Abstract
Purpose
Few studies have examined the geometry of endovascular mechanical thrombectomy pathways. Here we examine the tortuosity and angulations of catheter pathways from the aortic arch to the termination of the internal carotid artery (ICA) and its association with thrombectomy performance.
Methods
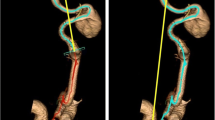
We included 100 consecutive anterior circulation large vessel occlusion thrombectomy patients over 12 months. Computed tomography angiograms (CTA) were used for 3D segmentation of catheter pathway from the aortic arch to ICA termination. Tortuosity index (TI) and angulations of the catheter pathway were measured in a semi-automated fashion. TI and angulation degree were compared between sides and correlated with age and procedural measures.
Results
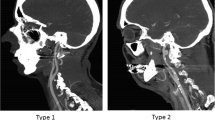
We analyzed 188 catheter pathways in 100 patients. Severe angulation (≤ 30°) was present in 5.8% and 39.4% of common carotid artery (CCA) and extracranial ICA segments, respectively. Five pathways (2.6%) had 360° loop. CCA and extracranial ICA tortuosity had a weak but significant correlation with age (r = 0.17, 0.21, p value = 0.05, 0.02 respectively), time from groin puncture to the site of occlusion (r = 0.29, 0.25, p values = 0.008, 0.026 respectively), and fluoroscopy time (r = 0.022, 0.31, p values = 0.016, 0.001 respectively). There was a significant difference in the pattern of angulation (p value = 0.04) and tortuosity between right and left side in CCA segment (TI = 0.20 ± 0.086 vs. 0.15 ± 0.82, p value < 0.001).
Conclusions
There was a significant difference in CCA angulation between right and left sides. TI of extracranial CCA and ICA correlated with age and influenced time from groin puncture to the occlusion site and total fluoroscopy time.



Similar content being viewed by others
References
Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW et al (2016) Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA 316:1279–1288
Shen XH, Xue HD, Chen Y, Wang M, Mirjalili SA, Zhang ZH et al (2017) A reassessment of cervical surface anatomy via CT scan in an adult population. Clin Anat 30:330–335
Zenteno M, Leeb A, Moscote-Salazar LR (2013) Anatomic variations of the internal carotid artery: implications for the neurologic endovascular therapist. Bol Asoc Med P R 105:70–75
Dumont TM, Mokin M, Wach MM, Drummond PS, Siddiqui AH, Levy EI et al (2014) Understanding risk factors for perioperative ischemic events with carotid stenting: is patient age over 80 years or is unfavorable arch anatomy to blame? J Neurointerv Surg 6:219–224
Werner M, Bausback Y, Braunlich S, Ulrich M, Piorkowski M, Friedenberger J et al (2012) Anatomic variables contributing to a higher periprocedural incidence of stroke and tia in carotid artery stenting: single center experience of 833 consecutive cases. Catheter Cardiovasc Interv 80:321–328
Yamamoto S, Yamagami H, Todo K, Kuramoto Y, Ishikawa T, Imamura H et al (2014) Correlation of middle cerebral artery tortuosity with successful recanalization using the merci retrieval system with or without adjunctive treatments. Neurol Med Chir (Tokyo) 54:113–119
Schwaiger BJ, Gersing AS, Zimmer C, Prothmann S (2015) The curved mca: Influence of vessel anatomy on recanalization results of mechanical thrombectomy after acute ischemic stroke. AJNR Am J Neuroradiol 36:971–976
Pellegrino L, Prencipe G, Vairo F (1998) Dolicho-arteriopathies (kinking, coiling, tortuoosity) of the carotid arteries: study by color doppler ultrasonography. Minerva Cardioangiol 46:69–76
Kim ST, Brinjikji W, Lehman VT, Carr CM, Luetmer PH, Rydberg CH (2018) Association between carotid artery tortuosity and carotid dissection: a case-control study. J Neurosurg Sci 62:413–417
Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL et al (2013) Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke 44:2650–2663
Zaidat OO, Castonguay AC, Linfante I, Gupta R, Martin CO, Holloway WE et al (2018) First pass effect: a new measure for stroke thrombectomy devices. Stroke 49:660–666
Madhwal S, Rajagopal V, Bhatt DL, Bajzer CT, Whitlow P, Kapadia SR (2008) Predictors of difficult carotid stenting as determined by aortic arch angiography. J Invasive Cardiol 20:200–204
Morris SA, Orbach DB, Geva T, Singh MN, Gauvreau K, Lacro RV (2011) Increased vertebral artery tortuosity index is associated with adverse outcomes in children and young adults with connective tissue disorders. Circulation 124:388–396
Dougherty G, Varro J (2000) A quantitative index for the measurement of the tortuosity of blood vessels. Med Eng Phys 22:567–574
