Abstract
Purpose
Hemodynamics may play an important role in border zone infarct (BZI), but macroscopic and microscopic hemodynamics of BZI still remain unclear. This study aims to investigate arterial flow and tissue perfusion differences between BZI and non-BZI in patients with unilateral middle cerebral artery (MCA) territory infarcts.
Methods
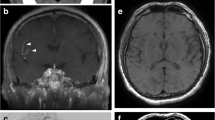
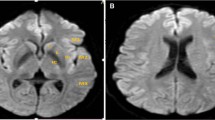
Subacute ischemic stroke patients with unilateral infarcts at MCA territory were included. Imaging protocols included 4D flow, ASL (arterial spin labeling), and routine clinical brain MRI scan. A total of 56 patients (56.1 ± 11.9 years, 39 male) were included and divided as BZI (n = 26) and non-BZI (n = 30). BZI was further subdivided as cortical BZI (CBZI, n = 9), internal BZI (IBZI, n = 11), and mixed BZI (n = 6). Average blood flow (Flowavg), regional average cerebral blood flow (CBFavg) were compared between infarct and contralateral sides to test hemodynamic lateralization. Flow-index and CBF-index (infarct sides/contralateral sides) were compared between groups and subgroups.
Results
Flowavg and CBFavg showed significant lateralization in both BZI and non-BZI as well as CBZI and IBZI. Flow-index (0.51 ± 0.37 vs. 0.87 ± 0.36, p < 0.01) and CBF-index (0.70 ± 0.21 vs. 0.90 ± 0.19, p < 0.01) were significantly different between BZI and non-BZI but were not significantly different between CBZI and IBZI.
Conclusion
In summary, hemodynamic lateralization can occur in subacute stroke patients with BZI and non-BZI and the one that occurs in BZI tends to be more severe in view of arterial flow and tissue perfusion.




Similar content being viewed by others
Availability of data and material
Data supporting the findings of this study are available from the corresponding author on reasonable request.
Code availability
Code supporting the findings of this study are available from the corresponding author on reasonable request.
References
Tatu L, Moulin T, Bogousslavsky J, Duvernoy H (1998) Arterial territories of the human brain: ccerebral hemispheres. Neurology 50:1699–1708. https://doi.org/10.1212/wnl.50.6.1699
Lee DK, Kim JS, Kwon SU, Yoo SH, Kang DW (2005) Lesion patterns and stroke mechanism in atherosclerotic middle cerebral artery disease: early diffusion-weighted imaging study. Stroke 36:2583–2588. https://doi.org/10.1161/01.STR.0000189999.19948.14
Torvik A (1984) The pathogenesis of watershed infarcts in the brain. Stroke 15:221–223. https://doi.org/10.1161/01.STR.15.2.221
Yaghi S, Grory BM, Prabhakaran S, Yeatts SD, Cutting S, Jayaraman M, Sacchetti D, Furie K, Zaidat OO, Liebeskind DS, Khatri P (2019) Infarct pattern, perfusion mismatch thresholds, and recurrent cerebrovascular events in symptomatic intracranial stenosis. J Neuroimaging 29:640–644. https://doi.org/10.1111/jon.12630
Schaafsma JD, Silver FL, Kasner SE, Caplan LR, Rose-Finnell L, Charbel FT, Pandey DK, Amin-Hanjani S, for the VSG (2019) Infarct patterns in patients with atherosclerotic vertebrobasilar disease in relation to hemodynamics. Cerebrovasc Dis Extra 9:123–128. https://doi.org/10.1159/000503091
Del Sette M, Eliasziw M, Streifler JY, Hachinski VC, Fox AJ, Barnett HJ (2000) Internal borderzone infarction: a marker for severe stenosis in patients with symptomatic internal carotid artery disease. For the North American Symptomatic Carotid Endarterectomy (NASCET) Group. Stroke 31:631–636. https://doi.org/10.1161/01.str.31.3.631
Momjian-Mayor I, Baron JC (2005) The pathophysiology of watershed infarction in internal carotid artery disease: review of cerebral perfusion studies. Stroke 36:567–577. https://doi.org/10.1161/01.STR.0000155727.82242.e1
Chaves CJ, Silver B, Schlaug G, Dashe J, Caplan LR, Warach S (2000) Diffusion- and perfusion-weighted MRI patterns in borderzone infarcts. Stroke 31:1090–1096. https://doi.org/10.1161/01.str.31.5.1090
Bisschops RH, Klijn CJ, Kappelle LJ, van Huffelen AC, van der Grond J (2003) Association between impaired carbon dioxide reactivity and ischemic lesions in arterial border zone territories in patients with unilateral internal carotid artery occlusion. Arch Neurol 60:229–233. https://doi.org/10.1001/archneur.60.2.229
Markl M, Frydrychowicz A, Kozerke S, Hope M, Wieben O (2012) 4D flow MRI. J Magn Reson Imaging 36:1015–1036. https://doi.org/10.1002/jmri.23632
Hendrikse J, Petersen ET, van Laar PJ, Golay X (2008) Cerebral border zones between distal end branches of intracranial arteries: MR imaging. Radiology 246:572–580. https://doi.org/10.1148/radiol.2461062100
Song X, Zhao X, Liebeskind DS, Wang L, Xu W, Xu Y, Hou D, Zheng Z, Wu J (2020) Incremental value of plaque enhancement in predicting stroke recurrence in symptomatic intracranial atherosclerosis. Neuroradiology 62:1123–1131. https://doi.org/10.1007/s00234-020-02418-8
