Abstract
Purpose
We compared the predictive accuracy of early-phase brain diffusion tensor imaging (DTI), proton magnetic resonance spectroscopy (1H-MRS), and serum neuron-specific enolase (NSE) against the motor score and epileptic seizures (ES) for poor neurological outcome after out-of-hospital cardiac arrest (OHCA).
Methods
The predictive accuracy of DTI, 1H-MRS, and NSE along with motor score at 72 h and ES for the poor neurological outcome (modified Rankin Scale, mRS, 3 − 6) in 92 comatose OHCA patients at 6 months was assessed by area under the receiver operating characteristic curve (AUROC). Combined models of the variables were included as exploratory.
Results
The predictive accuracy of fractional anisotropy (FA) of DTI (AUROC 0.73, 95% CI 0.62–0.84), total N-acetyl aspartate/total creatine (tNAA/tCr) of 1H-MRS (0.78 (0.68 − 0.88)), or NSE at 72 h (0.85 (0.76 − 0.93)) was not significantly better than motor score at 72 h (0.88 (95% CI 0.80–0.96)). The addition of FA and tNAA/tCr to a combination of NSE, motor score, and ES provided a small but statistically significant improvement in predictive accuracy (AUROC 0.92 (0.85–0.98) vs 0.98 (0.96–1.00), p = 0.037).
Conclusion
None of the variables (FA, tNAA/tCr, ES, NSE at 72 h, and motor score at 72 h) differed significantly in predicting poor outcomes in this patient group. Early-phase quantitative neuroimaging provided a statistically significant improvement for the predictive value when combined with ES and motor score with or without NSE. However, in clinical practice, the additional value is small, and considering the costs and challenges of imaging in this patient group, early-phase DTI/MRS cannot be recommended for routine use.
Trial registration
ClinicalTrials.gov NCT00879892, April 13, 2009.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In-hospital mortality of successfully resuscitated out-of-hospital cardiac arrest (OHCA) patients remains high, ranging from 41 to 86%, despite the implementation of therapeutic hypothermia (also referred to as targeted temperature management) and other treatments [1, 2]. The major cause of morbidity and mortality in survivors of OHCA is hypoxic-ischemic brain damage with survivors at risk for a diverse spectrum of neurological injuries [3].
Based on the current guidelines, neurological prognostication is recommended in patients with a motor score ≤ 3 at 72 h or later after cardiac arrest. Notably, these guidelines allow imaging to be performed before 72 h from ROSC. However, the results of these early imaging studies should only be evaluated later, at the time of clinical determination [4]. A multimodal approach with a combination of clinical assessment, serum biomarkers, electroencephalography, somatosensory-evoked potentials, and neuroimaging is recommended during the early phase at 3–5 days after cardiac arrest. However, a poor outcome cannot be predicted with certainty and the assessment may be confounded by contradictory results from the different assessment modalities [4, 5]. Therefore, there is an unmet need for new biomarkers to improve the accuracy of early-phase prognostication in order to identify patients with a likely poor neurological outcome.
Among conventional methods of neuroimaging, the value of diffusion-weighted imaging (DWI) in neurological prognostication is well-demonstrated; however, DWI has been reported to underestimate the extent of ischemic injury during the first three days after OHCA [6]. While the gray matter has classically been thought to be more sensitive to hypoxic-ischemic brain damage, white matter is also highly vulnerable even in the early stages of ischemia [7]. Diffusion tensor imaging (DTI) is an extension of DWI that allows the evaluation of microstructural integrity of brain white matter using directional assessment of water diffusion, thus potentially being more sensitive than DWI to detect white matter damage in OHCA patients [8].
Proton magnetic resonance spectroscopy (1H-MRS) is another advanced magnetic resonance technique with some evidence of prognostic value in hypoxic-ischemic brain damage in adults after stroke and cardiac arrest as well as in asphyxiated neonates [9,10,11]. 1H-MRS can be used for detecting concentrations of several brain metabolites: N-acetylaspartate (NAA) is almost exclusively cited in neurons and is considered as a marker for neuronal integrity [12]. Creatine (Cr) is produced in the liver and is used as an energy source for ATP synthesis [13]. Often the sum signal of creatine and phosphocreatine (tCr) is used as a reference for other metabolites although its level does not remain constant in all pathologies [14]. Choline (Cho) and phosphocholine (PCho) are mainly situated in the cell membrane and considered as markers for cell membrane density and integrity [10].
