Abstract
Objective
Pseudotumors, a well-known complication of metal-on-metal total hip arthroplasty (MoM THA), are well identified on metal artifact-reducing sequences magnetic resonance imaging (MARS-MRI). Several MRI grading systems are described in the orthopedic literature, but their validity is unknown in large clinical studies. Our study was undertaken to describe the classification of pseudotumors in a preselected cohort divided into high- and low-risk patients, using three pseudotumor grading systems applied on MARS-MRI, and to determine the interobserver reliability of the grading systems.
Patients and methods
A retrospective study was performed on 377 consecutive patients (240 MRI scans) treated with an M2a-38 and Taperloc stem combination (Biomet, Warsaw, IN, USA). Patients were divided into a high-risk and a low-risk group based on previous published risk factors. Two observers determined the presence of pseudotumors using three different pseudotumor grading systems for classifying MARS-MRI results.
Results
The prevalence of pseudotumors as determined with MARS-MRI was 59% in our high-risk group, 0% in the low-risk group and 43% in the control group. Serum cobalt values were increased in the high-risk group. The kappa values of the Anderson, Hauptfleisch and Matthies grading system scores were 0.43, 0.44, and 0.49 respectively.
Conclusions
High-risk patients are at a high risk for pseudotumor development. No pseudotumor development was found in low-risk patients. Interobserver reliability scored best with the Matthies system, but all three grading systems showed only a moderate agreement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Concerns have been raised on the use of metal-on-metal total hip arthroplasty (MoM THA) because of frequent early revision rates [1], raised cobalt and chrome serum levels in the blood and their possible toxicological effects [2], and the occurrence of cystic and/or solid massed, or so-called pseudotumors, in the periprosthetic tissue [3]. Recent studies show that the incidence of pseudotumors is comparable with other THA systems such as cobalt on polyethylene and metal on polyethylene [4, 5]. MoM THA-induced pseudotumors can cause compression of the neurovascular bundle [6, 7]. This had also been described for conventional THA, although this pseudotumor compression was associated with a broken or worn-out inlay, which induces a MoM reaction [8, 9]. A possible explanation could be that the MoM reaction stimulates the formation of pseudotumors with a larger mass than those observed in conventional THA, although recent research rejected this suggestion [4]. Associations between the presence of a pseudotumor and serum cobalt levels have been described [10]. High local cobalt values may induce pseudotumor formation and are known to cause osteolysis [11]. Risk factors for the formation of a pseudotumor are cobalt >5 μg/l [10], female gender [12, 13], pain [14], and a high inclination angle >55° [15]. Despite the observed associations and risk factors, the exact mechanism of THA-induced pseudotumors is still unclear. Pseudotumors are well defined on MRI and three grading systems have been described in the orthopedic literature by Anderson [16], Matthies [17], and Hauptfleisch [3]. Table 1 provides details of the scoring systems.
Van der Weegen et al. [18] described kappa values for all three classification systems (49 hips) and Chang et al. [14] describes a kappa for the Anderson classification (192 hips). Importantly, other radiological studies on pseudotumors do not report a kappa value and therefore the results should be interpreted with caution [3, 19,20,21]. The reproducibility of these grading systems is of clinical importance and may help to unravel the etiology of a pseudotumor.
The aims of this study were to describe the classification of pseudotumors in a preselected cohort by utilizing metal artifact-reducing sequences magnetic resonance imaging (MARS-MRI) in a high-risk and low-risk group for pseudotumor development, and to study the interobserver reliability of three different pseudotumor grading systems in a large single cohort of MoM THA (240 hips).
Patients and methods
Our investigation reviewed 377 uncemented MoM THA performed in our institution between February 2008 and January 2011. In all cases, a cobalt and chromium bearing couple consisting of a monoblock acetabular cup with a 38-mm fixed size head design was implanted (M2a-38; Biomet, Warsaw, IN, USA). The cup size ranged from 48 mm to 64 mm. All patients received a press-fit titanium femoral stem (Taperloc, Biomet, Warsaw, IN, USA).
