Abstract
Purpose
Accurate detection of leptomeningeal metastasis (LM) is critical for risk stratification and treatment of pediatric brain tumors. Poor-quality staging MRI has been associated with decreased survival in this population, but technical factors differentiating good from poor quality screening MRIs remain undefined. To test the hypothesis that key technical factors are associated with accurate MRI diagnosis of leptomeningeal metastasis in children with leptomeningeal seeding brain tumors.
Methods
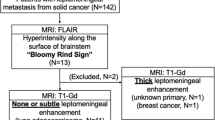
MRIs acquired at outside facilities and repeated in our institution within 35 days for 75 children with leptomeningeal seeding tumors were assessed for slice thickness and gap; use of T2 FLAIR + Contrast, acquisition plane of 3DT1WI + Contrast (brain); axial T1 + Contrast sequence, and use of pre-contrast T1 images (spine). Reported findings were recorded as positive, negative, or equivocal for LM and classified as true positive (TP; unequivocal metastasis), false negative (FN; not reported), false positive (FP; resolved without treatment), or true negative. Wilcoxon signed-rank and Fisher’s exact test were used to assess technical differences between TP and FN MRIs.
Results
Rate of LM detection was greater with smaller interslice gap in brain (P = 0.003) and spine (P = 0.002); use of T2 FLAIR + Contrast (P = 0.005) and sagittal plane for 3DT1WI + Contrast (P = 0.028) in brain; and use of alternatives to axial TSE/FSE in spine (P = 0.048). Slice thickness was not significant. Pre-contrast T1WI did not contribute to LM diagnosis in spine.
Conclusion
Using post-contrast T2 FLAIR and sagittal 3DT1 in brain, small/no interslice gap, and avoiding TSE/FSE axials in spine may facilitate leptomeningeal metastasis detection in children with brain tumors.




Similar content being viewed by others
Code availability (software application or custom code)
Data were reviewed on PACS system no other software (commercial or in-house) was used.
References
Maroldi R, Ambrosi C, Farina D (2005) Metastatic disease of the brain: extra-axial metastases (skull, dura, leptomeningeal) and tumour spread. Eur Radiol 15(3):617–626
Terterov S et al (2010) Evaluation of intracranial cerebrospinal fluid cytology in staging pediatric medulloblastomas, supratentorial primitive neuroectodermal tumors, and ependymomas. J Neurosurg Pediatr 6(2):131–136
Pang J, Banerjee A, Tihan T (2008) The value of tandem CSF/MRI evaluation for predicting disseminated disease in childhood central nervous system neoplasms. J Neurooncol 87(1):97–102
Packer RJ et al (2006) Phase III study of craniospinal radiation therapy followed by adjuvant chemotherapy for newly diagnosed average-risk medulloblastoma. J Clin Oncol 24(25):4202–4208
Fukuoka H et al (2010) Comparison of the added value of contrast-enhanced 3D fluid-attenuated inversion recovery and magnetization-prepared rapid acquisition of gradient echo sequences in relation to conventional postcontrast T1-weighted images for the evaluation of leptomeningeal diseases at 3T. AJNR Am J Neuroradiol 31(5):868–873
Griffiths PD et al (2003) Contrast-enhanced fluid-attenuated inversion recovery imaging for leptomeningeal disease in children. AJNR Am J Neuroradiol 24(4):719–723
Kremer S et al (2006) Accuracy of delayed post-contrast FLAIR MR imaging for the diagnosis of leptomeningeal infectious or tumoral diseases. J Neuroradiol 33(5):285–291
Mathews VP et al (1999) Brain: gadolinium-enhanced fast fluid-attenuated inversion-recovery MR imaging. Radiology 211(1):257–263
Aboian MS et al (2018) Early detection of recurrent medulloblastoma: the critical role of diffusion-weighted imaging. Neurooncol Pract 5(4):234–240
Cho HH, et al. (2016) Free-breathing radial 3D fat-suppressed T1-Weighted gradient-echo sequence for contrast-enhanced pediatric spinal imaging: comparison with T1-weighted turbo spin-echo sequence. AJR Am J Roentgenol 1–6
Harreld JH (2018) Comment on “Response assessment in medulloblastoma and leptomeningeal seeding tumors: recommendations from the Response Assessment in Pediatric Neuro-Oncology Committee.” Neuro Oncol 20(1):143–144
Kralik SF et al (2017) Radiological diagnosis of drop metastases from paediatric brain tumours using combination of 2D and 3D MRI sequences. Clin Radiol 72(10):902.e13-902.e19
