Abstract
Purpose
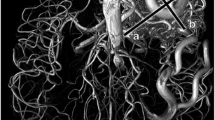
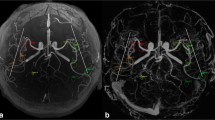
3D multi-echo gradient-recalled echo (ME-GRE) can simultaneously generate time-of-flight magnetic resonance angiography (pTOF) in addition to T2*-based susceptibility-weighted images (SWI). We assessed the clinical performance of pTOF generated from a 3D ME-GRE acquisition compared with conventional TOF-MRA (cTOF).
Methods
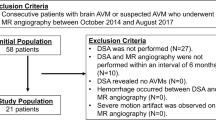
Eighty consecutive children were retrospectively identified who obtained 3D ME-GRE alongside cTOF. Two blinded readers independently assessed pTOF derived from 3D ME-GRE and compared them with cTOF. A 5-point Likert scale was used to rank lesion conspicuity and to assess for diagnostic confidence.
Results
Across 80 pediatric neurovascular pathologies, a similar number of lesions were reported on pTOF and cTOF (43–40%, respectively, p > 0.05). Rating of lesion conspicuity was higher with cTOF (4.5 ± 1.0) as compared with pTOF (4.0 ± 0.7), but this was not significantly different (p = 0.06). Diagnostic confidence was rated higher with cTOF (4.8 ± 0.5) than that of pTOF (3.7 ± 0.6; p < 0.001). Overall, the inter-rater agreement between two readers for lesion count on pTOF was classified as almost perfect (κ = 0.98, 96% CI 0.8–1.0).
Conclusions
In this study, TOF-MRA simultaneously generated in addition to SWI from 3D MR-GRE can serve as a diagnostic adjunct, particularly for proximal vessel disease and when conventional TOF-MRA images are absent.




Similar content being viewed by others
Availability of data
Upon request
References
Nishimura DG (1990) Time-of-flight MR angiography. Magn Reson Med 14:194–201. https://doi.org/10.1002/mrm.1910140206
Graves MJ (1997) Magnetic resonance angiography. Br J Radiol 70:6–28. https://doi.org/10.1259/bjr.70.829.9059290
Du YP, Jin Z (2008) Simultaneous acquisition of MR angiography and venography (MRAV). Magn Reson Med 59:954–958. https://doi.org/10.1002/mrm.21581
Luo J, Jagadeesan BD, Cross AH, Yablonskiy DA (2012) Gradient echo plural contrast imaging--signal model and derived contrasts: T2*, T1, phase, SWI, T1f, FST2*and T2*-SWI. Neuroimage 60:1073–1082. https://doi.org/10.1016/j.neuroimage.2012.01.108
Deistung A, Dittrich E, Sedlacik J, Rauscher A, Reichenbach JR (2009) ToF-SWI: simultaneous time of flight and fully flow compensated susceptibility weighted imaging. J Magn Reson Imaging 29:1478–1484. https://doi.org/10.1002/jmri.21673
Haacke EM, Makki M, Ge Y, Maheshwari M, Sehgal V, Hu J, Selvan M, Wu Z, Latif Z, Xuan Y, Khan O, Garbern J, Grossman RI (2009) Characterizing iron deposition in multiple sclerosis lesions using susceptibility weighted imaging. J Magn Reson Imaging 29:537–544. https://doi.org/10.1002/jmri.21676
Mittal S, Wu Z, Neelavalli J, Haacke EM (2009) Susceptibility-weighted imaging: technical aspects and clinical applications, part 2. AJNR Am J Neuroradiol 30:232–252. https://doi.org/10.3174/ajnr.A1461
Haacke EM, Cheng NYC, House MJ et al (2005) Imaging iron stores in the brain using magnetic resonance imaging. Magn Reson Imaging 23:1–25. https://doi.org/10.1016/j.mri.2004.10.001
Ogg RJ, Langston JW, Haacke EM, Steen RG, Taylor JS (1999) The correlation between phase shifts in gradient-echo MR images and regional brain iron concentration. Magn Reson Imaging 17:1141–1148. https://doi.org/10.1016/s0730-725x(99)00017-x
