK, Kim SE, So H, et al. Recent Trends in PET Image Interpretations Using Volumetric and Texture-based Quantification Methods in Nuclear Oncology. Nucl Med Mol Imaging. 48(1):1–15. https://doi.org/10.1007/s13139-013-0260-2.
Steven ML, Yusuf E, Timothy A, et al. Tumor Treatment Response Based on Visual and Quantitative Changes in Global Tumor Glycolysis Using PET-FDG Imaging: The Visual Response Score and the Change in Total Lesion Glycolysis. Clin Positron Imaging. 2(3):159–71.
Ahmadian A, Brogan A, Berman J, et al. Quantitative interpretation of FDG PET/CT with myocardial perfusion imaging increases diagnostic information in the evaluation of cardiac sarcoidosis. J Nucl Cardiol. 2014;21:925–39. https://doi.org/10.1007/s12350-014-9901-9.
Kwiecinski J, Dey D, Cadet S, et al. Predictors of 18F-sodium fluoride uptake in patients with stable coronary artery disease and adverse plaque features on computed tomography angiography. Eur Heart J Cardiovasc Imaging. 2019. https://doi.org/10.1093/ehjci/jez152.
Forsythe RO, Dweck MR, McBride OMB, et al. F-18-Sodium Fluoride Uptake in Abdominal Aortic Aneurysms The SoFIA(3) Study. J Am Coll Cardiol. 71(5):513–23. https://doi.org/10.1016/j.jacc.2017.11.053.
Han JH, Lim SY, Lee MS, et al. Sodium [18F]fluoride PET/CT in myocardial infarction. Mol Imaging Biol. 2015;17:214–21.
Giovanna Trivieri M, Dweck MR, Abgral R, Robson PM, et al. 18F-sodium fluoride PET/MR for the assessment of cardiac amyloidosis. J Am Coll Cardiol. 2016;68:2712–4.
Marchesseau S, Seneviratna A, Sjoholm AT, et al. Hybrid PET/CT and PET/MRI imaging of vulnerable coronary plaque and myocardial scar tissue in acute myocardial infarction. J Nucl Cardiol. 2017.
Chen HHW, Chiu N-T. Su W-Cet al. Prognostic value of whole-body total lesion glycolysis at pretreatment FDG PET/CT in non–small cell lung cancer. Radiology. 2012;264(2):559–66.
Frings V, van Velden FHP, Velasquez LM, et al. Repeatability of metabolically active tumor volume measurements with FDG PET / CT in advanced gastrointestinal malignancies: a multicenter study. Radiology. 2014;273(2):539–48.
Kramer GM, Frings V, Hoetjes N, et al. Repeatability of quantitative whole-body 18F-FDG PET/CT uptake measures as function of uptake interval and lesion selection in non-small cell lung cancer patients. J Nucl Med. 2016;57(9):1343–9.
Lee P, Weerasuriya DK, Lavori PW, et al. Metabolic tumor burden predicts for disease progression and death in lung cancer. Int J Radiat Oncol Biol Phys. 2007;69(2):328–33.
La TH, Filion EJ, Turnbull BB, et al. Metabolic tumor volume predicts for recurrence and death in head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2009;74(5):1335–41.
Kwiecinski J, Berman DS, Lee SE et al. 2018 Three-hour delayed imaging improves assessment of coronary 18F-sodium fluoride PET. J Nucl Me jnumed.118.217885 published ahead of print September 13.
Funding
This research was supported in part by grants R01HL135557 and R01HL133616 from the National Heart, Lung, and Blood Institute/National Institute of Health (NHLBI/NIH) and by a grant from the Dr. Miriam & Sheldon G. Adelson Medical Research Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This research is also supported by a grant from the Dr. Miriam & Sheldon G. Adelson Medical Research Foundation. Data analysis was supported by a grant from Siemens Medical Systems.
Other author relationshipsDEN (CH/09/002, RE/13/3/30183) and MRD (FS/14/78/31020) are also supported by the British Heart Foundation. DEN is the recipient of a Wellcome Trust Senior Investigator Award (WT103782AIA) and MRD of Sir Jules Thorn Award for Biomedical Research Award (2015).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All other authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardiology
Electronic supplementary material
ESM 1
(DOCX 3581 kb)
Rights and permissions
About this article
Cite this article
Kwiecinski, J., Cadet, S., Daghem, M. et al. Whole-vessel coronary 18F-sodium fluoride PET for assessment of the global coronary microcalcification burden. Eur J Nucl Med Mol Imaging 47, 1736–1745 (2020). https://doi.org/10.1007/s00259-019-04667-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-019-04667-z