All patients were subjected to a pre-defined screening protocol, which was initiated after the first concerns of the MoM THA. The clinical results of this screening were reported recently [22]. In the current study, all patients with an MoM THA and available MARS-MRI were selected.
Screening protocol
Patients received a standardized outpatient consultation. This included physical examination, patient-reported questionnaires, blood analysis for serum cobalt, radiographs of the hip and pelvis, and magnetic resonance imaging (MRI). Contrast-enhanced MRI of the hip region with MARS was performed in patients with osteolysis on the X-ray, elevated serum metal ion levels above 5 μg/l, or pain. Patients without these criteria received routine annual follow-up, which was the same as the first screening.
Pain was defined as the presence or absence of any pain in the hip area reported by the patient.
Cobalt and chromium ion levels were determined in the serum with the use of an AAnalyst 800 Atomic Absorption Spectrophotometer (Perkin Elmer, Waltham, MA, USA). The blood samples were collected in a metal-free container. Serum cobalt levels ranging from 0.04 to 0.64 μg/l are considered normal in the general population [23]. Cobalt serum levels higher than 5 μg/l were defined as elevated in MoM THA [2]. Inclination was measured on the 6-week post-operative X-ray. The observer who performed the measurements had shown good reliability for measuring post-operative cup inclination angle (ICC = 0.74, p = <0.001) in a previous study (Smeekes et al., accepted for publication)
Patients were divided into three groups based on the likelihood of developing a pseudotumor: one group was supposed to have a high risk for developing a pseudotumor based on the literature. Selection criteria for the high-risk group were: serum cobalt >5 μg/l [10], female sex [12, 13], hip pain [14] and a high cup inclination angle >45°, which is considered to be out of the safe zone in resurfacing prosthesis [16, 24]. Inclusion criteria for the low-risk group were the opposing criteria (male sex, no hip pain, cup inclination <45°, and serum cobalt <5 μg/l). All other patients were used as the control group.
For a description of the pseudotumors, the Anderson classification [16], the classification of Matthies [17], and the Hauptfleisch classification were used [3]. Also, a list of other findings on the MRI scan that are not reported in these scores is shown (Table 1). An experienced musculoskeletal radiologist and a musculoskeletal radiologist in training independently scored the MRI scans. The radiologists applied all grading systems at the same time. Kappa values were compared for each grading system. Discordant cases were discussed and consensus was obtained for the classification system with the best kappa values.
For the MRI scans, an MRI scanner with a field strength of 1.5 Tesla was used. The following MARS-MRI sequences were used: T1-weighted coronal plane with echo time (TE) 16 ms, repetition time (TR) 450–650 ms, slices (SL) 2.5 mm, field-of-view (FOV) 36 × 37.1, and bandwidth (BW) 435 Hz/pixel; T2-weighted coronal plane with TE 80 ms, TR 3,500–7,000 ms, SL 2.5 mm, FOV 36 × 45, and BW 435 Hz/pixel; T2-weighted short tau inversion recovery (STIR) coronal plane with TE 40 ms, TR shortest ms, SL 3.5 mm, FOV 36 × 45, and BW 435.5 Hz/pixel.
The scientific committee of the Leiden University Medical Centre and the ethics committee in the Meander Medical Centre waived ethical approval.
Statistical analyses
Descriptive analyses were performed on baseline data and final outcomes. The results are expressed as means with standard deviations or medians with ranges where relevant. Reliability of the radiological measurements was evaluated by calculating interclass correlation coefficients using Cohen’s kappa. The differences among the cobalt values in the pseudotumor classification group were analyzed using post-hoc tests in a one-way ANOVA after logarithmic transformation of the cobalt values because of the skewed (positive) distribution of these values. Chi-squared test was used for the analyses of gender and pain between the pseudotumor classifications. Fisher’s test was used to analyze the difference between the presence of a pseudotumor in the high- and low-risk groups. A t test was used for comparing the serum cobalt levels in patients in the control group with and without a pseudotumor. For all tests, a two-tailed significance level of 0.05 was used. SPSS software (version 20; IBM, Armonk, NY, USA) was used for the analyses.
