Abstract
Rationale
Major depressive disorder (MDD) is a severe mental disorder with affective, cognitive, and somatic symptoms. Mood congruent cognitive biases, including a negative attentional bias, are important for development, maintenance, and recurrence of depressive symptoms. MDD is associated with maladaptive changes in the biological stress systems such as dysregulations of central noradrenergic alpha2-receptors in the locus coeruleus-noradrenergic system, which can affect cognitive processes including attention. Patients with adverse childhood experiences (ACE), representing severe stress experiences in early life, might be particularly affected.
Objectives
With an experimental design, we aimed to gain further knowledge about the role of noradrenergic activity for attentional bias in MDD patients with and without ACE.
Methods
We tested the effect of increased noradrenergic activity induced by the alpha2-receptor blocker yohimbine on attentional bias in a placebo-controlled repeated measures design. Four groups were included as follows: MDD patients with and without ACE, and healthy participants with and without ACE (total N = 128, all without antidepressant medication).
Results
A significant effect of MDD on attentional bias scores of sad face pictures (p = .037) indicated a facilitated attentional processing of sad face pictures in MDD patients (compared to non-MDD individuals). However, we found no such effect of ACE. For attentional bias of happy face pictures, we found no significant effects of MDD and ACE. Even though a higher increase of blood pressure and salivary alpha-amylase following yohimbine compared to placebo indicated successful noradrenergic stimulation, we found no significant effects of yohimbine on attentional bias of happy or sad face pictures.
Conclusions
Our results are consistent with the hypothesis of a negative attentional bias in MDD patients. However, as we found no effect of ACE or yohimbine, further research is needed to understand the mechanisms by which ACE increases the risk of MDD and to understand the biological basis of the MDD-related negative attentional bias.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Major depressive disorder (MDD) is a serious mental disorder associated with high subjective suffering and pronounced functional disruptions (Ferrari et al. 2013; Otte et al. 2016; Saarni et al. 2007). Among other symptoms, MDD patients suffer from low mood, lack of motivation and cognitive dysfunction. Mood congruent cognitive biases in the processing of emotional information, such as an attentional bias for negative stimuli (Armstrong and Olatunji 2012; Caseras et al. 2007; Mathews and MacLeod 2005; Peckham et al. 2010), are a prominent feature of MDD and have been implicated in the development, maintenance, and treatment of MDD (Beck & Bredemeier, 2016; Joormann and Quinn 2014; LeMoult and Gotlib 2019). Furthermore, MDD patients tend to interpret ambiguous information more negatively compared to healthy individuals (Lawson et al. 2002; Lee et al. 2016; Orchard et al. 2016; Voncken et al. 2007) and to a memory bias for negative information (Bradley et al. 1996; Gaddy and Ingram 2014; Mathews and MacLeod 2005; Power et al. 2000; Taylor and John 2004; Watkins et al. 2000; Watkins et al. 1996; Yang et al. 2016).
