Abstract
Purpose
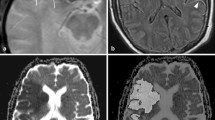
Diffusion-weighted imaging (DWI) lesion expansion after endovascular thrombectomy (EVT) is not well characterized. We used serial diffusion-weighted magnetic resonance imaging (MRI) to measure lesion expansion between 2 and 24 h after EVT.
Methods
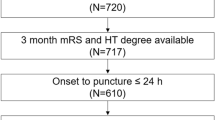
In this single-center observational analysis of patients with acute ischemic stroke due to large vessel occlusion, DWI was performed post-EVT (< 2 h after closure) and 24-h later. DWI lesion expansion was evaluated using multivariate generalized linear mixed modeling with various clinical moderators.
Results
We included 151 patients, of which 133 (88%) had DWI lesion expansion, defined as a positive change in lesion volume between 2 and 24 h. In an unadjusted analysis, median baseline DWI lesion volume immediately post-EVT was 15.0 mL (IQR: 6.6–36.8) and median DWI lesion volume 24 h post-EVT was 20.8 mL (IQR: 9.4–66.6), representing a median change of 6.1 mL (IQR: 1.5–17.7), or a 39% increase. There were no significant associations among univariable models of lesion expansion. Adjusted models of DWI lesion expansion demonstrated that relative lesion expansion (defined as final/initial DWI lesion volume) was consistent across eTICI scores (0–2a, 0.52%; 2b, 0.49%; 2c–3, 0.42%, p = 0.69). For every 1 mL increase in lesion volume, there was 2% odds of an increase in 90-day mRS (OR: 1.021, 95%CI [1.009, 1.034], p < 0.001).
Conclusion
We observed substantial lesion expansion post-EVT whereby relative lesion expansion was consistent across eTICI categories, and greater absolute lesion expansion was associated with worse clinical outcome. Our findings suggest that alternate endpoints for cerebroprotectant trials may be feasible.



Similar content being viewed by others
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
References
Linfante I, Starosciak AK, Walker GR, Dabus G, Castonguay AC, Gupta R, Sun C-HJ, Martin C, Holloway WE, Mueller-Kronast N, English JD, Malisch TW, Marden FA, Bozorgchami H, Xavier A, Rai AT, Froehler MT, Badruddin A, Nguyen TN, Taqi MA, Abraham MG, Janardhan V, Shaltoni H, Novakovic R, Yoo AJ, Abou-Chebl A, Chen PR, Britz GW, Kaushal R, Nanda A, Issa MA, Nogueira RG, Zaidat OO (2016) Predictors of poor outcome despite recanalization: a multiple regression analysis of the NASA registry. J NeuroInterv Surg 8(3):224–229
Ospel J, Rex N, Kandregula S, Goyal M (2023) The vessel has been recanalized: now what? Neurotherapeutics 20(3):679–692
Zhang X, Huang P, Zhang R (2021) Evaluation and prediction of post-stroke cerebral edema based on neuroimaging. Front Neurol 12:763018
Sah RG, d’Esterre CD, Hill MD, Hafeez M, Tariq S, Forkert ND, Demchuk AM, Goyal M, Barber PA (2017) Diffusion-weighted MRI stroke volume following recanalization treatment is threshold-dependent. Clin Neuroradiol 29(1):135–141
Sah RG, d’Esterre CD, Hill MD, Hafeez M, Tariq S, Forkert ND, Frayne R, Demchuk AM, Goyal M, Barber PA (2018) Diffusion-weighted imaging lesion growth occurs despite recanalization in acute ischemic stroke: implications for future treatment trials. Int J Stroke 14(3):257–264
Sarraj A, Hassan AE, Savitz S, Sitton C, Grotta J, Chen P, Cai C, Cutter G, Imam B, Reddy S, Parsha K, Pujara D, Riascos R, Vora N, Abraham M, Kamal H, Haussen DC, Barreto AD, Lansberg M, Gupta R, Albers GW (2019) Outcomes of endovascular thrombectomy vs medical management alone in patients with large ischemic cores: a secondary analysis of the optimizing patient’s Selection for Endovascular Treatment in Acute Ischemic Stroke (SELECT) Study. JAMA Neurol 76(10):1147
Kim Y-C, Lee J-E, Yu I, Song H-N, Baek I-Y, Seong J-K, Jeong H-G, Kim BJ, Nam HS, Chung J-W, Bang OY, Kim G-M, Seo W-K (2019) Evaluation of diffusion lesion volume measurements in acute ischemic stroke using encoder-decoder convolutional network. Stroke 50(6):1444–1451