However, the value of DTI and 1H-MRS, either alone or in combination with serum neuron-specific enolase (NSE), for predicting poor neurological outcomes at an early phase after OHCA, has yet to be established.
DTI performed between 7 and 28 days after cardiac arrest has shown great promise to accurately predict neurological outcome in this patient group [11]. As defined in the original study protocol, the purpose of this study was to test the hypothesis that DTI and/or MRS could be used at an earlier phase to assess the neurological outcome in this patient group and to further explore whether there is benefit in combining NSE with brain imaging. We assessed the predictive values for a 6-month neurological outcome, dichotomized as good (mRS 0–2) and poor (mRS 3–6), of fractional anisotropy from DTI, several brain metabolites from 1H-MRS each obtained by MRI (magnetic resonance imaging) and NSE performed in comatose survivors within 72 h after OHCA.
Methods
Study design
This study was approved by the ethics committee of the Hospital District of Southwest Finland and the institutional review boards of the Helsinki University Hospital and the Finnish Medicines Agency. All patients’ next of kin or legal representative gave written informed assent within 4 h after hospital arrival. Consent was sought from patients when they regained consciousness. An independent data and safety monitoring committee reviewed data after the enrolment of every 4 patients and after each 6-month interval. The study was conducted according to good clinical practice and the latest revision of the Declaration of Helsinki. The study design and methodology were consistent with the STARD guidelines for reporting diagnostic accuracy studies [15].
Participants
Consecutive comatose survivors of witnessed out-of-hospital cardiac arrest from an initial shockable rhythm admitted to the Turku and Helsinki University hospitals between August 2009 and September 2014 were screened for eligibility. Detailed inclusion and exclusion criteria are listed in Supplementary Information (Online Resource 1).
Randomization and blinding
The patients were allocated in a 1:1 ratio with random block sizes of 4, 6, and 8 to receive either temperature management with 33 °C (TTM) alone for 24 h or inhaled xenon LENOXe, Air Liquide Medical GmbH, DÜsseldorf, Germany in combination with TTM for 24 h. The neurological end-point evaluators as well as the patients were blinded to the treatment.
Procedures
MRI imaging was scheduled to be performed within 16 h of rewarming, i.e., 36–52 h after OHCA. Patients were kept intubated and sedated (with sedation interruptions after completion of rewarming) until brain imaging was performed, regardless of neurological status. A predetermined prognostication protocol (see Supplementary Information Online Resource 1) was used to preclude premature decisions to withdraw life-sustaining therapy. DTI and 1H-MRS results did not inform the outcome of the prognostication. The clinical outcome was evaluated at 6 months after OHCA with a modified ranking scale (mRS) by experienced neurologists.
After rewarming was completed, sedation interruptions were initiated and performed every 6 to 12 h throughout the intensive care stay. A motor score of the Glasgow Coma Scale was assessed during each sedation interruption by a trained intensive care nurse or on-duty intensive care physicians. NSE serum concentration (Immuno-Electro-Chemi-Luminescent assay, Roche Diagnostics GmbH, Mannheim, Germany) was determined at hospital arrival, and at 24 h, 48 h, and 72 h after OHCA. An electroencephalogram was recorded only if it was clinically indicated.
Siemens Magnetom Verio 3 T scanner (Siemens Medical Solutions, Erlangen, Germany) with a 12-element Head Matrix coil was used in both MRI centers. DTI and DWI data were acquired using a diffusion-weighted spin-echo echo planar imaging (SE-EPI) sequence with 20 diffusion encoding directions (see Supplementary Table S1 in Online Resource 1 for details).
FSL software library (version 6.0, Analysis Group, FMRIB, Oxford, United Kingdom) was used for processing the DTI images, following the tract-based spatial statistics (TBSS) processing [16, 17]. This observer-independent and hypothesis-free method has the ability to spatially locate group differences in the DTI data. The mean fractional anisotropy value of white matter was calculated as a mean value of all the voxels in the skeleton (see Supplementary Methods in Online Resource 1 for details).