Several studies indicate an unfavorable relation of dysregulations in the biological stress systems in MDD and cognitive performance (Behnken et al. 2013; Gomez et al. 2006; Harmer et al. 2009; Hinkelmann et al. 2009, 2013; O'Hara et al. 2007; Schlosser et al. 2011; Wingenfeld et al. 2013), mainly with a focus on cortisol and the hypothalamic–pituitary–adrenal axis and to a lower extend on the locus coeruleus-noradrenaline (LC-NA) system. Since the noradrenergic system has an impact on cognitive processes (Chamberlain and Robbins 2013; Mather et al. 2016; Sara 2016) and attentional biases (Ehlers and Todd 2017), dysregulations of the LC-NA system could play an important role in cognitive dysfunctions associated with MDD. Enhanced binding capacity of central noradrenergic alpha2-receptors, especially in the LC and prefrontal cortex areas, were found in MDD patients (Callado et al. 1998; Cottingham and Wang 2012; Garcia-Sevilla et al. 1999; Goddard et al. 2010; Meana et al. 1992; Ordway et al. 2003; Rivero et al. 2014). Because alpha2-receptors are involved in the autoregulation of NA release, this might lead to lower central NA levels and in turn affect cognitive processes. Described effects of NA activity on cognitive processes include allocation of attentional resources and processing of emotional material, e.g., emotional learning and memory (Giustino and Maren 2018) as well as emotion recognition (Oliva and Anikin 2018) and biased attention based on associative learning processes (Ehlers and Todd 2017). Emotional information is often processed differently from neutral information and depends on the valence of the information and its meaning for the individual. This leads to biased processing of emotional information. This bias also seems to be affected by NA activity. For example, Vasa et al.’s study (Vasa et al. 2009) demonstrated an attentional bias for angry faces following placebo that was vanished following single administration of the NA alpha-2 receptor blocker yohimbine. MDD associated alterations in the LC-NA system might contribute to negative biases in processing of emotional information in MDD patients. First experimental investigations suggest increased sensitivity for noradrenergic stimulation regarding cognitive alterations in MDD. A single administration of the NA reuptake inhibitor reboxetine could reverse negative bias in emotional processing such as emotion recognition and memory of self-relevant information in MDD patients (Harmer et al. 2009). A study from our group (Wingenfeld et al. 2013) demonstrated a positive effect of a single administration of the alpha2-receptor blocker yohimbine on memory consolidation, which was more prominent in MDD patients compared to healthy controls. Again, NA stimulation seemed to compensate for the adverse effects of MDD on cognition. As the effect of NA stimulation on memory was significantly affected by self-reported childhood adversity in the group of MDD patients, alterations in the LC-NA system might be especially pronounced in a subgroup of MDD patients with a history of childhood adversity.
Adverse childhood experiences (ACE) such as emotional neglect, sexual or physical abuse seem to play an important role in the development of vulnerability to depression and about one half of MDD patients have ACE in their biography (Nelson et al. 2017; Nemeroff 2016). On the one hand, ACE represent severe stressors and can contribute to alterations in the biological stress systems (Flugge et al. 2003; Heim and Nemeroff 2002; Ladd et al. 1996; Meaney et al. 1995; Otte et al. 2016; Plotsky and Meaney 1993). Accordingly, some experimental studies have demonstrated a higher NA reactivity to stress in individuals with ACE compared to those without ACE (Heim et al. 2000; Kuras et al. 2017; Otte et al. 2005). On the other hand, ACE have been associated with alterations in cognitive performance later in life (Hedges and Woon 2011; Lovallo et al. 2013; Pechtel and Pizzagalli 2011) including modification of cognitive biases for emotional information (Herzog et al. 2018; Pfaltz et al. 2019; Vrijsen et al. 2015). These ACE-related alterations may contribute to the increased vulnerability to MDD in individuals with childhood adversity. Indeed, a few studies on attentional bias in MDD included ACE in their analysis and found associations between attentional biases for emotional faces and ACE in MDD patients (Bodenschatz et al. 2019; England-Mason et al. 2018; Günther et al. 2015). However, this means, if ACE is not systematically included on studies on attentional bias in MDD, effects of MDD and ACE could be easily confounded. It therefore seems important to include ACE as a factor in the design of such studies.
As mentioned above, a negative attentional bias may contribute to the development, maintenance, and treatment of MDD. It is therefore important to better understand the underlying biological mechanisms of these relationships. In this study, we aimed to investigate whether alterations in the LC-NA system of MDD patients, e.g., in alpha-2 receptor functioning, may contribute to biased attention for emotional information. Our study used an emotional dot probe task as a measure of attentional bias, conducted after administration of the alpha2-receptor blocker yohimbine, which stimulates NA activity, and after placebo in a repeated measures design. We included four groups to implement a study design in which the factors MDD and ACE were fully crossed to disentangle the potential role of ACE: MDD patients with and without ACE, and healthy participants with and without ACE (all without antidepressant medication).