Larsen DW, Teitelbaum GP, Norman D (1996) Cerebrospinal fluid flow artifact. A possible pitfall on fast-spin-echo MR imaging of the spine simulating intradural pathology. Clin Imaging 20(2):140–2
Lisanti C et al (2007) Normal MRI appearance and motion-related phenomena of CSF. AJR Am J Roentgenol 188(3):716–725
Shapiro MD (2006) MR imaging of the spine at 3T. Magn Reson Imaging Clin N Am 14(1):97–108
McRobbie DWMEA, Graves MJ, Prince MR (2007) MRI from Picture to Proton (2nd Ed.). Cambridge University Press
Ercan N et al (2004) Diagnostic value of contrast-enhanced fluid-attenuated inversion recovery MR imaging of intracranial metastases. AJNR Am J Neuroradiol 25(5):761–765
Harreld JH et al (2014) Elevated cerebral blood volume contributes to increased FLAIR signal in the cerebral sulci of propofol-sedated children. AJNR Am J Neuroradiol 35(8):1574–1579
Mori N et al (2009) The leptomeningeal “ivy sign” on fluid-attenuated inversion recovery MR imaging in Moyamoya disease: a sign of decreased cerebral vascular reserve? AJNR Am J Neuroradiol 30(5):930–935
Kawashima M et al (2009) Unilateral hemispheric proliferation of ivy sign on fluid-attenuated inversion recovery images in moyamoya disease correlates highly with ipsilateral hemispheric decrease of cerebrovascular reserve. AJNR Am J Neuroradiol 30(9):1709–1716
Elliott JM et al (2011) The pearls and pitfalls of magnetic resonance imaging for the spine. J Orthop Sports Phys Ther 41(11):848–860
McRobbie DW, Moore EA, Graves MJ (2017) MRI from picture to proton. Third edition. Cambridge: University Printing House, Cambridge University Press. xix, 382 pages
Warren KE, et al (2017) Response assessment in medulloblastoma and leptomeningeal seeding tumors: recommendations from the Response Assessment in Pediatric Neuro-Oncology Committee. Neuro Oncol
Ganesan K, Bydder GM (2014) A prospective comparison study of fast T1 weighted fluid attenuation inversion recovery and T1 weighted turbo spin echo sequence at 3 T in degenerative disease of the cervical spine. Br J Radiol 87(1041):20140091
Lavdas E et al (2014) Evaluation of fat saturation and contrast enhancement on T1-weighted FLAIR sequence of the spine at 3.0 T. Clin Imaging 38(4):428–33
Lavdas E et al (2010) Comparison of T1-weighted fast spin-echo and T1-weighted fluid-attenuated inversion recovery images of the lumbar spine at 3.0 Tesla. Acta Radiol 51(3):290–5
Shah KB et al (2011) Comparison of gadolinium-enhanced fat-saturated T1-weighted FLAIR and fast spin-echo MRI of the spine at 3 T for evaluation of extradural lesions. AJR Am J Roentgenol 197(3):697–703
Buch K et al (2018) Balanced Steady-state free precession sequence (CISS/FIESTA/3D driven equilibrium radiofrequency reset pulse) increases the diagnostic yield for spinal drop metastases in children with brain tumors. AJNR Am J Neuroradiol 39(7):1355–1361
Hayes LL et al (2012) Drop metastases to the pediatric spine revealed with diffusion-weighted MR imaging. Pediatr Radiol 42(8):1009–1013
Acknowledgements
The authors wish to thank Bogdan Mitrea for assistance with data collection.
Funding
Supported in part by Grant No. CA21765 from the National Cancer Institute and by the American Lebanese and Syrian Associated Charities.
Author information
Authors and Affiliations
Contributions
Provided in separate document file.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
This study was performed with IRB approval and waiver of consent.
Consent for publication: not applicable
Our paper does not include any individual’s data in any form, so we do not need consent for publication.
Data access statement
The data that support the findings in this study are available upon reasonable request from the corresponding author (AK). The data are not publicly available due to privacy concerns.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was previously presented at the 2018 meeting of The Society for Pediatric Radiology in Nashville, TN.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Harreld, J.H., Khan, A., Angel, J. et al. MRI sequences and interslice gap influence leptomeningeal metastasis detection in children with brain tumors. Neuroradiology 64, 1447–1456 (2022). https://doi.org/10.1007/s00234-022-02928-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-022-02928-7