Abstract
Background
No previous research papers have reported a comparative survey of local radiologic diagnoses and central review in children with hepatoblastoma.
Objective
To evaluate the utility of central review of children with hepatoblastoma enrolled in a clinical trial.
Materials and methods
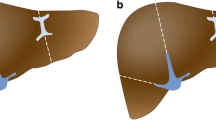
The study included 91 children enrolled in a clinical trial conducted by the Japanese Study Group for Pediatric Liver Tumor. We compared the results of the initial pre-treatment extent of tumor (PRETEXT) disease staging performed at local sites with the results obtained on central review to determine the concurrence rates for tumor staging and additional criteria.
Results
The concurrence rate for PRETEXT staging was 70%. As the stage increased, the concurrence rate decreased. Using additional criteria, central review identified 143 lesions (157.1%), about 1.8 times higher than the number identified for the local site diagnoses. The additional criterion found most often on central review was “multifocal lesion” (n=19). The concurrence rate for lung metastases was high. However, our central review found many false-positive assertions of hepatic vein lesions, portal vein invasion and extrahepatic lesions among the local site diagnoses.
Conclusion
In a clinical trial of hepatoblastoma, central review provided a more precise diagnosis than local site diagnoses with respect to severe PRETEXT stages III and IV cases and other cases including hepatic and portal vein invasion. The central review process appears to be effective and essential for improving the quality of clinical trials.





Similar content being viewed by others
References
Pugmire BS, Towbin AJ (2016) Magnetic resonance imaging of primary pediatric liver tumors. Pediatr Radiol 46:764–777
Hiyama E, Hishiki T, Watanabe K et al (2020) Outcome and late complications of hepatoblastomas treated using the Japanese Study Group for Pediatric Liver Tumor 2 protocol. J Clin Oncol 38:2488–2498
Towbin AJ, Meyers RL, Woodley H et al (2018) 2017 PRETEXT: radiologic staging system for primary hepatic malignancies of childhood revised for the Paediatric Hepatic International Tumour Trial (PHITT). Pediatr Radiol 48:536–554
MacKinlay GA, Pritchard J (1992) A common language for childhood liver tumours. Pediatr Surg Int 7:325–326
Pritchard J, Brown J, Shafford E et al (2000) Cisplatin, doxorubicin, and delayed surgery for childhood hepatoblastoma: a successful approach — results of the first prospective study of the International Society of Pediatric Oncology. J Clin Oncol 18:3819–3828
Roebuck DJ, Aronson D, Clapuyt P et al (2007) 2005 PRETEXT: a revised staging system for primary malignant liver tumours of childhood developed by the SIOPEL group. Pediatr Radiol 37:123–132
Smith EA (2019) The Children’s Oncology Group: an opportunity for pediatric radiologists. Pediatr Radiol 49:1382–1383
Hamilton TE, Barnhart D, Gow K (2013) Inter-rater reliability of surgical reviews for AREN03B2: a COG renal tumor committee study. J Pediatr Surg 49:154–158
Rodriguez D, Chambers T, Warmuth-Metz M et al (2019) Evaluation of the implementation of the response assessment in neuro-oncology criteria in the HERBY trial of pediatric patients with newly diagnosed high-grade gliomas. AJNR Am J Neuroradiol 40:568–575
Shi Y, Su H, Song Y (2019) Safety and activity of sintilimab in patients with relapsed or refractory classical Hodgkin lymphoma (ORIENT-1): a multicentre, single-arm, phase 2 trial. Lancet Haematol 6:e12–e19
Yoon HM, Hwang J, Kim KW (2019) Prognostic factors for event-free survival in pediatric patients with hepatoblastoma based on the 2017 PRETEXT and CHIC-HS systems. Cancers 11:1387
Zsiros J, Brugieres L, Brock P et al (2013) Dose-dense cisplatin-based chemotherapy and surgery for children with high-risk hepatoblastoma (SIOPEL-4): a prospective, single-arm, feasibility study. Lancet Oncol 14:834–842
Maibach R, Roebuck D, Brugieres L et al (2012) Prognostic stratification for children with hepatoblastoma: the SIOPEL experience. Eur J Cancer 48:1543–1549
Watanabe K (2013) Current chemotherapeutic approaches for hepatoblastoma. J Clin Oncol 18:955–961
Hishiki T, Watanabe K, Ida K et al (2017) The role of pulmonary metastasectomy for hepatoblastoma in children with metastasis at diagnosis: results from the JPLT-2 study. J Pediatr Surg 52:2051–2055
Meyers RL, Katzenstein HM, Krailo M et al (2007) Surgical resection of pulmonary metastatic lesions in children with hepatoblastoma. J Pediatr Surg 42:2050–2056
Meyers AB, Towbin AJ, Geller JI et al (2012) Hepatoblastoma imaging with gadoxetate disodium-enhanced MRI — typical, atypical, pre- and post-treatment evaluation. Pediatr Radiol 42:859–866
Tajiri T, Kimura O, Fumino S et al (2012) Surgical strategies for unresectable hepatoblastomas. J Pediatr Surg 47:2194–2198
Sakamoto S, Kasahara M, Mizuta K et al (2014) Nationwide survey of the outcomes of living donor liver transplantation for hepatoblastoma in Japan. Liver Transpl 20:333–346
Watanabe K, Mori M, Hishiki T et al (2021) Feasibility of dose-dense cisplatin-based chemotherapy in children with high-risk hepatoblastoma: analysis of the JPLT-3-H pilot study. Pediatr Blood Cancer 66:s66–s67
Acknowledgments
The authors would like to thank Dr. Yoshitomo Matsuo and Ban Asatsuma for technical support with respect to a cloud-based teleradiology system (Esite Healthcare Co., Tokyo, Japan). The authors appreciate the contributions made by all of the physician members of the Japan Children’s Cancer Group (JCCG) and liver tumor committee. We thank Mrs. Hiroe Saito, Mrs. Rika Kashihara and Mrs. Minako Mase for office work in the radiology committee of the JCCG. This work was supported by the Japan Agency for Medical Research and Development (AMED) under grant numbers 17ck0106332h, 20ck0106609h and 20lk0201066h, and the Japanese Society for the Promotion of Science (JSPS KAKENHI) under grant number JP16H02778.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miyazaki, O., Oguma, E., Nishikawa, M. et al. Usefulness of central radiologic review in clinical trials of children with hepatoblastoma. Pediatr Radiol 53, 367–377 (2023). https://doi.org/10.1007/s00247-022-05530-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-022-05530-4