van Osch MJ, Teeuwisse WM, van Walderveen MA, Hendrikse J, Kies DA, van Buchem MA (2009) Can arterial spin labeling detect white matter perfusion signal? Magn Reson Med 62:165–173. https://doi.org/10.1002/mrm.22002
Mangla R, Kolar B, Almast J, Ekholm SE (2011) Border zone infarcts: pathophysiologic and imaging characteristics. Radiographics 31:1201–1214. https://doi.org/10.1148/rg.315105014
Yamauchi H, Nishii R, Higashi T, Kagawa S, Fukuyama H (2009) Hemodynamic compromise as a cause of internal border-zone infarction and cortical neuronal damage in atherosclerotic middle cerebral artery disease. Stroke 40:3730–3735. https://doi.org/10.1161/STROKEAHA.109.560011
Li Y, Chen H, He L, Cao X, Wang X, Chen S, Li R, Yuan C (2018) Hemodynamic assessments of venous pulsatile tinnitus using 4D-flow MRI. Neurology 91:e586–e593. https://doi.org/10.1212/WNL.0000000000005948
Amukotuwa S, Straka M, Aksoy D, Fischbein N, Desmond P, Albers G, Bammer R (2019) Cerebral blood flow predicts the infarct core: new insights from contemporaneous diffusion and perfusion imaging. Stroke 50:2783–2789. https://doi.org/10.1161/STROKEAHA.119.026640
Bang OY, Lee PH, Heo KG, Joo US, Yoon SR, Kim SY (2005) Specific DWI lesion patterns predict prognosis after acute ischaemic stroke within the MCA territory. J Neurol Neurosurg Psychiatry 76:1222–1228. https://doi.org/10.1136/jnnp.2004.059998
Mutsaerts HJ, Petr J, Vaclavu L, van Dalen JW, Robertson AD, Caan MW, Masellis M, Nederveen AJ, Richard E, MacIntosh BJ (2017) The spatial coefficient of variation in arterial spin labeling cerebral blood flow images. J Cereb Blood Flow Metab 37:3184–3192. https://doi.org/10.1177/0271678X16683690
Ibaraki M, Nakamura K, Toyoshima H, Takahashi K, Matsubara K, Umetsu A, Pfeuffer J, Kuribayashi H, Kinoshita T (2019) Spatial coefficient of variation in pseudo-continuous arterial spin labeling cerebral blood flow images as a hemodynamic measure for cerebrovascular steno-occlusive disease: a comparative 15O positron emission tomography study. J Cereb Blood Flow Metab 39:173–181. https://doi.org/10.1177/0271678X18781667
ElSadek A, Gaber A, Afifi H, Farag S, Salaheldien N (2019) Microemboli versus hypoperfusion as an etiology of acute ischemic stroke in Egyptian patients with watershed zone infarction. Egypt J Neurol Psychiatr Neurosurg 55:2. https://doi.org/10.1186/s41983-018-0045-8
van Gelderen P, de Zwart JA, Duyn JH (2008) Pittfalls of MRI measurement of white matter perfusion based on arterial spin labeling. Magn Reson Med 59:788–795. https://doi.org/10.1002/mrm.21515
Wong KS, Gao S, Chan YL, Hansberg T, Lam WW, Droste DW, Kay R, Ringelstein EB (2002) Mechanisms of acute cerebral infarctions in patients with middle cerebral artery stenosis: a diffusion-weighted imaging and microemboli monitoring study. Ann Neurol 52:74–81. https://doi.org/10.1002/ana.10250
Mutsaerts H, Petr J, Bokkers RPH, Lazar RM, Marshall RS, Asllani I (2020) Spatial coefficient of variation of arterial spin labeling MRI as a cerebrovascular correlate of carotid occlusive disease. PLoS ONE 15:e0229444. https://doi.org/10.1371/journal.pone.0229444
Funding
This study is supported by the Beijing Municipal Science & Technology Commission (Z171100001017019), Tsinghua University initiative scientific research program (20219990033).
Author information
Authors and Affiliations
Contributions
Wenwen Chen: study design, data acquisition, data analysis, interpretation of the results, article writing; Xiaowei Song: study design, data acquisition, interpretation of the results, article editing; Zhensen Chen: data analysis, interpretation of the results, article editing; Shuo Chen: study design, interpretation of the results, article editing; Mingzhu Fu: data analysis, proofreading; Chenming Wei: interpretation of the results, proofreading; Zhuozhao Zheng: data acquisition, interpretation of the results; Jian Wu: data acquisition, interpretation of the results, article editing; Rui Li: study design, study supervision, interpretation of the results, article editing.
Corresponding authors
Ethics declarations
Ethics approval
The Ethical Review Board of the Beijing Changguang Hospital approved the study, and it was performed in accordance with the guidelines of the Declaration of Helsinki.
Consent to participate
Informed consent from participants was obtained from each patient or their family members.
Consent for publication
Patients signed informed consent regarding publishing their data and photographs.
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, W., Song, X., Chen, S. et al. Blood flow and perfusion lateralization in border zone infarct using 4D flow and arterial spin labeling. Neuroradiology 64, 2145–2152 (2022). https://doi.org/10.1007/s00234-022-02967-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-022-02967-0