Goyal M, Menon BK, Zwam WHV, Dippel DWJ, Mitchell PJ, Demchuk AM, Dávalos A, Majoie CBLM, Lugt AVD, Miquel MAD, Donnan GA, Roos YBWEM, Bonafe A, Jahan R, Diener H-C, Berg LAVD, Levy EI, Berkhemer OA, Pereira VM, Rempel J, Millán M, Davis SM, Roy D, Thornton J, Román LS, Ribó M, Beumer D, Stouch B, Brown S, Campbell BCV, Oostenbrugge RJV, Saver JL, Hill MD, Jovin TG (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. The Lancet 387(10029):1723–1731
Hill MD, Goyal M, Menon BK, Nogueira RG, McTaggart RA, Demchuk AM, Poppe AY, Buck BH, Field TS, Dowlatshahi D, van Adel BA, Swartz RH, Shah RA, Sauvageau E, Zerna C, Ospel JM, Joshi M, Almekhlafi MA, Ryckborst KJ, Lowerison MW, Heard K, Garman D, Haussen D, Cutting SM, Coutts SB, Roy D, Rempel JL, Rohr AC, Iancu D, Sahlas DJ, Yu AYX, Devlin TG, Hanel RA, Puetz V, Silver FL, Campbell BCV, Chapot R, Teitelbaum J, Mandzia JL, Kleinig TJ, Turkel-Parrella D, Heck D, Kelly ME, Bharatha A, Bang OY, Jadhav A, Gupta R, Frei DF, Tarpley JW, McDougall CG, Holmin S, Rha JH, Puri AS, Camden MC, Thomalla G, Choe H, Phillips SJ, Schindler JL, Thornton J, Nagel S, Heo JH, Sohn SI, Psychogios MN, Budzik RF, Starkman S, Martin CO, Burns PA, Murphy S, Lopez GA, English J, Tymianski M, Investigators E-N (2020) Efficacy and safety of nerinetide for the treatment of acute ischaemic stroke (ESCAPE-NA1): a multicentre, double-blind, randomised controlled trial. Lancet 395(10227):878–887
Hernández-Pérez M, Werner M, Remollo S, Martín C, Cortés J, Valls A, Ramos A, Dorado L, Serena J, Munuera J, Puig J, N. P. d. l. Ossa, M. Gomis, J. Carbonell, C. Castaño, L. Muñoz-Narbona, E. Palomeras, S. Domenech, A. Massuet, M. Terceño, A. Davalos and M. Millán, (2023) Early and delayed infarct growth in patients undergoing mechanical thrombectomy: a prospective, serial MRI study. Stroke 54(1):217–225
d’Esterre CD, Sah RG, Assis Z, Talai AS, Demchuk AM, Hill MD, Goyal M, Lee TY, Forkert ND, Barber PA (2020) Defining reperfusion post endovascular therapy in ischemic stroke using MR-dynamic contrast enhanced perfusion. Br J Radiol. 93(1116):20190890
Yaghi S, Raz E, Dehkharghani S, Riina H, McTaggart R, Jayaraman M, Prabhakaran S, Liebeskind DS, Khatri P, Grory BM, Al-Mufti F, Lansberg M, Albers G, A. d. Havenon, (2021) Penumbra consumption rates based on time-to-maximum delay and reperfusion status: a post hoc analysis of the DEFUSE 3 Trial. Stroke 52(8):2690–2693
Ospel JM, Hill MD, Menon BK, Demchuk A, McTaggart R, Nogueira R, Poppe A, Haussen D, Qiu W, Mayank A, Almekhlafi M, Zerna C, Joshi M, Jayaraman M, Roy D, Rempel J, Buck B, Tymianski M, Goyal M (2021) Strength of association between infarct volume and clinical outcome depends on the magnitude of infarct size: results from the ESCAPE-NA1 Trial. AJNR Am J Neuroradiol 42(8):1375–1379
Thomalla G, Simonsen CZ, Boutitie F, Andersen G, Berthezene Y, Cheng B, Cheripelli B, Cho TH, Fazekas F, Fiehler J, Ford I, Galinovic I, Gellissen S, Golsari A, Gregori J, Gunther M, Guibernau J, Hausler KG, Hennerici M, Kemmling A, Marstrand J, Modrau B, Neeb L, Perez de la Ossa N, Puig J, Ringleb P, Roy P, Scheel E, Schonewille W, Serena J, Sunaert S, Villringer K, Wouters A, Thijs V, Ebinger M, Endres M, Fiebach JB, Lemmens R, Muir KW, Nighoghossian N, Pedraza S, Gerloff C, Investigators W-U (2018) MRI-guided thrombolysis for stroke with unknown time of onset. N Engl J Med. 379(7):611–622
Marks MP, Lansberg MG, Mlynash M, Olivot JM, Straka M, Kemp S, McTaggart R, Inoue M, Zaharchuk G, Bammer R, Albers GW, Diffusion and I. Perfusion Imaging Evaluation for Understanding Stroke Evolution, (2014) Effect of collateral blood flow on patients undergoing endovascular therapy for acute ischemic stroke. Stroke 45(4):1035–1039
Kleine JF, Wunderlich S, Zimmer C, Kaesmacher J (2017) Time to redefine success? TICI 3 versus TICI 2b recanalization in middle cerebral artery occlusion treated with thrombectomy. Journal of NeuroInterventional Surgery 9(2):117–121
Jang KM, Nam TK, Ko MJ, Choi HH, Kwon JT, Park SW, Byun JS (2020) Thrombolysis in cerebral infarction grade 2C or 3 represents a better outcome than 2B for endovascular thrombectomy in acute ischemic stroke: a network meta-analysis. World Neurosurgery 136:e419–e439