Results
A total of 240 patients with an M2a-38 and Taperloc stem combination (Biomet, Warsaw, IN, USA) were eligible for analyses. Demographics and reason for surgery are listed in Table 2. Seventy-five patients had bilateral prostheses: all 75 had prostheses of the M2a-38 type with a Taperloc stem and were included in the study. The contralateral hip prostheses were of different types and were not included in the study. Twenty-three patients had a bilateral M2a-38 prosthesis and Taperloc stem (=46 M2a-38) combination and 119 patients had a unilateral MoM prosthesis of the M2a-38 type and a Taperloc stem (=119 M2a-38).
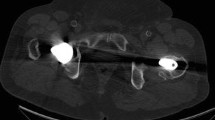
Classification of the pseudotumors
In this single cohort of MoM THA hips, observer 1 identified 107 pseudotumors (44.6%) and observer 2 identified 96 pseudotumors (40%) regardless of the grading system used. Observer 1 identified: 46 type C1, 58 type C2, and 3 type C3 pseudotumors using the Anderson grading system. Using the Matthies grading system, observer 1 identified: 32 type 1, 62 type 2a, 1 type 2b, and 12 type 3 pseudotumors. With the use of the Hauptfleisch grading, 62 type 1, 32 type 2, and 13 type 3 pseudotumors were classified. (Fig. 1; Table 3) Observer 2 identified: 16 type C1, 65 type C2, and 15 type C3 pseudotumors using the Anderson grading system. Using the Matthies grading system observer 2 identified 1 type 1, 85 type 2a, 1 type 2b, and 9 type 3 pseudotumors. With the use of the Hauptfleisch grading, 63 type 1, 24 type 2, and 9 type 3 pseudotumors were classified by observer 2 (Fig. 2; Table 3). Interobserver reliability on whether a pseudotumor was present or not was 0.56 (p = <0.001). Interobserver reliability for pseudotumor severity with the Anderson, Matthies, and Hauptfleisch grading systems was 0.43 (p = <0.001), 0.49 (p = <0.001), and 0.44 (p = <0.001) respectively. In our cohort, the Matthies score was the most reliable classification (Table 4).
A 17% complete agreement between observer 1 and observer 2 was reached for Anderson C1, 68% for Anderson C2, and 6% for Anderson C3. For the Matthies system, 3% complete agreement between observer 1 and observer 2 was reached for grade 1, 73% for grade 2a, 100% for grade 2b, and 75% for grade 3. For the Hauptfleisch system, 48% complete agreement between observer 1 and observer 2 was reached for grade 1, 53% for grade 2, and 39% for grade 3.
The Matthies grading system was discordant for the results of 70 scans. Observer 1 scored 21, no pseudotumors, whereas observer 2 scored the same scans as follows: 1 grade 1, 18 grade 2a, and 2 grade 3 pseudotumors. Observer 1 scored 32 scans as a grade 1 pseudotumor and observer 2 scored 23 as having no pseudotumor, whereas only 9 were scored as grade 1 pseudotumor. Observer 1 scored 10 grade 2a pseudotumors where observer 2 scored 8 no pseudotumors and 2 grade 3 pseudotumors. Lastly, observer 1 scored 7 scans as a grade 3 pseudotumor whereas observer 2 scored 1 no pseudotumor and 6 grade 2a pseudotumors.
A bursa filled with fluid (without connection with the joint) was found for 25.8% cases by observer 1 and for 24.2% of the cases by observer 2. Atrophy of the gluteus medius and minimus muscles was scored by observer 1 in 90 cases, whereas observer 2 scored 39 cases as positive. Atrophy of the gluteus medius muscle was found in 72 of the cases by observer 1 and in 16 cases by observer 2.
