Abstract
Purposes
The effects of preoperative statin treatment on acute kidney injury (AKI) remain controversial, and current clinical evidence regarding statin use in the elderly undergoing valve replacement surgery (VRS) is insufficient. The present study aimed to investigate the association between preoperative statin treatment and AKI after VRS in the elderly.
Methods
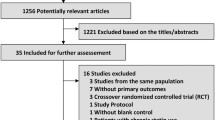
Three thousand seven hundred ninety-one elderly patients (≥ 60 years) undergoing VRS were included in this study and divided into 2 groups, according to the receipt of statin treatment before the operation: statin users (n = 894) and non-users (n = 2897). We determined the associations between statin use, AKI, and other adverse events using a multivariate model and propensity score-matched analysis.
Results
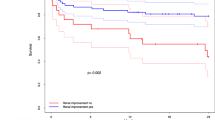
After propensity score-matched analysis, there was no difference between statin users and non-users in regard to postoperative AKI (72.5% vs. 72.4%, p = 0.954), in-hospital death (5.7% vs. 5.1%, p = 0.650) and 1-year mortality (log-rank = 0, p = 0.986). The multivariate analysis showed that statin use was not an independent risk factor for postoperative AKI (OR = 0.97, 95% CI: 0.90–1.17, p = 0.733), in-hospital mortality (OR = 1.12, 95% CI: 0.75–1.68, p = 0.568), or 1-year mortality (HR = 0.95, 95% CI: 0.70–1.28, p = 0.715).
Conclusion
Preoperative statin treatment did not significantly affect the risk of AKI among elderly patients undergoing VRS.


Similar content being viewed by others
Data availability
The data generated or analyzed during this study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
Abbreviations
- AKI: :
-
Acute kidney injury
- VRS: :
-
Valve replacement surgery
- CSA-AKI: :
-
Cardiac surgery-associated acute kidney injury
- SCr: :
-
Serum creatinine
- LVEF: :
-
Left ventricular ejection fraction
- AVR: :
-
Aortic valve replacement
- MVR: :
-
Mitral valve replacement
- TVI: :
-
Tricuspid valve intervention
- CABG: :
-
Coronary artery bypass graft surgery
- CAD: :
-
Coronary artery disease
References
Lau D, Pannu N, James MT, Hemmelgarn BR, Kieser TM, Meyer SR, Klarenbach S (2020) Costs and consequences of acute kidney injury after cardiac surgery: a cohort study. J Thorac Cardiovasc Surg. https://doi.org/10.1016/j.jtcvs.2020.01.101
Gumbert SD, Kork F, Jackson ML, Vanga N, Ghebremichael SJ, Wang CY, Eltzschig HK (2020) Perioperative acute kidney injury. Anesthesiology 132(1):180–204. https://doi.org/10.1097/ALN.0000000000002968
O’Neal JB, Shaw AD, Billings FTt (2016) Acute kidney injury following cardiac surgery: current understanding and future directions. Crit Care 20(1):187. https://doi.org/10.1186/s13054-016-1352-z
Liu LY, Liu Y, Wu MY, Sun YY, Ma FZ (2018) Efficacy of atorvastatin on the prevention of contrast-induced acute kidney injury: a meta-analysis. Drug Des Devel Ther 12:437–444. https://doi.org/10.2147/DDDT.S149106
Joannidis M, Druml W, Forni LG, Groeneveld ABJ, Honore PM, Hoste E, Ostermann M, Oudemans-van Straaten HM, Schetz M (2017) Prevention of acute kidney injury and protection of renal function in the intensive care unit: update 2017: expert opinion of the Working Group on Prevention, AKI section, European Society of Intensive Care Medicine. Intensive Care Med 43(6):730–749. https://doi.org/10.1007/s00134-017-4832-y
Wang J, Gu C, Gao M, Yu W, Yu Y (2015) Preoperative statin therapy and renal outcomes after cardiac surgery: a meta-analysis and meta-regression of 59,771 patients. Can J Cardiol 31(8):1051–1060. https://doi.org/10.1016/j.cjca.2015.02.034
Lewicki M, Ng I, Schneider AG (2015) HMG CoA reductase inhibitors (statins) for preventing acute kidney injury after surgical procedures requiring cardiac bypass. Cochrane Database Syst Rev (3): CD010480. https://doi.org/10.1002/14651858.CD010480.pub2
