Abstract
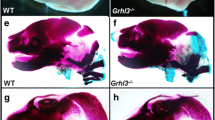
Crouzon syndrome is a debilitating congenital disorder involving abnormal craniofacial skeletal development caused by mutations in fibroblast growth factor receptor-2 (FGFR2). Phenotypic expression in humans exhibits an autosomal dominant pattern that commonly involves premature fusion of the coronal suture (craniosynostosis) and severe midface hypoplasia. To further investigate the biologic mechanisms by which the Crouzon syndrome–associated FGFR2C342Y mutation leads to abnormal craniofacial skeletal development, we created congenic BALB/c FGFR2C342Y/+ mice. Here, we show that BALB/c FGFR2C342Y/+ mice have a consistent craniofacial phenotype including partial fusion of the coronal and lambdoid sutures, intersphenoidal synchondrosis, and multiple facial bones, with minimal fusion of other craniofacial sutures. This phenotype is similar to the classic and less severe form of Crouzon syndrome that involves significant midface hypoplasia with limited craniosynostosis. Linear and morphometric analyses demonstrate that FGFR2C342Y/+ mice on the BALB/c genetic background differ significantly in form and shape from their wild-type littermates and that in this genetic background the FGFR2C342Y mutation preferentially affects some craniofacial bones and sutures over others. Analysis of cranial bone cells indicates that the FGFR2C342Y mutation promotes aberrant osteoblast differentiation and increased apoptosis that is more severe in frontal than parietal bone cells. Additionally, FGFR2C342Y/+ frontal, but not parietal, bones exhibit significantly diminished bone volume and density compared to wild-type mice. These results confirm that FGFR2-associated craniosynostosis occurs in association with diminished cranial bone tissue and may provide a potential biologic explanation for the clinical finding of phenotype consistency that exists between many Crouzon syndrome patients.









Similar content being viewed by others
References
Renier D, Lajeunie E, Arnaud E, Marchac D (2000) Management of craniosynostoses. Childs Nerv Syst 16(10–11):645–658
Seruya M, Oh AK, Boyajian MJ, Posnick JC, Keating RF (2011) Treatment for delayed presentation of sagittal synostosis: challenges pertaining to occult intracranial hypertension. J Neurosurg Pediatr 8(1):40–48
Morriss-Kay GM, Wilkie AO (2005) Growth of the normal skull vault and its alteration in craniosynostosis: insights from human genetics and experimental studies. J Anat 207(5):637–653
Kreiborg S (1981) Craniofacial growth in plagiocephaly and Crouzon syndrome. Scand J Plast Reconstr Surg 15(3):187–197
Cohen MM Jr (1993) Sutural biology and the correlates of craniosynostosis. Am J Med Genet 47:581–616
Okajima K, Robinson LK, Hart MA, Abuelo DN, Cowan LS, Hasegawa T, Maumenee IH, Jabs EW (1999) Ocular anterior chamber dysgenesis in craniosynostosis syndromes with a fibroblast growth factor receptor 2 mutation. Am J Med Genet 85(2):160–170
Stavrou P, Sgouros S, Willshaw HE, Goldin JH, Hockley AD, Wake MJ (1997) Visual failure caused by raised intracranial pressure in craniosynostosis. Childs Nerv Syst 13(2):64–67
Abe H, Ikota T, Akino M, Kitami K, Tsuru M (1985) Functional prognosis of surgical treatment of craniosynostosis. Childs Nerv Syst 1(1):53–61
Shah PS, Siriwardena K, Taylor G, Steele L, Ray P, Blaser S, Chitayat D (2006) Sudden infant death in a patient with FGFR3 P250R mutation. Am J Med Genet A 140(24):2794–2796
Rasmussen SA, Yazdy MM, Frías JL, Honein MA (2008) Priorities for public health research on craniosynostosis: summary and recommendations from a Centers for Disease Control and Prevention-sponsored meeting. Am J Med Genet A 146A(2):149–158
Cohen MM Jr, Kreiborg S (1992) Upper and lower airway compromise in the Apert syndrome. Am J Med Genet 44(1):90–93
Cunningham ML, Seto ML, Ratisoontorn C, Heike CL, Hing AV (2007) Syndromic craniosynostosis: from history to hydrogen bonds. Orthod Craniofac Res 10(2):67–81
