Abstract
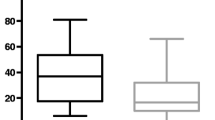
Protein-losing enteropathy (PLE) is a rare but potentially devastating complication of single-ventricle physiology after the Fontan operation. Although abnormal bone mineral density (BMD) is a known complication of chronic disease and congenital heart disease, no reports have described BMD in patients with PLE. This study investigated a cross-sectional sample of children and young adults with a confirmed diagnosis of PLE. Serum levels of 25(OH)D, calcium, total protein, and albumin were recorded from the first outpatient encounter with each subject. Corrected calcium (cCa) was calculated from the serum calcium and albumin levels. Dual-energy X-ray absorptiometry (DXA) was used to measure BMD, and z-scores were generated using appropriate software. DXA results were available for 12 patients (eight males and four females). The age at DXA ranged from 7.2 to 25.2 years. The mean z-score was −1.73 standard deviation (SD) for the entire cohort, with 42 % z-scores below −2 SDs. Serum 25(OH)D levels were abnormal in 58 % of the patients. There was a positive correlation between cCa and DXA z-score and a negative correlation between total protein and DXA z-score. Patients receiving corticosteroid therapy had a significantly lower DXA z-score than those not receiving corticosteroids (−3.15 vs. −0.31; p = 0.02). Children with PLE are at risk for abnormal BMD compared with age- and sex-matched control subjects. In the study cohort, corticosteroid exposure, a marker of disease severity, appeared to be associated with decreased BMD. Routine bone health screening is warranted for children with PLE, particularly those receiving corticosteroid therapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Ali T, Lam D, Bronze MS, Humphrey MB (2009) Osteoporosis in inflammatory bowel disease. Am J Med 122:599–604
Cohen MI, Bush DM, Ferry RJ Jr, Spray TL, Moshang T Jr, Wernovsky G et al (2000) Somatic growth failure after the Fontan operation. Cardiol Young 10:447–457
Cohen MS, Zak V, Atz AM, Printz BF, Pinto N, Lambert L et al (2010) Anthropometric measures after Fontan procedure: implications for suboptimal functional outcome. Am Heart J 160:1092–1098, 1098.e1
Donnelly JP, Rosenthal A, Castle VP, Holmes RD (1997) Reversal of protein-losing enteropathy with heparin therapy in three patients with univentricular hearts and Fontan palliation. J Pediatr 130:474–478
Fontan F, Baudet E (1971) Surgical repair of tricuspid atresia. Thorax 26:240–248
Goldberg DJ, Dodds K, Rychik J (2010) Rare problems associated with the Fontan circulation. Cardiol Young 20(Suppl 3):113–119
Goldberg DJ, Shaddy RE, Ravishankar C, Rychik J (2011) The failing Fontan: etiology, diagnosis, and management. Expert Rev Cardiovasc Ther 9:785–793
John AS, Phillips SD, Driscoll DJ, Warnes CA, Cetta F (2011) The use of octreotide to successfully treat protein-losing enteropathy following the Fontan operation. Congenit Heart Dis 6:653–656
John AS, Driscoll DJ, Warnes CA, Phillips SD, Cetta F (2011) The use of oral budesonide in adolescents and adults with protein-losing enteropathy after the Fontan operation. Ann Thorac Surg 92:1451–1456
Kreutzer G, Galindez E, Bono H, De Palma C, Laura JP (1973) An operation for the correction of tricuspid atresia. J Thorac Cardiovasc Surg 66:613–621
Mertens L, Hagler DJ, Sauer U, Somerville J, Gewillig M (1998) Protein-losing enteropathy after the Fontan operation: an international multicenter study. PLE study group. J Thorac Cardiovasc Surg 115:1063–1073
O’Brien CA, Jia D, Plotkin LI, Bellido T, Powers CC, Stewart SA et al (2004) Glucocorticoids act directly on osteoblasts and osteocytes to induce their apoptosis and reduce bone formation and strength. Endocrinology 145:1835–1841
Osteoporosis prevention, diagnosis, and therapy (2000). NIH Consens Statement 17:1–45
Rychik J (2007) Protein-losing enteropathy after Fontan operation. Congenit Heart Dis 2:288–300
Rychik J (2010) Forty years of the Fontan operation: a failed strategy. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 13:96–100
Schumacher KR, Cools M, Goldstein BH, Ioffe-Dahan V, King K, Gaffney D et al (2011) Oral budesonide treatment for protein-losing enteropathy in Fontan-palliated patients. Pediatr Cardiol 32:966–971
Siffledeen JS, Fedorak RN, Siminoski K, Jen H, Vaudan E, Abraham N et al (2005) Randomized trial of etidronate plus calcium and vitamin D for treatment of low bone mineral density in Crohn’s disease. Clin Gastroenterol Hepatol 3:122–132
Thacker D, Patel A, Dodds K, Goldberg DJ, Semeao E, Rychik J (2010) Use of oral budesonide in the management of protein-losing enteropathy after the Fontan operation. Ann Thorac Surg 89:837–842
Uzun O, Wong JK, Bhole V, Stumper O (2006) Resolution of protein-losing enteropathy and normalization of mesenteric Doppler flow with sildenafil after Fontan. Ann Thorac Surg 82:e39–e40
Weinstein RS (2011) Clinical practice: glucocorticoid-induced bone disease. N Engl J Med 365:62–70
Weinstein RS, Jilka RL, Parfitt AM, Manolagas SC (1998) Inhibition of osteoblastogenesis and promotion of apoptosis of osteoblasts and osteocytes by glucocorticoids: potential mechanisms of their deleterious effects on bone. J Clin Invest 102:274–282
Witzel C, Sreeram N, Coburger S, Schickendantz S, Brockmeier K, Schoenau E (2006) Outcome of muscle and bone development in congenital heart disease. Eur J Pediatr 165:168–174
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goldberg, D.J., Dodds, K., Avitabile, C.M. et al. Children With Protein-Losing Enteropathy After the Fontan Operation Are at Risk for Abnormal Bone Mineral Density. Pediatr Cardiol 33, 1264–1268 (2012). https://doi.org/10.1007/s00246-012-0290-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-012-0290-z