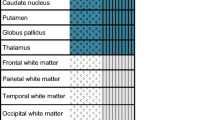
1H-MRS data were acquired from the region of basal ganglia by utilizing Chemical Shift Imaging (CSI) technique (see Supplementary Table S2 in Online Resource 1 for details). Acquired data were analyzed using the LCModel software (version 6.3-0C) [18]. An average of all analyzed voxels, except the ones containing cerebrospinal fluid (CSF), was selected for the final analysis (Fig. 1). The metabolite concentration values were corrected for relaxation effects (Supplementary Methods in Online Resource 1), but absolute concentration values were not feasible to use. Therefore, the amount of tNAA (total N-acetyl aspartate) and total choline (tCho) were expressed as ratios over total creatine (tCr), i.e., tNAA/tCr and tCho/tCr, as it is expected to remain stable. In addition, apart from the tNAA/tCho ratio, the ratio of tNAA and tCho was considered as these individual parameters are related to neuronal density, activity, and integrity [19].
1H-MRS analyzed voxels and typical spectra. A An average of all analyzed voxels in basal ganglia excluding the ones typically including cerebrospinal fluid was used in the analysis. Voxels outside the analysis area are dimmed. B A typical spectrum of a single voxel with tNAA/tCr = 2.41 which is close to the mean of the survivors. C A typical spectrum of a single voxel with tNAA/tCr = 2.19 which is close to the mean of the non-survivors. The signal of total N-acetylaspartate is colored in red, total choline is colored in green, and total creatine is colored in blue
Statistical analysis
The sample size of 110 patients was based on a power analysis of the fractional anisotropy values from brain magnetic resonance imaging. The categorical demographic data and baseline clinical characteristics between groups of mRS 0–2 and mRS 3–6 were compared with chi-square or Fisher’s exact test. Two-sample t test or Mann–Whitney U test was used to test the differences in continuous demographic data and baseline clinical characteristics between the groups mRS 0–2 and mRS 3–6. The normality of continuous variables was evaluated visually using histograms. The mean differences in mean fractional anisotropy, 1H-MRS data, and NSE at 48 and 72 h after OHCA between the groups were tested with two-sample t test. Age-, sex-, treatment-, and site-adjusted mean differences between the groups were compared with analysis of covariance. NSE values were log-transformed for statistical analysis due to positively skewed distribution. Permutation-based voxel-wise statistical analysis with tract-based spatial statistics in conjunction with family-wise error correction was used for multiple comparisons across space to obtain group differences in the white matter tracts [16, 17].
The prognostic values of fractional anisotropy, tNAA/tCr, and NSE 72 h after OHCA and logistic regression-derived combined models were evaluated by calculating the area under the curve of the receiver operating characteristic curve (AUROC) using a nonparametric method. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for each prognostic variable were calculated. Optimal cutoff values were chosen by using the Youden Index (sensitivity + specificity-1). Combined models were described as exploratory.
A 2-sided p value less than 0.05 was considered statistically significant. Statistical analyses were performed with SAS System for Windows, version 9.4 (SAS Institute Inc., Cary, NC) and SPSS Statistics for Macintosh, version 24 (IBM Corp., Armonk, NY).
Results
Patients
Of the 224 patients screened for eligibility, 110 were included. Of these, 97 underwent magnetic resonance imaging in a median (inter-quartile range) time of 53 h (47–64) after OHCA and 93 had 1H-MRS, DTI data available (Fig. 2).
One patient was withdrawn 6 days after the index event by the next of kin, and therefore, 92 out of 93 had applicable mRS data (Fig. 2, Supplementary Table S3 in Online Resource 1). Six months after OHCA, 61 patients had a good (mRS 0–2) and 31 patients had a poor (mRS 3–6) neurological functional outcome. Patient demographics and clinical characteristics are presented in Table 1.
NSE, motor score, and epileptic seizures
NSE at 48 and 72 h after OHCA was significantly higher in patients with poor neurological outcomes than in the patients with good neurological outcomes at 6 months (Table 2, Supplementary Table S4 in Online Resource 1). Nine of the 61 patients with good neurological outcomes and 27 out of 31 patients with poor neurological outcomes had motor score ≤ 3 at 72 h after OHCA (Table 2). Ten patients responded appropriately to commands within 48 h after OHCA; a further 32 patients were responsive to commands between 48 and 72 h, and 25 patients achieved this state later than 72 h. Twenty-five patients never achieved a motor score of 6, all of whom died. The proportion of patients with epileptic seizures (ES) was also significantly higher in the poor outcome group (19/31) than in the good outcome group (6/61).