Flapper WJ, Anderson PJ, Roberts RM, David DJ (2009) Intellectual outcomes following protocol management in Crouzon, Pfeiffer, and Muenke syndromes. J Craniofac Surg 20(4):1252–1255
Baird LC, Gonda D, Cohen SR, Evers LH, Lefloch N, Levy ML, Meltzer HS (2011) Craniofacial reconstruction as a treatment for elevated intracranial pressure. Childs Nerv Syst 28(3):411–418
Boyadjiev SA, International Craniosynostosis Consortium (2007) Genetic analysis of non-syndromic craniosynostosis. Orthod Craniofac Res 10(3):129–137
Wilkie AO, Byren JC, Hurst JA, Jayamohan J, Johnson D, Knight SJ, Lester T, Richards PG, Twigg SR, Wall SA (2010) Prevalence and complications of single-gene and chromosomal disorders in craniosynostosis. Pediatrics 126(2):e391–e400
Reardon W, Winter RM, Rutland P, Pulleyn LJ, Jones BM, Malcolm S (1994) Mutations in the fibroblast growth factor receptor 2 gene cause Crouzon syndrome. Nat Genet 8:98–103
Schell U, Hehr A, Feldman GJ, Robin NH, Zackai EH, de Die-Smulders C, Viskochil DH, Stewart JM, Wolff G, Ohashi H et al (1995) Mutations in FGFR1 and FGFR2 cause familial and sporadic Pfeiffer syndrome. Hum Mol Genet 4:323–328
Wilkie AO, Slaney SF, Oldridge M, Poole MD, Ashworth GJ, Hockley AD, Hayward RD, David DJ, Pulleyn LJ, Rutland P et al (1995) Apert syndrome results from localized mutations of FGFR2 and is allelic with Crouzon syndrome. Nat Genet 9:165–172
Ibrahimi OA, Zhang F, Eliseenkova AV, Linhardt RJ, Mohammadi M (2004) Proline to arginine mutations in FGF receptors 1 and 3 result in Pfeiffer and Muenke craniosynostosis syndromes through enhancement of FGF binding affinity. Hum Mol Genet 13:69–78
Eswarakumar VP, Horowitz MC, Locklin R, Morriss-Kay GM, Lonai P (2004) A gain-of-function mutation of Fgfr2c demonstrates the roles of this receptor variant in osteogenesis. Proc Natl Acad Sci USA 101:12555–12560
Yin L, Du X, Li C, Xu X, Chen Z, Su N, Zhao L, Qi H, Li F, Xue J, Yang J, Jin M, Deng C, Chen L (2008) A Pro253Arg mutation in fibroblast growth factor receptor 2 (Fgfr2) causes skeleton malformation mimicking human Apert syndrome by affecting both chondrogenesis and osteogenesis. Bone 42:631–643
Cohen MM Jr, Kreiborg S (1992) Birth prevalence studies of the Crouzon syndrome: comparison of direct and indirect methods. Clin Genet 41(1):12–15
Online Mendelian Inheritance in Man. Johns Hopkins University, Baltimore, MD. MIM number: 123500. http://omim.org/entry/123500. Accessed 22 June 2012
Perlyn CA, DeLeon VB, Babbs C, Govier D, Burell L, Darvann T, Kreiborg S, Morriss-Kay G (2006) The craniofacial phenotype of the Crouzon mouse: analysis of a model for syndromic craniosynostosis using three-dimensional microCT. Cleft Palate Craniofac J 43(6):740–748
Flippen JH Jr (1950) Cranio-facial dysostosis of Crouzon; report of a case in which the malformation occurred in four generations. Pediatrics 5(1):90–96
Holmes G, Rothschild G, Roy UB, Deng C, Mansukhani A, Basilico C (2009) Early onset of craniosynostosis in an Apert mouse model reveals critical features of this pathology. Dev Biol 328:273–284
Zhou YX, Xu X, Chen L, Li C, Brodie SG, Deng CX (2000) A Pro250Arg substitution in mouse Fgfr1 causes increased expression of Cbfa1 and premature fusion of calvarial sutures. Hum Mol Genet 9:2001–2008
Lomri A, Lemonnier J, Hott M, de Parseval N, Lajeunie E, Munnich A, Renier D, Marie PJ (1998) Increased calvaria cell differentiation and bone matrix formation induced by fibroblast growth factor receptor 2 mutations in Apert syndrome. J Clin Invest 101:1310–1317
Fragale A, Tartaglia M, Bernardini S, Di Stasi AM, Di Rocco C, Velardi F, Teti A, Battaglia PA, Migliaccio S (1999) Decreased proliferation and altered differentiation in osteoblasts from genetically and clinically distinct craniosynostotic disorders. Am J Pathol 154:1465–1477
Mansukhani A, Bellosta P, Sahni M, Basilico C (2000) Signaling by fibroblast growth factors (FGF) and fibroblast growth factor receptor 2 (FGFR2)-activating mutations blocks mineralization and induces apoptosis in osteoblasts. J Bone Miner Res 149:1297–1308