After the consensus, 106 pseudotumors were diagnosed with the use of the Matthies grading system. Type 2a pseudotumor was the most frequent classification (Fig. 3). Patients with a type 2a pseudotumor had a mean serum cobalt of 13.1 μg/l (SD 23.7). Thirty-eight of these patients had pain and 61 were female. After the logarithmic transformation of the cobalt values, a significant difference could be observed between the group of patients without a pseudotumor and the group of patients with a type 1 or 2a pseudotumor (p < 0.05), and also between a type 1 pseudotumor versus a type 2a pseudotumor (p < 0.05) or type 3 pseudotumor (p < 0.05) respectively. No difference between the pseudotumor classification and pain or gender could be detected (Table 5). Of the 106 pseudotumors, 52 were asymptomatic (49%). There was no difference between the presence of a pseudotumor in the symptomatic patients (54 out of 118) compared with the asymptomatic patients (52 out of 122; p = 0.62; Table 6). Regarding categories of pseudotumor wall thickness (no wall, <3 mm or ≥3 mm), there were no differences between the symptomatic and asymptomatic patients (Table 5).
High- and low-risk patient screening
After classification of pseudotumors according to the Matthies grading, patients were divided in a high-risk group for pseudotumor development, a low-risk group, and a control group. A significantly higher risk was found for pseudotumor development in the high-risk group (59%, 20 out of 34) versus the low-risk group (0%, 0 out of 5; p < 0.001). In the control group, 86 pseudotumors were diagnosed in 201 THAs (43%). The patients in the control group with a pseudotumor had a mean serum cobalt of 8.3 μg/l (SD 6.6 μg/l) and patients in the control group without a pseudotumor had a mean serum cobalt level of 7.8 μg/l (SD 7.5 μg/l; p = 0.61).
A difference was found between cobalt serum values and high- and low-risk patients. No differences were found in the control group between patients with a pseudotumor and those without a pseudotumor with regard to serum cobalt levels. No significant differences in the type of pseudotumor, pain, and gender were found among the groups. Also, no differences in the control group were found between symptomatic and asymptomatic patients.
Discussion
As far as we know, this is one of the largest series of MoM THA in which patients were screened for having a pseudotumor by utilizing MARS-MRI [25]. A total of 106 pseudotumors were diagnosed after consensus in 240 MoM THAs (44%), of which 49% had no symptoms. In the low-risk patient group (male sex, no hip pain, cup inclination <45°, and serum cobalt <5 μg/l), no pseudotumors were diagnosed, whereas a high percentage of pseudotumors (59%, 20 out of 34) was found in the high-risk patient group (serum cobalt >5 μg/l [10], female sex, hip pain, and a high cup inclination angle >45°). However, the control group also showed a high percentage of pseudotumors (43%, 86 out of 201). The high-risk group showed a significantly higher risk of developing a pseudotumor.
A higher cobalt level is also correlated with different levels of pseudotumors. One may hypothesize that a (local) higher cobalt level influences the formation of a pseudotumor; however, several studies show that cobalt values are a poor predictor [17, 26, 27]. In the literature, it is reported that the existence of a pseudotumor varies by type of prosthesis. In large-head MoM prosthesis patients, 40–60% of the patients develop a pseudotumor [10, 28, 29]. Our cohort results agree to these findings. Other studies showed that the prevalence of pseudotumors in conventional THA ceramics on polyethylene and metal on polyethylene is comparable with MoM THA [4, 5], but they are less symptomatic and revisions due to pseudotumors are rare in non-MoM THA. More patients with MoM THA report pain compared with patients with conventional THA [30], which may be caused by the local toxicity of the cobalt, hypersensitivity reactions on the metal release, subsequent osteolysis, and soft-tissue damage [22, 31]. Chang et al. reports that soft-tissue damage is associated with pain and not the presence or size of a pseudotumor [14]. The behavior of pseudotumors in the long term is unclear.