Petridou N, Wharton SJ, Lotfipour A, Gowland P, Bowtell R (2010) Investigating the effect of blood susceptibility on phase contrast in the human brain. Neuroimage 50:491–498. https://doi.org/10.1016/j.neuroimage.2009.12.052
Sedlacik J, Kutschbach C, Rauscher A, Deistung A, Reichenbach JR (2008) Investigation of the influence of carbon dioxide concentrations on cerebral physiology by susceptibility-weighted magnetic resonance imaging (SWI). Neuroimage 43:36–43. https://doi.org/10.1016/j.neuroimage.2008.07.008
Trofimova A, Kadom N (2019) Added value from abbreviated brain MRI in children with headache. Am J Roentgenol 212:1348–1353. https://doi.org/10.2214/ajr.18.20439
Skare S, Sprenger T, Norbeck O, Rydén H, Blomberg L, Avventi E, Engström M (2017) A 1-minute full brain MR exam using a multicontrast EPI sequence. Magn Reson Med 79:3045–3054. https://doi.org/10.1002/mrm.26974
Ogawa S, Lee T-M, Nayak AS, Glynn P (1990) Oxygenation-sensitive contrast in magnetic resonance image of rodent brain at high magnetic fields. Magn Reson Med 14:68–78. https://doi.org/10.1002/mrm.1910140108
Reichenbach JR, Venkatesan R, Schillinger DJ, Kido DK, Haacke EM (1997) Small vessels in the human brain: MR venography with deoxyhemoglobin as an intrinsic contrast agent. Radiology 204:272–277. https://doi.org/10.1148/radiology.204.1.9205259
Nael K, Khan R, Choudhary G et al (2014) Six-minute magnetic resonance imaging protocol for evaluation of acute ischemic stroke. Stroke 45:1985–1991. https://doi.org/10.1161/strokeaha.114.005305
Miller JH, Walkiewicz T, Towbin RB, Curran JG (2009) Improved delineation of ventricular shunt catheters using fast steady-state gradient recalled-echo sequences in a rapid brain MR imaging protocol in nonsedated pediatric patients. Am J Neuroradiol 31:430–435. https://doi.org/10.3174/ajnr.a1866
Missios S, Quebada PB, Forero JA, Durham SR, Pekala JS, Eskey CJ, Duhaime AC (2008) Quick-brain magnetic resonance imaging for nonhydrocephalus indications. J Neurosurg Pediatr 2:438–444. https://doi.org/10.3171/ped.2008.2.12.438
Tekes A, Senglaub SS, Ahn ES, Huisman TAGM, Jackson EM (2018) Ultrafast brain MRI can be used for indications beyond shunted hydrocephalus in pediatric patients. Am J Neuroradiol. https://doi.org/10.3174/ajnr.a5724
Lindberg DM, Stence NV, Grubenhoff JA, Lewis T, Mirsky DM, Miller AL, O’Neill BR, Grice K, Mourani PM, Runyan DK (2019) Feasibility and accuracy of fast MRI versus CT for traumatic brain injury in young children. Pediatrics 144:e20190419. https://doi.org/10.1542/peds.2019-0419
Ramgopal S, Karim SA, Subramanian S, Furtado AD, Marin JR (2020) Rapid brain MRI protocols reduce head computerized tomography use in the pediatric emergency department. BMC Pediatr 20:14. https://doi.org/10.1186/s12887-020-1919-3
Patel DM, Tubbs RS, Pate G, Johnston JM, Blount JP (2014) Fast-sequence MRI studies for surveillance imaging in pediatric hydrocephalus. J Neurosurg Pediatr 13:440–447. https://doi.org/10.3171/2014.1.peds13447
Iskandar BJ, Sansone JM, Medow J, Rowley HA (2004) The use of quick-brain magnetic resonance imaging in the evaluation of shunt-treated hydrocephalus. J Neurosurg Pediatr 101:147–151. https://doi.org/10.3171/ped.2004.101.2.0147
Niederhauser BD, McDonald RJ, Eckel LJ et al (2013) Retrospective review of rapid pediatric brain MR imaging at an academic institution including practice trends and factors affecting scan times. Am J Neuroradiol 34:1836–1840. https://doi.org/10.3174/ajnr.a3510