Importantly, MDD often co-occurs with anxiety, and measures of depression and anxiety correlate highly. Although both conditions are characterized by negative affectivity and share overlapping features, both are separate functional entities that can be conceptually differentiated. Depression is generally associated with goal loss and lack of positive affect (anhedonia); depressive processing and cognitive style is biased toward past mistakes and failures and an enhanced focus on the individual’s personal and emotional world. In contrast to this past-oriented, ruminative thinking, anxiety is future-oriented and focused on the prevention of harm and loss (Eysenck and Fajkowska 2018). Previous studies have been able to show an influence on attentional biases for both conditions (Bar-Haim et al. 2007; Kircanski and Gotlib 2015; Klein et al. 2018). However, while anxiety is associated with faster orienting to threatening stimuli such as angry facial expression, depression is characterized by a difficulty in disengaging from dysphoric content (Armstrong and Olatunji 2012). Since we expected higher measures of anxiety for the MDD groups, yet wanted to investigate attentional biases genuinely for MDD (Peckham et al. 2010), we deliberately chose depression-relevant stimuli with happy and sad facial expressions.
We hypothesized (1) an attentional bias toward sad face stimuli and away from positive face stimuli (as measured by the dot probe paradigm) in MDD compared to non-MDD. (2) The effect of MDD on attentional bias should be reduced following intake of yohimbine, due to increasing NA activity, and (3) this reduction should be especially pronounced in interaction with ACE.
Methods
Participants
This study was part of a larger research project, which will be and has been reported elsewhere (de Punder et al. 2018; Deuter et al. 2020; Kuehl et al. 2019; Schulz et al. 2021).The study design was approved by the ethical committee of the German Psychological Society to adhere to the Declaration of Helsinki. All participants provided written informed consent. Healthy participants and outpatients received monetary compensation (100 €) for their participation. Patients with MDD and healthy participants were recruited by public postings and from our specialized affective disorder unit at the Department of Psychiatry and Psychotherapy, Campus Benjamin Franklin, Charité—Universitätsmedizin Berlin.
Depressed patients were included if they fulfilled criteria for a current episode of MDD as assessed by a trained psychologist, using a German version of the Structured Clinical Interview for DSM-IV axis I (SCID-I) to validate psychiatric diagnoses (Wittchen et al. 1997). In addition to the SCID-I interview, current depressive symptoms were captured by a clinical rating scale and a questionnaire, the Montgomery Asberg Depression Rating Scale (MADRS) (Montgomery and Asberg 1979; Williams and Kobak 2008) and the Beck Depression Inventory (BDI) (Beck, Steer, & Hautzinger, 1994). ACE was defined as repeated physical or sexual abuse at least once a month over 1 year or more (adapted from Heim et al. 2000) before the age of 18, assessed by a screening interview, and validated by the German version of the semi-structured interview, the Early Trauma Inventory (Bremner et al. 2000; Wingenfeld et al. 2011). Additionally, adverse childhood experiences were measured using a German version of the Childhood Trauma Questionnaire (CTQ) (Bernstein et al. 2003; Wingenfeld et al. 2010). In the MDD groups, schizophrenia, schizoaffective disorder, bipolar disorder, depressive disorder with psychotic features, dementia, abuse of alcohol or drugs, and panic disorder led to exclusion. Healthy participants with and without ACE were free of any current mental disorder. Further exclusion criteria for all participants were CNS relevant diseases, neurological diseases, severe somatic diseases, diabetes type 1 and 2, steroid diseases, hypertonia, current infections, pregnancy, and the intake of psychotropic medication. Physical health criteria were checked by physical examination, clinical interview, and blood test.