Liang D, Bhatta S, Gerzanich V, Simard JM (2007) Cytotoxic edema: mechanisms of pathological cell swelling. Neurosurg Focus 22(5):E2
von Kummer R, Dzialowski I (2017) Imaging of cerebral ischemic edema and neuronal death. Neuroradiology 59(6):545–553
Nour M, Scalzo F, Liebeskind DS (2013) Ischemia-reperfusion injury in stroke. Interventional neurology 1(3–4):185–199
Liebeskind DS, Bracard S, Guillemin F, Jahan R, Jovin TG, Majoie CB, Mitchell PJ, van der LA, Menon BK, San Roman L, Campbell BC, Muir KW, Hill DM, Dippel DW, Saver JL, Demchuk AM, Davalos A, White P, Brown S, Goyal M (2018) eTICI reperfusion: defining success in endovascular stroke therapy. J Neurointerv. Surg 11(5):433–438
Rivers CS, Wardlaw JM, Armitage PA, Bastin ME, Carpenter TK, Cvoro V, Hand PJ, Dennis MS (2006) Do acute diffusion- and perfusion-weighted MRI lesions identify final infarct volume in ischemic stroke? Stroke 37(1):98–104
Liu CF, Hsu J, Xu X, Ramachandran S, Wang V, Miller MI, Hillis AE, Faria AV (2021) Deep learning-based detection and segmentation of diffusion abnormalities in acute ischemic stroke. Commun Med (Lond) 1:61
Acknowledgements
None
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Rhode Island Hospital Institutional Review Board. This study was performed in line with the principles of the Declaration of Helsinki.
Informed consent
After review by the IRB, the need for informed consent was waived due to the retrospective nature of this study.
Conflict of interest
Nathaniel Rex does not report any conflicts of interest.
Karim Oueidat does not report any conflicts of interest.
Johanna Ospel does not report any conflicts of interest.
Rosalie McDonough does not report any conflicts of interest.
Leon Rinkel does not report any conflicts of interest.
Grayson Baird does not report any conflicts of interest.
Scott Collins does not report any conflicts of interest.
Gaurav Jindal does not report any conflicts of interest.
Matthew Alvin does not report any conflicts of interest.
Jerrold Boxerman does not report any conflicts of interest.
Phil Barber does not report any conflicts of interest.
Mahesh Jayaraman does not report any conflicts of interest.
Wendy Smith does not report any conflicts of interest.
Amanda Amirault-Capuano does not report any conflicts of interest.
Michael Hill reports grants from Canadian Institutes for Health Research, Alberta Innovates, and NoNO, for the conduct of the study; reports personal fees from Merck; reports non-financial support from Hoffmann-La Roche Canada; reports grants from Covidien (Medtronic), Boehringer-Ingleheim, Stryker, and Medtronic, outside the submitted work; reports a patent for systems and methods for assisting in decision-making and triaging for acute stroke patients, issued to US Patent office Number 62/086,077; owns stock in Calgary Scientific; is a director of the Canadian Federation of Neurological Sciences and Circle NeuroVascular; and has received grant support from Alberta Innovates Health Solutions, CIHR, Heart & Stroke Foundation of Canada, and the National Institutes of Neurological Disorders and Stroke. CGM holds stock from NoNO.
Mayank Goyal reports personal fees from Medtronic, Stryker, Microvention, and Mentice, during the conduct of the study; unrestricted research grants to University of Calgary from NoNO, Stryker, and Medtronic; patents for a system of acute stroke diagnosis, with royalties paid to GE Healthcare, and a system of simulation for acute neurointervention, with royalties paid to Mentice; and ownership interest in Circle Neurovascular.
Ryan McTaggart does not report any conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Nathaniel Rex and Karim Oueidat are co-first authors.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rex, N., Oueidat, K., Ospel, J. et al. Modeling diffusion-weighted imaging lesion expansion between 2 and 24 h after endovascular thrombectomy in acute ischemic stroke. Neuroradiology 66, 621–629 (2024). https://doi.org/10.1007/s00234-024-03294-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-024-03294-2