Flom L, Fromkin J, Panigrahy A, Tyler-Kabara E, Berger RP (2016) Development of a screening MRI for infants at risk for abusive head trauma. Pediatr Radiol 46:519–526. https://doi.org/10.1007/s00247-015-3500-z
Kralik SF, Yasrebi M, Supakul N, Lin C, Netter LG, Hicks RA, Hibbard RA, Ackerman LL, Harris ML, Ho CY (2017) Diagnostic performance of ultrafast brain MRI for evaluation of abusive head trauma. Am J Neuroradiol 38:807–813. https://doi.org/10.3174/ajnr.a5093
Yue EL, Meckler GD, Fleischman RJ, Selden NR, Bardo DME, Chu O'Connor AK, Vu ET, Fu R, Spiro DM (2015) Test characteristics of quick brain MRI for shunt evaluation in children: an alternative modality to avoid radiation. J Neurosurg Pediatr 15:420–426. https://doi.org/10.3171/2014.9.peds14207
Khalil M, Enzinger C, Langkammer C, Tscherner M, Wallner-Blazek M, Jehna M, Ropele S, Fuchs S, Fazekas F (2009) Quantitative assessment of brain iron by R2* relaxometry in patients with clinically isolated syndrome and relapsing–remitting multiple sclerosis. Mult Scler J 15:1048–1054. https://doi.org/10.1177/1352458509106609
Yan S-Q, Sun J-Z, Yan Y-Q, Wang H, Lou M (2012) Evaluation of brain iron content based on magnetic resonance imaging (MRI): comparison among phase value, R2* and magnitude signal intensity. PLoS One 7:e31748. https://doi.org/10.1371/journal.pone.0031748
Liu Z, Liao H, Yin J, Li Y (2013) Using R2* values to evaluate brain tumours on magnetic resonance imaging: preliminary results. Eur Radiol 24:693–702. https://doi.org/10.1007/s00330-013-3057-x
Salomir R, de Senneville BD, Moonen CTW (2003) A fast calculation method for magnetic field inhomogeneity due to an arbitrary distribution of bulk susceptibility. Concepts Magn Reson 19B:26–34. https://doi.org/10.1002/cmr.b.10083
de Rochefort L, Liu T, Kressler B, Liu J, Spincemaille P, Lebon V, Wu J, Wang Y (2009) Quantitative susceptibility map reconstruction from MR phase data using bayesian regularization: validation and application to brain imaging. Magn Reson Med 63:194–206. https://doi.org/10.1002/mrm.22187
Kressler B, de Rochefort L, Liu T et al (2010) Nonlinear regularization for per voxel estimation of magnetic susceptibility distributions from MRI field maps. IEEE Trans Med Imaging 29:273–281. https://doi.org/10.1109/TMI.2009.2023787
de Rochefort L, Brown R, Prince MR, Wang Y (2008) Quantitative MR susceptibility mapping using piece-wise constant regularized inversion of the magnetic field. Magn Reson Med 60:1003–1009. https://doi.org/10.1002/mrm.21710
Schofield MA, Zhu Y (2003) Fast phase unwrapping algorithm for interferometric applications. Opt Lett 28:1194. https://doi.org/10.1364/ol.28.001194
Liu T, Khalidov I, de Rochefort L, Spincemaille P, Liu J, Tsiouris AJ, Wang Y (2011) A novel background field removal method for MRI using projection onto dipole fields (PDF). NMR Biomed 24:1129–1136. https://doi.org/10.1002/nbm.1670
Schweser F, Deistung A, Lehr BW, Reichenbach JR (2011) Quantitative imaging of intrinsic magnetic tissue properties using MRI signal phase: an approach to in vivo brain iron metabolism? Neuroimage 54:2789–2807. https://doi.org/10.1016/j.neuroimage.2010.10.070