The final sample consisted of 128 participants with completed measurements on both days: 27 MDD patients with ACE (MDD + /ACE +), 26 MDD patients without ACE (MDD + /ACE -), 29 participants with ACE but no current or lifetime MDD (MDD - /ACE +), and 46 participants with no current or lifetime MDD and no childhood adversity (MDD -/ACE -).
Procedure
Diagnostic assessment took place on a separate day prior to the laboratory testing and included psychiatric and medical assessment (for more details, see Kuehl et al. 2020). Participants were tested on two separate laboratory sessions. Experimental setup was identical on both days, except for the oral administration of either yohimbine (10 mg) or placebo in a double-blind, quasi-randomized design. All participants had to refrain from strenuous physical activity and caffeine consumption on the testing days. When they arrived at the laboratory at 09:30 h, participants were seated in a comfortable chair, provided a first saliva sample and blood pressure was measured after a 5 min resting period. Thereafter, participants were orally administered either yohimbine or placebo (09:45 h). Participants then waited 60 min (until 10:45) to allow digestive absorption of the drug.
The dot probe test started at 11:15 h, had a duration of approximately 15 min and was part of an extended study setup, which will be and has been reported elsewhere (Deuter et al. 2020; Kuehl et al. 2020; Schulz et al. 2021). As previous studies demonstrated a plasma peak level of yohimbine at 90 min after oral intake (O'Carroll et al. 1999; Peskind et al. 1995), drug effects were assumed to be present at testing time. The experimental tests had a total duration of approximately 70 min. The total duration of the experimental setup was approx. 2.5 h. The time between the two test sessions was at least 1 day with an average interval of 5.7 days (SD: 5.8). The order of interventions according to drug order (yohimbine vs. placebo) and test version (version A vs. version B) was counterbalanced between participants according to group assignment in a quasi-randomized way to minimize order effects.
Emotional dot probe paradigm
For the emotional dot-probe paradigm, we used a computer-based, emotional version of the visual dot-probe paradigm, which is a measure of selective attention toward emotional cues (MacLeod et al. 1986). A set of human faces from the FACES database (Ebner et al. 2010) was used, comprising 20 different persons (10 female, 10 male; different from persons whose pictures served as face stimuli in the approach avoidance paradigm) with happy, sad, and neutral facial expressions. A set of two pictures with human faces was shortly presented on a computer screen (for 500 ms), serving as stimuli. A picture set always consisted of two facial expressions of the same person, either paired as neutral-sad, neutral-happy, or neutral–neutral. One of these pictures was presented on the left side of the computer screen, the other picture on the right side. Afterwards, either the left or the right picture was replaced by a vertical bar which served as the cue (1100 ms). The participants were instructed to pay attention only to the cues and press one of two keys (left vs. right) as fast as possible in reaction to the cue´s position. The attentional capture was reflected in the response latency. It is assumed that participants react faster when the cue replaces the picture at which they antecedently concentrated their attention on. Emotional stimuli are assumed to bind more attention compared to neutral stimuli. In a congruent trial, the cue replaced the location of an emotional stimulus (positive or negative facial expression). In an incongruent trial, the cue replaced a neutral stimulus (neutral facial expression) (please see Fig. 1). In total, 200 trials were presented: 40 trials in the neutral condition, 40 trials in the positive congruent condition, 40 trials in the negative congruent condition, 40 trials in the positive incongruent condition, and 40 trials in the negative incongruent condition. The position of the facial pictures was counterbalanced between left and right, and the order between all trials was quasi-randomized. The total duration of the test was about 15 min. The “attentional bias index” can be determined by calculating the average reaction time for incongruence minus congruence (MacLeod and Mathews 1988; Tsumura and Shimada 2012):
Procedure of the emotional dot probe task: after presentation of a fixation cross (500 ms), a pair of face pictures of the same person occurred (500 ms) followed by a bar (1100 ms). Subjects were asked to respond to the bar with either left or right keystroke according to the position of the bar. In congruent trials, the bar replaced the position of a face picture with an emotional expression (happy or sad), in incongruent trials, the bar replaced the position of a face picture with neutral expression.
