Abstract
Purpose
This systematic review aimed to determine whether olanzapine is more likely than other second-generation antipsychotics (SGAs) to induce insulin resistance in patients with schizophrenia in China.
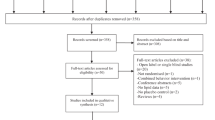
Methods
We reviewed all randomized controlled trials on insulin resistance and metabolic abnormalities caused by SGAs in the PubMed, China National Knowledge Infrastructure (CNKI), VIP, and Wanfang databases. Retrieved articles were published on or before December 2018. Meta-analysis was performed to determine the effect size of the treatment on the insulin resistance index (IRI), fasting blood glucose (FBG), and fasting insulin (FINS).
Results
Forty studies (3725 participants in total) were included. All studies contained data suitable for comparing aripiprazole vs. olanzapine, ziprasidone vs. olanzapine, and risperidone vs. olanzapine. Patients treated with olanzapine had higher IRI, FBG, and FINS levels than did patients treated with aripiprazole, ziprasidone, or risperidone, with significant differences (aripiprazole vs. olanzapine: FBG: standardized mean difference [SMD] = 0.72, 95% confidence interval [95%CI] − 0.82, − 0.61; FINS: SMD = − 0.8, 95%CI − 1.00, − 0.61; IRI: SMD = − 0.80, 95%CI − 0.99, − 0.61; ziprasidone vs. olanzapine: FBG: SMD = − 1.19, 95%CI − 1.30, − 1.08; FINS: SMD = − 0.66, 95%CI − 0.85, − 0.47; IRI: SMD = − 0.71, 95%CI − 0.88, − 0.55; risperidone vs. olanzapine: FBG: SMD = − 0.17, 95%CI − 0.34, − 0.00).
Conclusions
Existing data suggest that olanzapine is associated with a significantly greater risk of IRI, FBG, and FINS, while other agents are associated with relatively lower risks. Thus, olanzapine is more likely to induce insulin resistance than are other SGAs in schizophrenic patients in China.









Similar content being viewed by others
References
Kılıçoğlu Öİ, Salduz A, Birişik F, Bilgili F, Polat G, Kaya İ, Süleyman F, Coşkun M (2018) High rates of psychiatric disorders and below normal mental capacity associated with spastic peroneal flatfoot: a new relationship. J Foot Ankle Surg 57:501
Thaker GK Jr, C.W. (2001) Advances in schizophrenia. Nat Med 7:667–671
Kenji T, Nagahide T, Shinichi S, Nobuhisa M, Kunihiro I, Keizo Y, Hiroyuki K, Tetsuya I, Norio O (2010) Relationship of psychopathological symptoms and cognitive function to subjective quality of life in patients with chronic schizophrenia. Psychiatry Clin Neurosci 64:62–69
Shin O, Seiya M, Tomomi T, Rei K, Kazuaki O, Nobumi M, Yasuyuki F, Jun A, Sachiko T, Yukie I (2011) Effects of discontinuation of long-term biperiden use on cognitive function and quality of life in schizophrenia. Prog Neuro-Psychopharmacol Biol Psychiatry 35:78–83
Attard A, Taylor DM (2012) Comparative effectiveness of atypical antipsychotics in schizophrenia. CNS Drugs 26:491–508
del Campo A, Bustos C, Mascayano C, Acuña C (2018) Metabolic syndrome and antipsychotics: the role of mitochondrial fission/fusion imbalance. Front Endocrinol 9:144
Mathews M, Muzina DJ (2007) Atypical antipsychotics: new drugs, new challenges. Cleve Clin J Med 74:597–606
Stein-Reisner O, Preisman O, Alfici S, Melamed Y, Bleich A (2004) A long-acting second generation anti-psychotic—experience in Israel. Harefuah. 143:408–409
Gonçalves P, Araújo JR, Martel F (2015) Antipsychotics-induced metabolic alterations: focus on adipose tissue and molecular mechanisms. Eur Neuropsychopharmacol 25:1–16
Kobyliak N, Falalyeyeva T, Mykhalchyshyn G, Kyriienko D (2018) Effect of alive probiotic on insulin resistance in type 2 diabetes patients: randomized clinical trial. Diabetes & Metabolic Syndrome: Clinical Research & Reviews S1871402118301061
Reaven GM (1993) Role of insulin resistance in human disease (syndrome X): an expanded definition. Annu Rev Med 44:121–131
Hou P-H, Chen C-P, Geng-Ruei C, Lin Y-L (2018) Long-term administration of olanzapine induces adiposity and increases hepatic fatty acid desaturation protein in female C57BL/6J mice. Iranian J Basic Med Sci 21:495
Correll CU, Todd L, Malhotra AK (2011) Antipsychotic drugs and obesity. Trends Mol Med 17:97–107
Newcomer JW (2005) Second-generation (atypical) antipsychotics and metabolic effects. CNS Drugs 19:1–93
Haupt DW, Newcomer JW (2001) Hyperglycemia and antipsychotic medications. J Clin Psychiatry 62(Suppl. 27):15–26
Leucht S, Cipriani A, Spineli L, Mavridis D, Örey D, Richter F, Samara M, Barbui C, Engel RR, Geddes JR (2013) Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet. 382:951–962