DTI and 1H-MRS results
Mean fractional anisotropy values of the DTI, and tNAA/tCr and tNAA/tCho ratios of the 1H-MRS were significantly higher in patients with mRS 0–2 than in patients with mRS 3–6 (Table 2). The result of the tract-based spatial statistics analysis is visualized with a statistical parametric map (Fig. 3) [20].
White matter damage leads to a loss of microstructural organization that can be quantified by the loss of directionality in the diffusion of water molecules in the white matter tracts. Fractional anisotropy is a scalar value representing this directionality of water diffusion; lower fractional anisotropy values are indicative of less organized diffusion and are an index of more extensive white matter damage. The visualization presents the results of the voxel-wise tract-based spatial statistics analysis of fractional anisotropy values between patients with good (mRS 0–2) and poor (mRS 3–6) 6-month neurological outcomes. Voxels with significantly (P < 0.05, family-wise error corrected for multiple comparisons) lower fractional anisotropy values in patients with poor neurological outcome were identified and are shown in red in the statistical visualization (i.e., 57.9% of all 123,994 analyzed voxels), whereas the areas in which there was no significant difference in fractional anisotropy values between the groups are shown in green (i.e., 42.1% of all analyzed voxels). According to the Johns Hopkins University white matter tractography atlas [20], the tract-wise distribution of the voxels (percentages in parentheses below) with significantly (P < 0.05; family-wise error corrected for multiple comparisons) lower fractional anisotropy in non-survivors (marked red in the figure) were as follows: cingulum (cingulate gyrus) (41.6%), cingulum (hippocampal region) (59.6%), forceps minor (74.9%) and major (51.6%), superior longitudinal fasciculus (61.6%), inferior longitudinal fasciculus (57.3%), anterior thalamic radiation (66.0%), inferior fronto-occipital fasciculus (62.5%), corticospinal tract (56.4%), uncinate fasciculus (72.4%), and the body of corpus callosum (87.4%)
Receiver operating characteristic analysis of the single measures
The AUROC for predicting poor outcome was 0.73 (95% CI 0.62–0.84) for fractional anisotropy of DTI, 0.78 (0.68–0.88) for tNAA/tCr of 1H-MRS, and 0.85 (0.76–0.93) for NSE at 72 h; fractional anisotropy vs tNAA/tCr, fractional anisotropy vs NSE, and tNAA/tCr vs NSE; p = 0.53, p = 0.13, and p = 0.38, respectively (Fig. 4A, Table 3). Motor score at 72 h provided the best diagnostic predictive value for poor neurological outcome (AUROC 0.88 (95% CI 0.80–0.96), but it did not differ significantly with AUROC values of fractional anisotropy (p = 0.058), tNAA/tCr (p = 0.16), or NSE at 72 h (p = 0.51). The predictive value for ES (AUROC 0.76 (0.66–0.85)) was comparable to neuroimaging (Table 3, Fig. 4A).
Receiver operating characteristic curves of single measures of fractional anisotropy, tNAA/tCr, EEG (epileptic seizures), and NSE at 72 h and motor score ≤ 3 at 72 h (A). The combination of EEG (epileptic seizures), motor score, and NSE at 72 h, and the combination of fractional anisotropy, tNAA/tCr, EEG (epileptic seizures), NSE and motor score ≤ 3 at 72 h (B)
Explorative analysis
The combination of fractional anisotropy, tNAA/tCr, ES, and motor score at 72 h improved the diagnostic performance with or without NSE at 72 h (AUROC 0.98, 95% CI 0.96–1.00) as compared with NSE, motor score, and ES without imaging studies (AUROC 0.92 (0.85–0.98), p = 0.037) (Table 3, Fig. 4B).