Attentional bias index = ½ [(incogruence right − congruence right) + (incongruence left − congruence left)].
A positive attentional bias index score can be interpreted as an attentional bias toward the emotional stimulus, i.e., attention toward the happy or sad faces and a negative score as an attentional bias toward the neutral stimulus, i.e., avoiding the sad or happy faces.
We used the E-Prime 2.0 presentation software for stimulus presentation and data acquisition. Randomization of task lists was performed using RQube (Seifert and Britz 2007).
Physiological measurements
Blood pressure measurement
Discrete blood pressure measurements were taken using a standard, automated pressure cuff, which was fixed around the right upper arm (Dinamap 1846 SX). Blood pressure was measured 10 min before intake of yohimbine (pre) and 60, 90, 120, and 150 min after intake of yohimbine (post).
Assessment and analysis of salivary alpha-amylase
Six saliva samples were collected on each laboratory session in order to determine salivary-free alpha-amylase (sAA). All patients and participants had to refrain from eating for 2 h before testing and from drinking for 30 min before each saliva sample collection. All participants received instructions on the correct use of the Salivette salivary collection device (Salivettes®, blue cap; Sarstedt AG, Nümbrecht, Germany). Saliva samples were taken 15 and 5 min before intake of yohimbine (pre) and 60, 90, 120, and 150 min after intake of yohimbine (post). All samples were immediately stored on ice and subsequently stored at − 80 °C before biochemical analyses were performed in the Neurobiology Laboratory of the Department of Psychiatry, Charité Universitätsmedizin Berlin. The salivary alpha-amylase activity was determined using a modified protocol of a previously published direct alpha-amylase assay (Lorentz et al. 1999). Inter- and intra-assay coefficients of variation were both lower than 10% for sAA activity.
Statistical analysis
SPSS version 27.0 was used for all statistical analyses.
Demographic and clinical characteristics, including depression and childhood trauma scores in all subscales of the BDI-II, the MADRS, the CTQ, and the ETI, were analyzed with one-way ANOVA for continuous variables or chi2 test for dichotomous variables across groups. Blood pressure and sAA were evaluated using an analysis of variance (ANOVA), with the between-subjects factor “group” (MDD + /ACE + , MDD + /ACE - , MDD - /ACE + , MDD - /ACE -) and the within-subjects factors “treatment” (yohimbine vs. placebo) and “time.” Before analysis, data of salivary alpha-amylase were log-transformed because values were not normally distributed. To analyze differences between groups, Bonferroni corrected post-hoc tests were used.
To analyze the influence of yohimbine administration on attentional bias for happy and sad face expressions, we used 2 × 2 × 2 repeated measures ANOVAs with “treatment” (yohimbine vs. placebo) as within-subject factor and “MDD” (MDD vs. non MDD) and “ACE” (ACE vs. non ACE) as between-subject factor to analyze attentional biases for happy and sad face stimuli separately (Joormann and Gotlib 2007). Attentional bias indices were first calculated from reaction times as described above (see the “Emotional dot probe paradigm” section). Reaction times that were less than 100 ms (anticipation error) or greater than 1500 ms (lack of concentration) were excluded from statistical analyses to reduce the influence of ouliers.
A p-value smaller than 0.05 was considered to indicate statistical significance. In the case of violations of sphericity, reported p values were Greenhouse–Geisser corrected.
Results
Sample characteristics
For demographic and clinical data of the final sample, please see also Table 1.