Chen L, Li D, Li C, Engel A, Deng CX (2003) A Ser252Trp [corrected] substitution in mouse fibroblast growth factor receptor 2 (Fgfr2) results in craniosynostosis. Bone 33:169–171
Wang Y, Sun M, Uhlhorn VL, Zhou X, Peter I, Martinez-Abadias N, Hill CA, Percival CJ, Richtsmeier JT, Huso DL, Jabs EW (2010) Activation of p38 MAPK pathway in the skull abnormalities of Apert syndrome Fgfr2(+P253R) mice. BMC Dev Biol 10:22
Twigg SR, Healy C, Babbs C, Sharpe JA, Wood WG, Sharpe PT, Morriss-Kay GM, Wilkie AO (2009) Skeletal analysis of the Fgfr3(P244R) mouse, a genetic model for the Muenke craniosynostosis syndrome. Dev Dyn 238(2):331–342
Richtsmeier JT, Baxter LL, Reeves RH (2000) Parallels of craniofacial maldevelopment in Down syndrome and Ts65Dn mice. Dev Dyn 217(2):137–145
Lele S, Richtsmeier JT (2001) An invariant approach to statistical analysis of shapes. Chapman & Hall/CRC, Boca Raton
Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Müller R (2010) Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res 25(7):1468–1486
Hatch N, Li Y, Franceschi RT (2009) FGF2 stimulated expression of the pyrophosphate generating enzyme, PC-1, is mediated by Runx2. J Bone Miner Res 24(4):652–662
McCarthy TL, Centrella M, Canalis E (1988) Further biochemical and molecular characterization of primary rat parietal bone cell cultures. J Bone Miner Res 3(4):401–408
Harris SE, Sabatini M, Harris MA, Feng JQ, Wozney J, Mundy GR (1994) Expression of bone morphogenetic protein messenger RNA in prolonged cultures of fetal rat calvarial cells. J Bone Miner Res 9(3):389–394
Ducy P, Karsenty G (1995) Two distinct osteoblast-specific cis-acting elements control expression of a mouse osteocalcin gene. Mol Cell Biol 15(4):1858–1869
Martínez-Abadías N, Heuzé Y, Wang Y, Jabs EW, Aldridge K, Richtsmeier JT (2011) FGF/FGFR signaling coordinates skull development by modulating magnitude of morphological integration: evidence from Apert syndrome mouse models. PLoS One 6(10):e26425
Holmes G, Basilico C (2012) Mesodermal expression of Fgfr2S252 W is necessary and sufficient to induce craniosynostosis in a mouse model of Apert syndrome. Dev Biol 368(2):283–293
Li S, Quarto N, Longaker MT (2010) Activation of FGF signaling mediates proliferative and osteogenic differences between neural crest derived frontal and mesoderm parietal derived bone. PLoS One 5(11):e14033
Behr B, Panetta NJ, Longaker MT, Quarto N (2010) Different endogenous threshold levels of fibroblast growth factor ligands determine the healing potential of frontal and parietal bones. Bone 47(2):281–294
Quarto N, Behr B, Li S, Longaker MT (2009) Differential FGF ligands and FGF receptors expression pattern in frontal and parietal calvarial bones. Cells Tissues Organs 190(3):158–169
Iseki S, Wilkie AO, Heath JK, Ishimaru T, Eto K, Morriss-Kay GM (1997) Fgfr2 and osteopontin domains in the developing skull vault are mutually exclusive and can be altered by locally applied FGF2. Development 124:3375–3384
Iseki S, Wilkie AO, Morriss-Kay GM (1999) Fgfr1 and Fgfr2 have distinct differentiation- and proliferation-related roles in the developing mouse skull vault. Development 126:5611–5620
Lemonnier J, Haÿ E, Delannoy P, Fromigué O, Lomri A, Modrowski D, Marie PJ (2001) Increased osteoblast apoptosis in Apert craniosynostosis: role of protein kinase C and interleukin-1. Am J Pathol 158(5):1833–1842
Acknowledgments
We thank Dr. David Ornitz for providing the FGFR2C342Y/+ mice. This work was supported by NIH/NIDCR Grant R03DE021082.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have stated that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Liu, J., Nam, H.K., Wang, E. et al. Further Analysis of the Crouzon Mouse: Effects of the FGFR2C342Y Mutation Are Cranial Bone–Dependent. Calcif Tissue Int 92, 451–466 (2013). https://doi.org/10.1007/s00223-013-9701-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-013-9701-2