Togay-Isikay C, Kim J, Betterman K, Andrews C, Meads D, Tesh P et al (2005) Carotid artery tortuosity, kinking, coiling: stroke risk factor, marker, or curiosity? Acta Neurol Belg 105:68–72
Weibel J, Fields WS (1965) Tortuosity, coiling, and kinking of the internal carotid artery. I. Etiology and radiographic anatomy. Neurology 15:7–18
Kaesmacher J, Gralla J, Mosimann PJ, Zibold F, Heldner MR, Piechowiak E et al (2018) Reasons for reperfusion failures in stent-retriever-based thrombectomy: registry analysis and proposal of a classification system. AJNR Am J Neuroradiol 39:1848–1853
Alawieh A, Vargas J, Fargen KM, Langley EF, Starke RM, De Leacy R et al (2019) Impact of procedure time on outcomes of thrombectomy for stroke. J Am Coll Cardiol 73:879–890
Alawieh A, Pierce AK, Vargas J, Turk AS, Turner RD, Chaudry MI et al (2018) The golden 35 min of stroke intervention with adapt: effect of thrombectomy procedural time in acute ischemic stroke on outcome. J Neurointerv Surg 10:213–220
Spiotta AM, Vargas J, Turner R, Chaudry MI, Battenhouse H, Turk AS (2014) The golden hour of stroke intervention: effect of thrombectomy procedural time in acute ischemic stroke on outcome. J Neurointerv Surg 6:511–516
Kaymaz ZO, Nikoubashman O, Brockmann MA, Wiesmann M, Brockmann C (2017) Influence of carotid tortuosity on internal carotid artery access time in the treatment of acute ischemic stroke. Interv Neuroradiol 23:583–588
Albuquerque FC, Hirsch JA, Chen M, Fiorella D (2020) Robotics in neurointervention: the promise and the reality. J Neurointerv Surg 12:333–334
Funding
This work was supported in part by the NIH grant 1R21NS109575.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Levy—Shareholder/Ownership Interests: NeXtGen Biologics, RAPID Medical, Claret Medical, Cognition Medical, Imperative Care (formerly the Stroke Project), Rebound Therapeutics, StimMed, Three Rivers Medical; National Principal Investigator/Steering Committees: Medtronic (merged with Covidien Neurovascular) SWIFT Prime and SWIFT Direct Trials; Honoraria: Medtronic (training and lectures); Consultant: Claret Medical, GLG Consulting, Guidepoint Global, Imperative Care, Medtronic, Rebound, StimMed; Advisory Board: Stryker (AIS Clinical Advisory Board), NeXtGen Biologics, MEDX, Cognition Medical, Endostream Medical; Site Principal Investigator: CONFIDENCE study (MicroVention), STRATIS Study—Sub I (Medtronic).
Siddiqui—Research Grant: NIH/NINDS 1R01NS091075 as a co-investigator for Virtual Intervention of Intracranial Aneurysms; Financial Interest/Investor/Stock Options/Ownership: Amnis Therapeutics, Apama Medical, Blink TBI Inc., Buffalo Technology Partners Inc., Cardinal Consultants, Cerebrotech Medical Systems, Inc. Cognition Medical, Endostream Medical Ltd., Imperative Care, International Medical Distribution Partners, Neurovascular Diagnostics Inc., Q’Apel Medical Inc, Rebound Therapeutics Corp., Rist Neurovascular Inc., Serenity Medical Inc., Silk Road Medical, StimMed, Synchron, Three Rivers Medical Inc., Viseon Spine Inc; Consultant/Advisory Board: Amnis Therapeutics, Boston Scientific, Canon Medical Systems USA Inc., Cerebrotech Medical Systems Inc., Cerenovus, Corindus Inc., Endostream Medical Ltd., Guidepoint Global Consulting, Imperative Care, Integra LifeSciences Corp., Medtronic, MicroVention, Northwest University–DSMB Chair for HEAT Trial, Penumbra, Q’Apel Medical Inc., Rapid Medical, Rebound Therapeutics Corp., Serenity Medical Inc., Silk Road Medical, StimMed, Stryker, Three Rivers Medical, Inc., VasSol, W.L. Gore & Associates; Principal Investigator/Steering Comment of the Following Trials: Cerenovus NAPA and ARISE II; Medtronic SWIFT PRIME and SWIFT DIRECT; MicroVention FRED & CONFIDENCE; MUSC POSITIVE; and Penumbra 3D Separator, COMPASS, and INVEST.
Borlongan—Funded and received royalties and stock options from Astellas, Asterias, Sanbio, Athersys, KMPHC, and International Stem Cell Corporation; and also received consultant compensation for Chiesi Farmaceutici.
Mokin—Consultant: Canon, Cerebrotech, Imperative care. Investor: Serenity Medical.
None for others
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 18 kb).
Rights and permissions
About this article
Cite this article
Mokin, M., Waqas, M., Chin, F. et al. Semi-automated measurement of vascular tortuosity and its implications for mechanical thrombectomy performance. Neuroradiology 63, 381–389 (2021). https://doi.org/10.1007/s00234-020-02525-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-020-02525-6