We found no significant differences between groups regarding sex, age, body mass index, and education level. In women only, we found no significant group differences in use of hormonal contraceptives, cycling phases between groups on both testing days (day 1: χ2 = 4.02, df = 6, p = 0.68; day 2: χ2 = 3.96, df = 6, p = 0.68) nor in state of menopause (yes/no) (χ2 = 1.51 df = 3, p = 0.68). Furthermore, clinical characteristics of MDD patients did not differ between MDD patients with and without ACE (MDD + /ACE + , MDD + /ACE -) in regard to age at MDD onset and length of current MD episode. However, time since MDD onset was longer in MDD patients with ACE (MDD + /ACE +), which may be explained by their slightly older age, even though not significant, at study participation. As expected and also presented in earlier publications of this research project (de Punder et al. 2018; Deuter et al. 2020; Kuehl et al. 2020; Schulz et al. 2021), MADRS and BDI sum scores were significantly higher in the MDD groups (MDD + /ACE - , MDD + /ACE +) compared to the two healthy groups (MDD - /ACE - , MDD - /ACE +). There were no significant differences in MADRS and BDI sum scores in between the MDD groups (MDD + /ACE - , MDD + /ACE +) and the healthy groups (MDD - /ACE - , MDD - /ACE +). In addition to the main diagnosis of current major depression, twelve MDD + /ACE + patients (phobia: N = 3, PTSD [related to ACE]: N = 5, personality disorders: N = 4, dysthymia: N = 1, bulimia nervosa: N = 1, somatoform pain disorder: N = 1) and six MDD + /ACE - patients (phobia: N = 2, personality disorders: N = 2, dysthymia: N = 1, somatoform pain disorder: N = 1) fulfilled the criteria for one or more mental comorbid disorders. As expected due to our recruitment criteria, ETI and CTQ sum scores were higher in the groups with ACE (MDD + /ACE + , MDD - /ACE +) compared to the groups without ACE (MDD + /ACE - , MDD - /ACE -): ETI sum scores were significantly higher in the ACE + groups (MDD + /ACE + , MDD - /ACE +) compared to the ACE - groups (MDD + /ACE - , MDD - /ACE -) with no significant differences within groups with ACE (MDD + /ACE + , MDD - /ACE +) and groups without ACE (MDD + /ACE - , MDD - /ACE -). Higher CTQ sum scores were observed in the ACE + groups (MDD + /ACE + , MDD - /ACE +) compared to the ACE - groups (MDD + /ACE - , MDD - /ACE -). Sum scores of the additionally assessed STAI-T (trait version of the State-Trait Anxiety Inventory (STAI-T; Laux et al. 1981)) were significantly higher in the two MDD groups (MDD + /ACE - , MDD + /ACE +) compared to the two healthy groups (MDD - /ACE - , MDD - /ACE +) with no significant differences within both MDD groups, but a significant higher averaged STAI-T score in the MDD - /ACE + group compared the MDD - /ACE - group.
Physiological measures
All physiological measures showed a significant increase over time that was more pronounced following yohimbine compared to placebo as displayed by significant interaction effects of “time” and “treatment” for sAA (F5,535 = 10.06, p < 0.001) as well as for systolic (F4,452 = 20.64, p < 0.001) and diastolic blood pressure (F4,422 = 7.75, p < 0.001). Please see also Fig. 2. More detailed results are presented in Kuehl et al. (2020).
Attentional bias
Reaction times that were less than 100 ms (anticipation error) or greater than 1500 ms (lack of concentration) were excluded from statistical analyses to reduce the influence of ouliers. This was the case for N = 3 (one MDD patient without ACE, two healthy participants without ACE). Only reaction times from correct responses were analyzed. Overall, data of three participants were excluded due to less than 50% correct responses on one or both test sessions, indicating insufficient comprehension of the task rules (MDD + /ACE - : N = 1, MDD - /ACE - : N = 2). The percentage of correct answers was on average 99% or above in all test conditions in all groups.