A high complication rate (14%) in MoM revision surgery has been reported, with a 7% re-revision rate after 2 years (range: 26–52 months) [32] and a dislocation rate of up to 28% [33,34,35]. Three of the studies used a posterior approach and one study used a posterior approach in 80% of the cases and in 20% an anterolateral approach. The exact reason for the higher luxation rate after these revisions is not clear, but all authors suggest that the extensive destruction of soft tissue caused by the MoM prosthesis might play an important role. Atrophy of the gluteal musculature and subsequent instability may contribute to the high dislocation rate. In the case of symptomatic patients, MARS-MRI can be used as a preoperative tool to classify the damage of the soft tissue before revision and add to decision-making to choose a dual mobility cup to lower the dislocation rate [36].
To the best of our knowledge, only one study has reported the interobserver reliability among the three grading systems [18]. In this study, the highest kappa (0.58) was found for the Anderson grading system. In our study, the highest kappa (0.49) was found for the Matthies classification, 0.44 for the Anderson classification, and 0.43 for the Hauptfleisch classification. Although this study included a larger cohort of patients compared with van der Weegen et al., a lower kappa value was measured. We do not have an explanation for this, but in both studies, there was only moderate agreement, which questions the reproducibility and thus clinical use. Another difference is that we only used the M2a-38 system and in the other study, three different systems had been used. A shortcoming of the study is that the MARS-MRI scored all grading systems at the same time, which can create a “cross-contamination” of results. The low kappa value of the Anderson score can be partly explained by the inclusion of more parameters of periprosthetic tissue compared with the Matthies and Hauptfleisch scores, which only score the characteristics of the pseudotumor.
Compression by a pseudotumor on the neurovascular bundle, soft-tissue damage, and osteolysis aid in the clinical decision-making whether to revise or not.
In conclusion, a higher occurrence of pseudotumor development in high-risk patients was found. No pseudotumor development was found in low-risk patients. However, patients in the control group also showed a high occurrence of pseudotumors. This means that every patient, except those defined as “low risk,” is at a substantial risk for developing a pseudotumor. No differences were found in the control group between patients with a pseudotumor and those without a pseudotumor with regard to serum cobalt levels. The Matthies score was the most reliable classification, but all three grading systems showed limited interobserver reliability. MARS-MRI is one of the tools that aids in clinical decision-making regarding revision MoM THA, but whether or not a pseudotumor grading system should be used, or if so, which one, is still under debate.
References
Smith AJ, Dieppe P, Vernon K, Porter M, Blom AW. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet. 2012;379(9822):1199–204.
Hart AJ, Sabah SA, Bandi AS, Maggiore P, Tarassoli P, Sampson B, et al. Sensitivity and specificity of blood cobalt and chromium metal ions for predicting failure of metal-on-metal hip replacement. J Bone Joint Surg Br. 2011;93(10):1308–13.
Hauptfleisch J, Pandit H, Grammatopoulos G, Gill HS, Murray DW, Ostlere S. A MRI classification of periprosthetic soft tissue masses (pseudotumours) associated with metal-on-metal resurfacing hip arthroplasty. Skeletal Radiol. 2012;41(2):149–55.
Bisseling P, de Wit BW, Hol AM, van Gorp MJ, van Kampen A, van Susante JL. Similar incidence of periprosthetic fluid collections after ceramic-on-polyethylene total hip arthroplasties and metal-on-metal resurfacing arthroplasties: results of a screening metal artefact reduction sequence-MRI study. Bone Joint J. 2015;97-B(9):1175–82.
Nikolaou VS, Petit A, Khoury V, Blain-Pare E, Zukor DJ, Huk OL, et al. Magnetic resonance imaging of painful metal-on-metal total hip replacement. Eur J Orthop Surg Traumatol. 2015;25(2):313–9.
Abdel-Hamid H, Miles J, Carrington RW, Hart A, Loh A, Skinner JA. Combined vascular and orthopaedic approach for a pseudotumor causing deep vein thrombosis after metal-on-metal hip resurfacing arthroplasty. Case Rep Orthop. 2015;2015:926263.