Subgroup analysis
A subgroup of 46 patients had a motor score below 6 at 72 h after OHCA. The AUROC for predicting poor outcome in this subgroup was just slightly smaller than in the whole data: 0.72 (95% CI 0.57–0.87) for DTI (fractional anisotropy), 0.76 (0.62–0.90) for 1H-MRS (tNAA/tCr), and 0.82 (0.69–0.95) for NSE at 72 h; fractional anisotropy vs tNAA/tCr, fractional anisotropy vs NSE, and tNAA/tCr vs NSE; p = 0.65, p = 0.33 and p = 0.55, respectively.
Discussion
The main finding of this study was that early-stage quantitative fractional anisotropy of DTI or 1H-MRS did not perform better than NSE or motor score at 72 h or ES for prognosticating poor outcomes at 6 months after OHCA. Combining fractional anisotropy and tNAA/tCr to NSE, motor score and ES improved diagnostic accuracy slightly.
Of the single measures, motor score of ≤ 3 at 72 h provided the best diagnostic predictive value for poor neurological outcomes and NSE at 72 h was the next best. However, the predictive value of the motor score did not reach statistical significance as compared with the results revealed by NSE at 72 h or by the quantitative neuroimaging. In earlier studies, a cutoff value ≤ 2 for motor score has revealed low specificity and high sensitivity between 70 and 80% [21, 22]. Here, we demonstrate similar sensitivity values with higher specificity with the cutoff value of ≤ 3, which is consistent with the latest guidelines [4]; a homogenous cardiac arrest population that only included patients with a shockable primary rhythm can also explain the improvement in the latter attribute.
The current AUROC of 0.85 for NSE is consistent with the values of 0.86 and 0.90 recorded in earlier large studies in TTM-treated patients [23, 24]. However, comparing NSE results among studies may be problematic because cutoff values vary and a consistent threshold limit for 0% false positive ratio has not been recommended [4]. However, the recent guidelines identified a cutoff value of over 60 µg/L at 72 h to suggest poor prognosis when used as part of the multimodal prognostication [4]. In this study, the predictive value of NSE at 72 h with a cutoff value of 21 as identified by the Youden Index did not provide significantly better diagnostic performance as compared to motor score or single parameters obtained by the brain MRI.
Fractional anisotropy is a DTI-derived scalar value that reflects white matter tissue characteristics such as a fiber density, organization coherence, myelination, and axon diameter [25]. Lower fractional anisotropy values in ischemic white matter probably represent a combination of myelin damage, axonal degeneration, and edema, which all contribute to the loss of directional diffusion in white matter tracts [26].
A very recent study demonstrated a prognostic value of decreased mean global white matter fractional anisotropy levels imaged 7 to 28 days after cardiac arrest for long-term neurological outcome with an AUROC of 0.95 in a subset of 150 patients with a persistent unresponsiveness at day 7 [11]. According to earlier evidence, most survivors regain consciousness within a week and usually all of them within 10 days after cardiac arrest [4, 5, 27,28,29]. However, Velly and colleagues revealed that as many as 22% of patients who were without a response to simple commands a week after cardiac arrest may still have a favorable outcome 6 months after cardiac arrest [11]. The current lower prognostic value for fractional anisotropy at the early subacute phase can be partly due to evolving white matter injury over time. This suggests that the predictive value of fractional anisotropy varies depending on the used imaging time window [30]. Conventional DWI MRI seems to perform better than DTI/1H-MRS in the early phase [31, 32]. However, in this study, conventional DWI did not provide any additional value.
NAA is ubiquitous in the central nervous system and is a marker of the integrity of mature neurons; persistent reductions in NAA have been used as a marker of neuronal loss and extent of neurological damage and have prognostic value for outcome in stroke and cardiac arrest [9, 11, 33]. These earlier interpretations were supported by the present study revealing that ratios of tNAA/tCr and tNAA/tCho in the basal ganglia are independent predictors for poor neurological outcomes at 6 months.
In explorative analysis, the addition of early fractional anisotropy of DTI and tNAA/tCr to ES, NSE, and motor score at 72 h provided the best diagnostic performance with an AUROC of 0.98 with or without NSE. This was significantly better than the next best model including ES, motor score at 72 h and NSE. However, the absolute difference in diagnostic value remained relatively small and the predictive value without neuroimaging was already very good with an AUROC of 0.92. Therefore, considering the cost and challenges of MR imaging of critically-ill patients, early-phase DTI/MRS cannot be recommended for routine clinical practice, although it may have a potential role as an additional imaging modality in a multimodal prognostication for selected cases. The clinical applicability of DTI/MRS in the early phase after cardiac arrest needs further investigations in another population including patients with shockable and non-shockable primary rhythms.