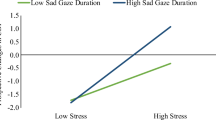
2 × 2 × 2 repeated measures ANOVAs with “treatment” (yohimbine vs. placebo) as within-subject factor and “MDD” (MDD vs. non MDD) and “ACE” (ACE vs. non ACE) as between-subject factors were conducted for happy and sad face pictures, separately. For happy face pictures, no significant main effects of “treatment” (F1,124 = 0.24, p = 0.624, partial eta2 = 0.002), “MDD” (F1,124 = 0.55, p = 0.461, partial eta2 = 0.004) or “ACE” (F1,124 = 0.50, p = 0.483, partial eta2 = 0.004) and no significant interaction effects were found. For sad face pictures, repeated measures ANOVA of bias scores revealed a significant main effect of “MDD” (F1,124 = 4.45, p = 0.037, partial eta2 = 0.035), indicating that MDD patients directed more attention to sad facial expressions (please see Fig. 3). There were no significant main effects of “treatment” (F1,124 = 0.05, p = 0.828, partial eta2 < 0.001) or “ACE” (F1,124 = 1.14, p = 0.289, partial eta2 = 0.009) and no significant interaction effects. The results did not change, when we controlled for drug order (placebo/yohimbine). In addition, there was no effect of test session order.
Attentional bias scores (reaction times (ms) of incongruent minus congruent trials with 95% confidence intervals indicated) toward and away from emotional face pictures (happy, sad) in the dot probe task according to (3a) major depressive disorder (MDD) across the factors “ACE” and “drug condition,” (3b) adverse childhood experiences (ACE) across the factors “MDD” and “ drug condition,” and (3c) experimental drug condition (placebo vs. yohimbine) across the factors “MDD” and “ACE”.
Discussion
To investigate the potential influence of the noradrenergic system on a negative attentional bias in individuals with major depression and childhood adversity, we tested the effect of enhanced noradrenergic activation induced by acute administration of the alpha2-receptor blocker yohimbine on attentional biases. An emotional dot probe task served as a measure of attentional bias. We further aimed to investigate biased attention influenced by NA activity as a potential mechanism for how ACE contribute to vulnerability to and maintenance of MDD.
We tested different hypotheses, investigating the effects of MDD on biased attentional processing per se and the possible influence of noradrenergic stimulation and ACE. These hypotheses have been partially confirmed. Our results show a significant effect of MDD when attentional bias scores for sad face pictures were analyzed. This could be carefully interpreted as facilitated attentional processing of sad emotional pictures in MDD patients (compared to non-MDD individuals), consistent with the hypothesis of a negative attentional bias in patients with MDD. Contrary to what was originally hypothesized, this effect was neither significantly increased by ACE nor decreased by the administration of yohimbine; these factors did not affect attentional processing.
An attentional bias of MDD patients for sad, but not happy faces in comparison to non-MDD, has been described before, especially as difficulty in disengaging attention from negative stimuli (Armstrong and Olatunji 2012; Caseras et al. 2007; Eizenman et al. 2003; Mathews and MacLeod 2005). Of note, we found no differences in attention bias scores of happy faces between MDD patients and non-MDD participants. This is in contrast to our hypothesis of an attentional bias away from positive face stimuli in MDD patients compared to non-MDD participants. A meta-analysis (Winer and Salem 2016) provides evidence for avoidance of positivity in depressed patients. The authors interpret this as arising from reward devaluation, rather than from initial lack of reward valuation. However, many dot-probe studies did not find effects of MDD for happy stimuli (e.g., (Gotlib et al. 2004; Zhou et al. 2015)). Interestingly, in a systematic investigation series regarding the dot probe paradigm in healthy participants, Puls and Rothermund (Puls and Rothermund 2018) demonstrated no evidence for a general effect for emotional faces in dot probe tasks for healthy participants, leading to the conclusion that individuals do not attend automatically to emotional faces. Furthermore, the authors state that attentional capture for specific emotional stimuli should be much more likely to occur if these stimuli are made relevant for the participants. Our results are in line with the assumption that only sad faces served as relevant stimuli primarily for MDD patients and captured their attention, thereby leading to an attentional bias toward sad faces. Happy faces might not have been relevant enough for MDD patients, and neither happy nor sad faces might have been relevant enough for healthy individuals, so no bias toward those pictures occurred. A mood congruent bias of MDD patients toward sad faces could be thus explained. However, previous studies using dot probe paradigms usually found a mood-congruent attention bias in MDD patients only when longer stimuli exposures than in our study were used (Joormann and Quinn 2014; LeMoult and Gotlib 2019). While MDD in itself biased attentional processing of sad facial stimuli, we did not find an effect of yohimbine administration or a history of childhood trauma on attentional bias.