Zheng Z, Jayaram R, Jiang L, Emberson J, Zhao Y, Li Q, Du J, Guarguagli S, Hill M, Chen Z, Collins R, Casadei B (2016) Perioperative rosuvastatin in cardiac surgery. N Engl J Med 374(18):1744–1753. https://doi.org/10.1056/NEJMoa1507750
Billings FTt, Hendricks PA, Schildcrout JS, Shi Y, Petracek MR, Byrne JG, Brown NJ (2016) High-dose perioperative atorvastatin and acute kidney injury following cardiac surgery: a randomized clinical trial. JAMA 315(9):877–888. https://doi.org/10.1001/jama.2016.0548
Chen J, Li W, Xiang M (2020) Burden of valvular heart disease, 1990–2017: results from the global burden of disease study 2017. J Glob Health 10(2):020404. https://doi.org/10.7189/jogh.10.020404
Yadgir S, Johnson CO, Aboyans V, Adebayo OM, Adedoyin RA, Afarideh M, Alahdab F, Alashi A, Alipour V, Arabloo J, Azari S, Barthelemy CM, Benziger CP, Berman AE, Bijani A, Carrero JJ, Carvalho F, Daryani A, Duraes AR, Esteghamati A, Farid TA, Farzadfar F, Fernandes E, Filip I, Gad MM, Hamidi S, Hay SI, Ilesanmi OS, Naghibi Irvani SS, Jurisson M, Kasaeian A, Kengne AP, Khan AR, Kisa A, Kisa S, Kolte D, Manafi N, Manafi A, Mensah GA, Mirrakhimov EM, Mohammad Y, Mokdad AH, Negoi RI, Thi Nguyen HL, Nguyen TH, Nixon MR, Otto CM, Patel S, Pilgrim T, Radfar A, Rawaf DL, Rawaf S, Rawasia WF, Rezapour A, Roever L, Saad AM, Saadatagah S, Senthilkumaran S, Sliwa K, Tesfay BE, Tran BX, Ullah I, Vaduganathan M, Vasankari TJ, Wolfe CDA, Yonemoto N, Roth GA, Global burden of disease study nonrheumatic valve disease C (2020) global, regional, and national burden of calcific aortic valve and degenerative mitral valve diseases, 1990–2017. Circulation 141(21):1670–1680. https://doi.org/10.1161/CIRCULATIONAHA.119.043391
Lancellotti P, Tribouilloy C, Hagendorff A, Popescu BA, Edvardsen T, Pierard LA, Badano L, Zamorano JL, Scientific Document Committee of the European Association of Cardiovascular I (2013) Recommendations for the echocardiographic assessment of native valvular regurgitation: an executive summary from the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 14(7):611–644. https://doi.org/10.1093/ehjci/jet105
Ostermann M, Zarbock A, Goldstein S, Kashani K, Macedo E, Murugan R, Bell M, Forni L, Guzzi L, Joannidis M, Kane-Gill SL, Legrand M, Mehta R, Murray PT, Pickkers P, Plebani M, Prowle J, Ricci Z, Rimmele T, Rosner M, Shaw AD, Kellum JA, Ronco C (2020) Recommendations on acute kidney injury biomarkers from the acute disease quality initiative consensus conference: a consensus statement. JAMA Netw Open 3(10):e2019209. https://doi.org/10.1001/jamanetworkopen.2020.19209
Ge S, Nie S, Liu Z, Chen C, Zha Y, Qian J, Liu B, Teng S, Xu A, Bin W, Xu X, Xu G (2016) Epidemiology and outcomes of acute kidney injury in elderly Chinese patients: a subgroup analysis from the EACH study. BMC Nephrol 17(1):136. https://doi.org/10.1186/s12882-016-0351-2
Pickering JW, James MT, Palmer SC (2015) Acute kidney injury and prognosis after cardiopulmonary bypass: a meta-analysis of cohort studies. Am J Kidney Dis 65(2):283–293. https://doi.org/10.1053/j.ajkd.2014.09.008
Hu J, Spina S, Zadek F, Kamenshchikov NO, Bittner EA, Pedemonte J, Berra L (2019) Effect of nitric oxide on postoperative acute kidney injury in patients who underwent cardiopulmonary bypass: a systematic review and meta-analysis with trial sequential analysis. Ann Intensive Care 9(1):129. https://doi.org/10.1186/s13613-019-0605-9
Meersch M, Schmidt C, Hoffmeier A, Van Aken H, Wempe C, Gerss J, Zarbock A (2017) Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high risk patients identified by biomarkers: the PrevAKI randomized controlled trial. Intensive Care Med 43(11):1551–1561. https://doi.org/10.1007/s00134-016-4670-3
Wang Y, Bellomo R (2017) Cardiac surgery-associated acute kidney injury: risk factors, pathophysiology and treatment. Nat Rev Nephrol 13(11):697–711. https://doi.org/10.1038/nrneph.2017.119