There are some limitations in this study. First, our results represent a two-center (single country) cohort of patients in successfully resuscitated cardiac arrest victims in whom a shockable rhythm was the initial rhythm at the time of resuscitation. Therefore, further validation of the results is required in patients with asystole and pulseless electrical activity. Second, earlier studies have demonstrated that pupillary reactivity assessed with pupillometry has a high accuracy to predict poor outcomes after cardiac arrest [34]. Unfortunately, a predictive value of pupillary light reflexes could not be analyzed due to methodological reasons. In this study, the pupillary reactivity was assessed only by standard visual inspection, which led to missing values in 61 patients. Third, metabolite concentration ratios instead of absolute values or inter-subject metabolite concentrations were used. The use of absolute concentration values would have required the use of reference solutions for calibrations and information about coil loading and T2 attenuation, or the use of a water-referencing method; none of these options was available for this study. In routine clinical practice, absolute metabolite values are seldom available, and thus, this approach was not deemed feasible. Fourth, lactate would be an important metabolite in evaluating the extent and stage of the neuronal damage. Unfortunately, the echo time of 135 ms in the CSI sequence leads to an unreliable determination of lactate signal in the 3 T MRI scanner. For a more robust detection of lactate, an echo time of 288 ms should be used, although it would decrease the overall SNR of the spectra [35]. Fifth, due to a possible bias caused by the neuroprotective effect of the xenon on the prognostic value of the current metrics, all statistical analyses were adjusted with the treatment group. Finally, our model was limited by a small number of patients with the study endpoint, and therefore, all variables with predictive value for poor outcomes could not be included.
Conclusions
Neither early-stage quantitative fractional anisotropy measured by DTI nor tNAA/tCr measured by 1H-MRS was better than NSE or motor score at 72 h in predicting poor outcomes in this patient group. While early-phase quantitative neuroimaging provided a statistically significant improvement in the predictive value when combined with NSE, motor score, and ES, the effect was small. Therefore, early-phase DTI/MRS cannot be recommended for routine clinical practice, although it may have a role in multimodal prognostication in specific cases. Current results warrant validation in a larger prospective study in cardiac arrest patients with shockable and non-shockable primary rhythms.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gräsner JT, Lefering R, Koster RW, Masterson S, Böttiger BW, Herlitz J et al (2016) EuReCa ONE Collaborators. EuReCa ONE-27 Nations, ONE Europe, ONE Registry A prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation 105:188–95
Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C et al (2013) TTM trial investigators. targeted temperature management at 33 degrees C versus 36 degrees C after cardiac arrest. N Engl J Med 369(23):2197–206
Dragancea I, Rundgren M, Englund E, Friberg H, Cronberg T (2013) The influence of induced hypothermia and delayed prognostication on the mode of death after cardiac arrest. Resuscitation 84(3):337–342
Nolan JP, Sandroni C, Böttiger BW, Cariou A, Cronberg T, Friberg H et al (2021) European Resuscitation Council and European Society of Intensive Care Medicine Guidelines 2021: post-resuscitation care. Resuscitation 161:220–269
Rossetti AO, Rabinstein AA, Oddo M (2016) Neurological prognostication of outcome in patients in coma after cardiac arrest. Lancet Neurol 15(6):597–609
Wijman CA, Mlynash M, Caulfield AF, Hsia AW, Eyngorn I, Bammer R et al (2009) Prognostic value of brain diffusion-weighted imaging after cardiac arrest. Ann Neurol 65(4):394–402
Matute C, Domercq M, Perez-Samartin A, Ransom BR (2013) Protecting white matter from stroke injury. Stroke 44(4):1204–1211