Liu J, Liu T, de Rochefort L, Ledoux J, Khalidov I, Chen W, Tsiouris AJ, Wisnieff C, Spincemaille P, Prince MR, Wang Y (2012) Morphology enabled dipole inversion for quantitative susceptibility mapping using structural consistency between the magnitude image and the susceptibility map. Neuroimage 59:2560–2568. https://doi.org/10.1016/j.neuroimage.2011.08.082
Lenz C, Klarhöfer M, Scheffler K (2011) Feasibility of in vivo myelin water imaging using 3D multigradient-echo pulse sequences. Magn Reson Med 68:523–528. https://doi.org/10.1002/mrm.23241
Fan AP, Evans KC, Stout JN, Rosen BR, Adalsteinsson E (2015) Regional quantification of cerebral venous oxygenation from MRI susceptibility during hypercapnia. Neuroimage 104:146–155. https://doi.org/10.1016/j.neuroimage.2014.09.068
Liu C, Li W (2013) Imaging neural architecture of the brain based on its multipole magnetic response. Neuroimage 67:193–202. https://doi.org/10.1016/j.neuroimage.2012.10.050
Duyn JH, van Gelderen P, Li T-Q, de Zwart JA, Koretsky AP, Fukunaga M (2007) High-field MRI of brain cortical substructure based on signal phase. Proc Natl Acad Sci U S A 104:11796–11801. https://doi.org/10.1073/pnas.0610821104
Marques JP, Maddage R, Mlynarik V, Gruetter R (2009) On the origin of the MR image phase contrast: an in vivo MR microscopy study of the rat brain at 14.1 T. Neuroimage 46:345–352. https://doi.org/10.1016/j.neuroimage.2009.02.023
Rauscher A, Sedlacik J, Deistung A, Mentzel HJ, Reichenbach JR (2006) Susceptibility weighted imaging: data acquisition, image reconstruction and clinical applications. Z Med Phys 16:240–250. https://doi.org/10.1078/0939-3889-00322
Zhong K, Leupold J, von Elverfeldt D, Speck O (2008) The molecular basis for gray and white matter contrast in phase imaging. Neuroimage 40:1561–1566. https://doi.org/10.1016/j.neuroimage.2008.01.061
Langkammer C, Liu T, Khalil M, Enzinger C, Jehna M, Fuchs S, Fazekas F, Wang Y, Ropele S (2013) Quantitative susceptibility mapping in multiple sclerosis. Radiology 267:551–559. https://doi.org/10.1148/radiol.12120707
Langkammer C, Schweser F, Krebs N, Deistung A, Goessler W, Scheurer E, Sommer K, Reishofer G, Yen K, Fazekas F, Ropele S, Reichenbach JR (2012) Quantitative susceptibility mapping (QSM) as a means to measure brain iron? A post mortem validation study. Neuroimage 62:1593–1599. https://doi.org/10.1016/j.neuroimage.2012.05.049
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Preliminary results from this article was presented at the American Society of Neuroradiology 2016 Annual Meeting, May 21-26, Washington, DC. Funding support was provided by ASNR Comparative Effectiveness Grant and NIH grant 1R21HD08380301A1.
Conflict of interest/Competing interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Stanford University Institutional Review Board in the Research Compliance Office (RCO). The study protocol number is 44683.
Informed consent
As the study was entirely retrospective in nature, informed consent for subjects in this study were not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
BAL and YH are co-first authors.
Electronic supplementary material
ESM 1
(DOCX 2.32 MB)
Rights and permissions
About this article
Cite this article
Lanzman, B.A., Huang, Y., Lee, E.H. et al. Simultaneous time of flight-MRA and T2* imaging for cerebrovascular MRI. Neuroradiology 63, 243–251 (2021). https://doi.org/10.1007/s00234-020-02499-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-020-02499-5