Clayton RA, Beggs I, Salter DM, Grant MH, Patton JT, Porter DE. Inflammatory pseudotumor associated with femoral nerve palsy following metal-on-metal resurfacing of the hip. A case report. J Bone Joint Surg Am. 2008;90(9):1988–93.
Fischer SR, Christ DJ, Roehr BA. Sciatic neuropathy secondary to total hip arthroplasty wear debris. J Arthroplast. 1999;14(6):771–4.
Fokter SK, Repse-Fokter A, Takac I. Case report: femoral neuropathy secondary to total hip arthroplasty wear debris. Clin Orthop Relat Res. 2009ss;467(11):3032–5.
Bosker BH, Ettema HB, Boomsma MF, Kollen BJ, Maas M, Verheyen CC. High incidence of pseudotumour formation after large-diameter metal-on-metal total hip replacement: a prospective cohort study. J Bone Joint Surg Br. 2012;94(6):755–61.
Keegan GM, Learmonth ID, Case CP. A systematic comparison of the actual, potential, and theoretical health effects of cobalt and chromium exposures from industry and surgical implants. Crit Rev Toxicol. 2008;38(8):645–74.
Langton DJ, Jameson SS, Joyce TJ, Hallab NJ, Natu S, Nargol AV. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: a consequence of excess wear. J Bone Joint Surg Br. 2010;92(1):38–46.
Moroni A, Savarino L, Hoque M, Cadossi M, Baldini N. Do ion levels in hip resurfacing differ from metal-on-metal THA at midterm? Clin Orthop Relat Res. 2011;469(1):180–7.
Chang EY, McAnally JL, Van Horne JR, Statum S, Wolfson T, Gamst A, et al. Metal-on-metal total hip arthroplasty: do symptoms correlate with MR imaging findings? Radiology. 2012;265(3):848–57.
Hart AJ, Muirhead-Allwood S, Porter M, Matthies A, Ilo K, Maggiore P, et al. Which factors determine the wear rate of large-diameter metal-on-metal hip replacements? Multivariate analysis of two hundred and seventy-six components. J Bone Joint Surg Am. 2013;95(8):678–85.
Anderson H, Toms AP, Cahir JG, Goodwin RW, Wimhurst J, Nolan JF. Grading the severity of soft tissue changes associated with metal-on-metal hip replacements: reliability of an MR grading system. Skeletal Radiol. 2011;40(3):303–7.
Matthies AK, Skinner JA, Osmani H, Henckel J, Hart AJ. Pseudotumors are common in well-positioned low-wearing metal-on-metal hips. Clin Orthop Relat Res. 2012;470(7):1895–906.
Van der Weegen W, Brakel K, Horn RJ, Wullems JA, Das HP, Pilot P, et al. Comparison of different pseudotumor grading systems in a single cohort of metal-on-metal hip arthroplasty patients. Skeletal Radiol. 2014;43(2):149–55.
Bisseling P, de Wit BW, Hol AM, van Gorp MJ, van K A, van Susante JL. Similar incidence of periprosthetic fluid collections after ceramic-on-polyethylene total hip arthroplasties and metal-on-metal resurfacing arthroplasties: results of a screening metal artefact reduction sequence-MRI study. Bone Joint J. 2015;97-B(9):1175–82.
Nawabi DH, Gold S, Lyman S, Fields K, Padgett DE, Potter HG. MRI predicts ALVAL and tissue damage in metal-on-metal hip arthroplasty. Clin Orthop Relat Res. 2014;472(2):471–81.
Reito A, Elo P, Puolakka T, Pajamaki J, Nieminen J, Eskelinen A. Repeated magnetic resonance imaging in 154 hips with large-diameter metal-on-metal hip replacement. Acta Orthop. 2014;85(6):570–6.
Smeekes C, Ongkiehong B, van der Wal B, Wolterbeek R, Henseler JF, Nelissen R. Large fixed-size metal-on-metal total hip arthroplasty: higher serum metal ion levels in patients with pain. Int Orthop. 2015;39(4):631–8.