Luyt CE, Galanaud D, Perlbarg V, Vanhaudenhuyse A, Stevens RD, Gupta R et al (2012) Neuro Imaging for Coma Emergence and Recovery Consortium. Diffusion tensor imaging to predict long-term outcome after cardiac arrest: a bicentric pilot study. Anesthesiology 117(6):1311–21
Federico F, Simone IL, Lucivero V, Giannini P, Laddomada G, Mezzapesa DM et al (1998) Prognostic value of proton magnetic resonance spectroscopy in ischemic stroke. Arch Neurol 55(4):489–494
Cheong JLY, Cady EB, Penrice J, Wyatt JS, Cox IJ, Robertson NJ (2006) Proton MR spectroscopy in neonates with perinatal cerebral hypoxic-ischemic injury: metabolite peak-area ratios, relaxation times, and absolute concentrations. Am J Neuroradiol 27(7):1546–1554
Velly L, Perlbarg V, Boulier T, Adam N, Delphine S, Luyt CE et al (2018) MRI-COMA Investigators. Use of brain diffusion tensor imaging for the prediction of long-term neurological outcomes in patients after cardiac arrest: a multicentre, international, prospective, observational, cohort study. Lancet Neurol 17(4):317–26
Demougeot C, Garnier P, Mossiat C, Bertrand N, Giroud M, Beley A et al (2001) N-Acetylaspartate, a marker of both cellular dysfunction and neuronal loss: its relevance to studies of acute brain injury. J Neurochem 77(2):408–415
Utine GE, Akpınar B, Arslan U, Kiper PÖ, Volkan-Salancı B, Alanay Y et al (2014) Neurochemical evaluation of brain function with 1H magnetic resonance spectroscopy in patients with fragile X syndrome. Am J Med Genet A 164A(1):99–105
Muñoz Maniega S, Cvoro V, Armitage PA, Marshall I, Bastin ME, Wardlaw JM (2008) Choline and creatine are not reliable denominators for calculating metabolite ratios in acute ischemic stroke. Stroke 39(9):2467–2469
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig L et al (2015) STARD Group STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ 351:h5527
Smith SM, Jenkinson M, Johansen-Berg H, Rueckert D, Nichols TE, Mackay CE et al (2006) Tract-based spatial statistics: voxelwise analysis of multi-subject diffusion data. Neuroimage 31(4):1487–1505
Jenkinson M, Beckmann CF, Behrens TE, Woolrich MW, Smith SM (2012) FSL Neuroimage 62(2):782–790
Provencher S (1993) Estimation of metabolite concentrations from localized in-vivo proton Nmr-spectra. Magn Reson Med 30(6):672–679
Tang ZR, Li CS, Zhao H, Gong P, Zhang MY, Su ZY et al (2013) Effects of hypothermia on brain injury assessed by magnetic resonance imaging after cardiopulmonary resuscitation in a porcine model of cardiac arrest. Am J Emerg Med 31(1):86–93
Wakana S, Jiang H, Nagae-Poetscher LM, van Zijl PC, Mori S (2004) Fiber tract-based atlas of human white matter anatomy. Radiology 230(1):77–87
Sandroni C, Cavallaro F, Callaway CW, Sanna T, D’Arrigo S, Kuiper M et al (2013) Predictors of poor neurological outcome in adult comatose survivors of cardiac arrest: a systematic review and meta-analysis. Part 2: patients treated with therapeutic hypothermia. Resuscitation 84:1324–38
Sandroni C, Cavallaro F, Callaway CW, Sanna T, D’Arrigo S, Kuiper M et al (2013) Predictors of poor neurological outcome in adult comatose survivors of cardiac arrest: a systematic review and meta-analysis. Part 1: patients not treated with therapeutic hypothermia. Resuscitation 84:1310–23
Streitberger KJ, Leithner C, Wattenberg M, Tonner PH, Hasslacher J, Joannidis M et al (2017) Neuron-specific enolase predicts poor outcome after cardiac arrest and targeted temperature management: a multicenter study on 1,053 patients. Crit Care Med 45(7):1145–1151
Stammet P, Collignon O, Hassager C, Wise MP, Hovdenes J, Åneman A et al (2015) TTM-Trial Investigators. Neuron-specific enolase as a predictor of death or poor neurological outcome after out-of-hospital cardiac arrest and targeted temperature management at 33 °C and 36 °C. J Am Coll Cardiol 65:2104–14
Beaulieu C (2002) The basis of anisotropic water diffusion in the nervous system - a technical review. NMR Biomed 15(7–8):435–455
Liu Y, D’Arceuil HE, Westmoreland S, He J, Duggan M, Gonzalez RG, Pryor J et al (2007) Serial diffusion tensor MRI after transient and permanent cerebral ischemia in nonhuman primates. Stroke 38(1):138–145
Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Böttiger BW et al (2008) Post-cardiac arrest syndrome epidemiology, pathophysiology, treatment, and prognostication a consensus statement from the international liaison committee on resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa);the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care;the Council on Clinical Cardiology; and the Stroke Council. Circulation 118(23):2452–2483
Grossestreuer AV, Abella BS, Leary M, Perman SM, Fuchs BD, Kolansky DM et al (2013) Time to awakening and neurologic outcome in therapeutic hypothermia-treated cardiac arrest patients. Resuscitation 84(12):1741–1746
Gold B, Puertas L, Davis SP, Metzger A, Yannopoulos D, Oakes DA et al (2014) Awakening after cardiac arrest and post resuscitation hypothermia: are we pulling the plug too early? Resuscitation 85(2):211–214
Zelaya F, Flood N, Chalk JB, Wang D, Doddrell DM, Strugnell W et al (1999) An evaluation of the time dependence of the anisotropy of the water diffusion tensor in acute human ischemia. Magn Reson Imaging 17(3):331–348
Lee BK, Kim WY, Shin J, Oh JS, Wee JH, Cha KC et al (2016) Korean Hypothermia Network Investigators. Prognostic value of gray matter to white matter ratio in hypoxic and non-hypoxic cardiac arrest with non-cardiac etiology. Am J Emerg Med 34:1583–8
Park JS, Lee SW, Kim H, Min JH, Kang JH, Yi KS et al (2015) Efficacy of diffusion-weighted magnetic resonance imaging performed before therapeutic hypothermia in predicting clinical outcome in comatose cardiopulmonary arrest survivors. Resuscitation 88:132–137
Wardlaw J, Marshall I, Wild J, Dennis MS, Cannon J, Lewis SC (1998) Studies of acute ischemic stroke with proton magnetic resonance spectroscopy - relation between time from onset, neurological deficit, metabolite abnormalities in the infarct, blood flow, and clinical outcome. Stroke 29(8):1618–1624
Oddo M, Sandroni C, Citerio G, Miroz J-P, Horn J, Rundgren M et al (2018) Quantitative versus standard pupillary light reflex for early prognostication in comatose cardiac arrest patients: an international prospective multicenter double-blinded study. Intensive Care Med 44:2102–2111
Lange T, Dydak U, Roberts TP, Rowley HA, Bjeljac M, Boesiger P (2006) Pitfalls in lactate measurements at 3T. Am J Neuroradiol 27(4):895–901
Funding
Open Access funding provided by University of Turku (UTU) including Turku University Central Hospital. The study was funded by the Academy of Finland and by the State Research Funding.
Author information
Authors and Affiliations
Consortia
Contributions
TTL had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: TTL, RL, RP, JS, and SV.
Acquisition, analysis, or interpretation of the data: All authors.
Drafting of the manuscript: SV and KK wrote the first draft.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: TV.
Obtained funding: TTL and ROR.
Administrative, technical, or material support: TTL.
Study supervision: TTL and RP.
SV and KK contributed equally.
The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the ethics committee of the Hospital District of Southwest Finland and the institutional review boards of the Helsinki University Hospital and the Finnish Medicines Agency.
Consent to participate
All patients’ next of kin or legal representative gave written informed assent within 4 h after hospital arrival. Consent was sought from patients when they regained consciousness.
Consent for publication
Not applicable.
Conflict of interest
TL reports a grant from the Finnish Foundation for Cardiovascular Research. RL is a paid governmental consultant official for the National Supervisory Authority for Welfare and Health. AS reports grants from the Academy of Finland and Finnish Foundation for Cardiovascular Research during the conduct of the study; consulting fees from the GE Healthcare, Novartis, Abbot, and Astra Zeneca. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Koskensalo, K., Virtanen, S., Saunavaara, J. et al. Comparison of the prognostic value of early-phase proton magnetic resonance spectroscopy and diffusion tensor imaging with serum neuron-specific enolase at 72 h in comatose survivors of out-of-hospital cardiac arrest—a substudy of the XeHypotheca trial. Neuroradiology 65, 349–360 (2023). https://doi.org/10.1007/s00234-022-03063-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-022-03063-z