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Revista Española de Nutrición Humana y Dietética 18(3):e123
Abdulghani MA, Defronzo RA (2010) Pathogenesis of insulin resistance in skeletal muscle. Journal of Biomedicine & Biotechnology 2010(1):476279
Zheng Q, Meng G, Li Y, Deng L (2010) Influences of aripiprazole and olanzapine on glycolipid metabolism of schizophrenia patients. J Clin Psychosom Dis 16:102–103
Li X, Xing B, Zhang Y, Wu H (2011) Comparison of endoctine and metabolic effects of airpiprazole and olanzapine on the treatment of schizophrenia. Clin Educ Gen Pract 4:384–386
Chen Y, Wen W, Zheng Y, Zhang C, Zou G, Li Y, Yang F (2012) Comparative study on efficacy, weight, blood sugar and blood lipid between ziprasidone and olanzapine in treatment of first-episode female patients with schizophrenia. Pharm Today 07:410–412
Liu S, Zou Z (2013) A comparative study of domestic aripiprazole and olanzapine in the treatment of schizophrenia. Chongqing Medicine 2013(29):3548–3550
Xiao M, Hui D, Yang M, Liu J (2013) A control study of metabolic syndrome induced by atypical antipsychotics in schizophrenia. J Clin Psychosom Dis 19:11–13
Jian-kang XU, Xu L, Lu-bin Z, Hong-xia LV, Chang-hong W (2013) Effects of aripiprazole versus olanzapine on glucose and lipid metabolism in first-episode of schizophrenics. Henan Med Res 22:183–187
Liu C (2014) A comparative study of the efficacy of aripiprazole and olanzapine in the treatment of patients with schizophrenia and the effects of glucose and lipid metabolism. The Chinese and foreign health abstract 15:13–14
Lu X, Liu S, Tian B (2014) A comparative study of the effects of olanzapine and aripiprazole on glucose and lipid metabolism in first-episode schizophrenia. J Psychiatr 27:369–370
Chen W (2015) Effect of ziprasidone and olanzapine on clinical efficacy and glucose and lipid metabolism in first-episode schizophrenia. J Math Med 1:30–31
Gao C (2015) Effect on aripiprazole and olanzapine in the treatment of schizophrenia and influence on glucolipid metabolism. Chin J Pract Nerv Dis 9:27–28
Huang S, Chen X, Wei M (2015) Comparison of curative effects of two therapeutic drugs on elderly patients with schizophrenia and effects of glycolipid metabolism. Psychologist 21:36–37
Liu Q, Zhao J, Shen L (2015) Effect of aripiprazole and olanzapine on clinical efficacy and glucose and lipid metabolism in patients with first-episode schizophrenia. Chin J Trauma Disability Med 23:90–91
Zhao J, Li W, Gu X, Ai X, Hua T, Lv L (2015) Effect of low-dose aripiprazole on metabolism and quality of life in patients with schizophrenia taking olanzapine. Chin J New Drugs Clin Remed 12:929–934
Shucun B (2016) Effects of different drugs on treatment of elderly schizophrenia and on glucolipid metabolism. Med J Nat Defend Forces Southw China 26:975–977
Wang S (2016) Comparison of the effects of olanzapine and aripiprazole in the treatment of schizophrenia. Chin J Rural Med Pharm 23:19–20
Hui Y, Gangqiao Q, Yaoyu Y (2017) Effects of aripiprazole and olanzapine on body weight and lipid metabolism in schizophrenia patients. Chin J Prim Med Pharm 24:600–603
Sun R, Xue F, Peng Z, Tan Q (2012) Effects on body mass and metabolism of ziprasidone versus olanzapine in the treatment of schizophrenia. J Psychiatry 01:8–10
Wu J (2017) Effects of aripiprazole and olanzapine on body mass and glycolipid metabolism in patients with schizophrenia. World Clin Med 11:93
Chen Q, Liu X, Chen Y (2008) Research on efficacy and safety of olanzapine and ziprasidonein the treatment of research on efficacy and safety of olanzapine and ziprasidonein the treatment of schizophrenia. Chin J Hosp Pharm 28(21):1856–1858
Jia J, Zhang Y (2013) Comparison of effects of different drugs on glucose and lipid metabolism in newly diagnosed patients with schizophrenia. Chin J Clin 24:11867–11868
Shao P, Ou J, Wu R, Fang M, Chen H, Xu Y, Zhao J (2013) Effects of ziprasidone and olanzapine on glucose and lipid metabolism in first-episode schizophrenia. J Cent South Univ 38:365–369
Chen X (2014) Clinical efficacy of ziprasidone and olanzapine in the treatment of first-episode schizophrenia and study on the safety of glycolipid metabolism. For All Health 10:510
Lv S, Luo C (2014) Efficacy of ziprasidone and olanzapine in the treatment of elderly patients with schizophrenia and its effect on glucose and lipid metabolism. Chin J Gerontol 34:908–909