Goulle JP, Mahieu L, Castermant J, Neveu N, Bonneau L, Laine G, et al. Metal and metalloid multi-elementary ICP-MS validation in whole blood, plasma, urine and hair. Reference values. Forensic Sci Int. 2005;153(1):39–44.
Langton DJ, Joyce TJ, Jameson SS, Lord J, Van OM, Holland JP, et al. Adverse reaction to metal debris following hip resurfacing: the influence of component type, orientation and volumetric wear. J Bone Joint Surg Br. 2011;93(2):164–71.
Reito A, Elo P, Nieminen J, Puolakka T, Eskelinen A. Gluteal muscle fatty atrophy is not associated with elevated blood metal ions or pseudotumors in patients with a unilateral metal-on-metal hip replacement. Acta Orthop. 2016;87(1):29–35.
Bayley N, Khan H, Grosso P, Hupel T, Stevens D, Snider M, et al. What are the predictors and prevalence of pseudotumor and elevated metal ions after large-diameter metal-on-metal THA? Clin Orthop Relat Res. 2015;473(2):477–84.
Bosker BH, Ettema HB. Van RM, Boomsma MF, Kollen BJ, Maas M, et al. Pseudotumor formation and serum ions after large head metal-on-metal stemmed total hip replacement. Risk factors, time course and revisions in 706 hips. Arch Orthop Trauma Surg. 2015;135(3):417–25.
Hart AJ, Satchithananda K, Liddle AD, Sabah SA, McRobbie D, Henckel J, et al. Pseudotumors in association with well-functioning metal-on-metal hip prostheses: a case-control study using three-dimensional computed tomography and magnetic resonance imaging. J Bone Joint Surg Am. 2012;94(4):317–25.
Williams DH, Greidanus NV, Masri BA, Duncan CP, Garbuz DS. Prevalence of pseudotumor in asymptomatic patients after metal-on-metal hip arthroplasty. J Bone Joint Surg Am. 2011;93(23):2164–71.
Nikolajsen L, Brandsborg B, Lucht U, Jensen TS, Kehlet H. Chronic pain following total hip arthroplasty: a nationwide questionnaire study. Acta Anaesthesiol Scand. 2006;50(4):495–500.
Gill HS, Grammatopoulos G, Adshead S, Tsialogiannis E, Tsiridis E. Molecular and immune toxicity of CoCr nanoparticles in MoM hip arthroplasty. Trends Mol Med. 2012;18(3):145–55.
Liow MH, Dimitriou D, Tsai TY, Kwon YM. Preoperative risk factors associated with poor outcomes of revision surgery for "pseudotumors" in patients with metal-on-metal hip arthroplasty. J Arthroplast. 2016;31(12):2835–42.
De Smet KA, Van Der Straeten C, Van O M, Doubi R, Backers K, Grammatopoulos G. Revisions of metal-on-metal hip resurfacing: lessons learned and improved outcome. Orthop Clin North Am. 2011;42(2):259–69. ix
Grammatopoulos G, Pandit H, Kwon YM, Gundle R, McLardy-Smith P, Beard DJ, et al. Hip resurfacings revised for inflammatory pseudotumour have a poor outcome. J Bone Joint Surg Br. 2009;91(8):1019–24.
Munro JT, Masri BA, Duncan CP, Garbuz DS. High complication rate after revision of large-head metal-on-metal total hip arthroplasty. Clin Orthop Relat Res. 2014;472(2):523–8.
Mohaddes M, Cnudde P, Rolfson O, Wall A, Karrholm J. Use of dual-mobility cup in revision hip arthroplasty reduces the risk for further dislocation: analysis of seven hundred and ninety one first-time revisions performed due to dislocation, reported to the Swedish Hip Arthroplasty Register. Int Orthop. 2017;41(3):583–8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Smeekes, C., Schouten, B.J.M., Nix, M. et al. Pseudotumor in metal-on-metal hip arthroplasty: a comparison study of three grading systems with MRI. Skeletal Radiol 47, 1099–1109 (2018). https://doi.org/10.1007/s00256-018-2873-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-018-2873-0