Xu J, Xu X, Shen B, Zhuang Y, Liu L, Wang Y, Fang Y, Luo Z, Teng J, Wang C, Ronco C, Yu J, Ding X (2019) Evaluation of five different renal recovery definitions for estimation of long-term outcomes of cardiac surgery associated acute kidney injury. BMC Nephrol 20(1):427. https://doi.org/10.1186/s12882-019-1613-6
Ivert T, Holzmann MJ, Sartipy U (2014) Survival in patients with acute kidney injury requiring dialysis after coronary artery bypass grafting. Eur J Cardiothorac Surg 45(2):312–317. https://doi.org/10.1093/ejcts/ezt247
Li M, Zou H, Xu G (2016) The prevention of statins against AKI and mortality following cardiac surgery: a meta-analysis. Int J Cardiol 222:260–266. https://doi.org/10.1016/j.ijcard.2016.07.173
Wang Y, Zhu S, Du R, Zhou J, Chen Y, Zhang Q (2018) Statin initiation and renal outcomes following isolated coronary artery bypass grafting: a meta-analysis. J Cardiovasc Surg (Torino) 59(2):282–290. https://doi.org/10.23736/S0021-9509.17.10074-1
Bjorklund E, Nielsen SJ, Hansson EC, Karlsson M, Wallinder A, Martinsson A, Tygesen H, Romlin BS, Malm CJ, Pivodic A, Jeppsson A (2020) Secondary prevention medications after coronary artery bypass grafting and long-term survival: a population-based longitudinal study from the SWEDEHEART registry. Eur Heart J 41(17):1653–1661. https://doi.org/10.1093/eurheartj/ehz714
Sirtori CR (2014) The pharmacology of statins. Pharmacol Res 88:3–11. https://doi.org/10.1016/j.phrs.2014.03.002
Werida R, Khairat I, Khedr NF (2021) Effect of atorvastatin versus rosuvastatin on inflammatory biomarkers and LV function in type 2 diabetic patients with dyslipidemia. Biomed Pharmacother 135:111179. https://doi.org/10.1016/j.biopha.2020.111179
Liu WT, Lin C, Tsai MC, Cheng CC, Chen SJ, Liou JT, Lin WS, Cheng SM, Lin CS, Tsao TP (2020) Effects of pitavastatin, atorvastatin, and rosuvastatin on the risk of new-onset diabetes mellitus: a single-center cohort study. Biomedicines 8 (11). https://doi.org/10.3390/biomedicines8110499
Mithani S, Kuskowski M, Slinin Y, Ishani A, McFalls E, Adabag S (2011) Dose-dependent effect of statins on the incidence of acute kidney injury after cardiac surgery. Ann Thorac Surg 91(2):520–525. https://doi.org/10.1016/j.athoracsur.2010.10.061
Acknowledgements
Not applicable.
Funding
This study was supported by grants from the National Natural Science Foundation of China [grant no. 82002014], the Science and Technology Projects of Guangzhou [grant no. 201903010097], the National Clinical Key Specialty Construction Project of China [grant no. 2012–649 and 2013–544], and Natural Science Foundation of Guangdong Province (grant no. 2021A1515010107). The funders had no role in the study design, data collection and analysis, decision to publish, or the preparation of the manuscript. The work was not funded by any industry sponsors.
Author information
Authors and Affiliations
Contributions
DQY, JYC, and SHW were involved in the conception and design of the study. BQF, XBW, ZDZS, YWL, ZHK, and TT contributed to data collection and/or analysis. BQF, XBW, and ZDZS were involved in the construction of the manuscript, which was revised critically and approved by all the authors for publication.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Research Ethics Committee of Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences with a waiver of written informed consent (No. GDREC2018525H).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fu, Bq., Wei, Xb., Su, Z. et al. The effect of preoperative statin treatment on acute kidney injury in elderly patients undergoing valve replacement surgery. Eur J Clin Pharmacol 78, 505–512 (2022). https://doi.org/10.1007/s00228-021-03252-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-021-03252-4