Hao J, Chen B, Qin T, Wang L, Wen J (2015) Clinical observation of ziprasidone combined with olanzapine in the treatment of refractory schizophrenia in elderly patients. China Pharm 26:4652–4654
Xiao J (2015) Clinical analysis on ziprasidone and olanzapine in the treatment of early schizophrenia. China Modern Med 22(30):80–82
Xuezhi Y, Bing LU, Jianqing M, Wan W (2015) Effect of ziprasidone and olanzapine in treatment of newly diagnosed mental patients and its effects on metabolism of glucose and lipid. Modern Chin Doctor 11:16–18
Yuan M, Wu N, Wang J, Yuan B (2015) Therapeutic effect of ziprasidone and olanzapine in elderly patients with schizophrenia and its effect on blood glucose and blood lipid levels. J Int Psychiatry 02:29–32
Huang Y, Lou Y (2016) Efficacy of ziprasidone and olanzapine in the treatment of elderly patients with organic brain disorders and its effects on glucose and lipid metabolism. China Pract Med 11(27):170–171
Zhou Y (2016) Effect of ziprasidone and olanzapine on glucose and lipid metabolism in patients with first-episode schizophrenia. World Latest Medicine (88)
Zhao X (2017) Effects of ziprasidone and olanzapine on glucolipid metabolism of first-episode schizophrenia patients. J Clin Psychosom Dis 23(14–15):19
Li M, Xie C (2008) Changes of blood glucose and lipid levels in adolescents with first-episode schizophrenia treated with olanzapine and riperidone. J Psychiatry 21:107–109
Zhao M, Xie F (2011) Efficacy of olanzapine and risperidone in the treatment of schizophrenia in elderly women and its effect on glucose and lipid metabolism. Chin Rural Health Serv Adm 31:1307–1309
Yu J, Hao Z, Xu P, Wang Z, Lin X, Sun J, Li H (2014) A control of schizophrenia’s metabolic syndrome caused by olanzapine and risperidone. J Clin Psychosom Dis 113:1–4
Xu X (2015) Efficacy of olanzapine and risperidone in the treatment of schizophrenia in elderly women and its effect on glucose and lipid metabolism. J Qiqihar Med College 36:2557–2558
Liu W (2017) Correlation between metabolic disorder related index and serum adiponectin in schizophrenics caused by olanzapine. J Clin Psychosom Dis 23:21–27
Wang L, Lv H, Xu J, Ma W (2017) Effects of different atypical antipsychotics on the efficacy, body mass and liposaccharide metabolism in patients with organic mental disorders. J Int Psychiatry 44(1)
Higgins, JPT (2008) Cochrane Handbook for Systematic Reviews of Interventions. Cochrane handbook for systematic reviews of interventions
Fukushima M, Taniguchi A, Sakai M, Doi K, Nagasaka S, Tanaka H, Tokuyama K, Nakai Y (1999) Homeostasis model assessment as a clinical index of insulin resistance. Comparison with the minimal model analysis. Diabetes Care 22(11):1911–1912
Jozef Peuskens MDHM (2001) The clinical value of risperidone and olanzapine: a meta-analysis of efficacy and safety. Int J Psychiat Clin 5:179–187
Bartoli F, Crocamo C, Clerici M, Carrà G (2015) Second-generation antipsychotics and adiponectin levels in schizophrenia: a comparative meta-analysis. Eur Neuropsychopharmacol 25:1767–1774
Patricio LJ, Diego GA, Jose LL, Cristina LL, Javier MO, Andrea GR, Stefany TC (2014) The role of leptin/adiponectin ratio in metabolic syndrome and diabetes. Horm Mol Biol Clin Invest 18:37–45
Author’s contributors
LY. Yu and SL. Wu participated in the design of the study, collection and analysis of data, drawing conclusions, and writing of the manuscript. They are the first author, and they contributed equally to this work. YH. Deng and LX. Yu participated in drawing conclusions and reviewing the manuscript. They are the co-author. J. Lei managed the literature searches and extracted data. She is the co-author. WY. Li participated in the design of the study, participated in drawing conclusions, and reviewing the manuscript. He is the corresponding author. All authors contributed to and have approved the final manuscript.
Funding
The work was financially supported by the National Natural Science Foundation of China under Grant No. 81573509.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Yu, L., Wu, S., Deng, Y. et al. Insulin resistance induced by olanzapine and other second-generation antipsychotics in Chinese patients with schizophrenia: a comparative review and meta-analysis. Eur J Clin Pharmacol 75, 1621–1629 (2019). https://doi.org/10.1007/s00228-019-02739-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-019-02739-5