An absence of the yohimbine effect raises the question of wether the dose of administered yohimbine was high enough to raise noradrenergic activity to an effective level. Indeed, our dose was lower compared to other studies that found effects on cognitive processes (e.g., O'Carroll et al. 1999; Soeter and Kindt 2011, 2012). However, in a study by Wingenfeld et al. (Wingenfeld et al. 2013), only 5 mg were administered, yet this still had an effect on memory. Furthermore, an increase in blood pressure and saliva alpha amylase indicates a sufficient effect on noradrenergic activity. However, these are measures from the periphery, and in the absence of any direct measure of central effects, we cannot make a final statement about the actual central NA activity.
Another explanation might be that noradrenergic activation simply has no effect on attentional bias for emotional face stimuli. However, a study by Vasa et al. (Vasa et al. 2009) found an effect of yohimbine administration, in that a bias toward angry faces under placebo was absent under yohimbine. Still, that study investigated only healthy participants and used other emotional facial expressions as stimuli compared to our study. Since we tested only sad and happy, but not angry or any further emotional facial expressions in our paradigm, we can only speculate about the specific role of distinct emotions for the effect of noradrenergic activity. As increased noradrenergic activity, as for example resulting from yohimbine administration, has been linked to anxiety and fear (for review Bremner et al. 1996a, b; Tanaka et al. 2000)), anxiety-related emotional stimuli such as fearful or angry faces might be more affected. In a series of studies (Harmer et al. 2003; Harmer et al. 2004; Murphy et al. 2009) that compared effects of selective serotonin reuptake inhibitors (SSRI) versus selective noradrenaline reuptake inhibitors (SNRI) on several cognitive biases in healthy participants found overall increased processing of positive material compared to negative material for both antidepressant drugs. However, there was no effect of a noradrenergic challenge by SNRI on attentional bias for fearful faces, but of SSRI based on a serotonergic mechanism (Murphy et al. 2009). Overall, the authors suggest a more depression specific effect of a noradrenergic intervention with SNRI, while SSRIs seem to work for anxiety-related material as well. Of note, two of the studies (Harmer et al. 2004; Murphy et al. 2009) used a short-term intervention of seven days and not an acute single drug administration as in our study.
While we found neither an effect of ACE nor an interaction effect of ACE x MDD, some studies indicate associations between attentional biases for emotional material and ACE (Bodenschatz et al. 2019; England-Mason et al. 2018; Günther et al. 2015; Wells et al. 2014). However, most of these studies found rather specific ACE-related associations such as in postpartum women with greater experiences of maltreatment and difficulties with emotion regulation (England-Mason et al. 2018) or under cognitive load condition solely (Wells et al. 2014). In the study of Bodenschatz et al. (Bodenschatz et al. 2019), ACE were associated with reduced attention for angry and sad facial expressions in depressed patients. As we only used sad facial expressions as negative stimuli, we can only speculate about an emotion specific attentional biases in MDD patients with ACE. In Günther et al.’s study (Günther et al. 2015), however, attentional bias toward sad facial expressions was positively correlated with severity of ACE in MDD patients. In contrast to our study, a longer stimulus duration of 1000 ms was used. As earlier studies found attention bias in MDD patients only with longer stimuli durations (Joormann and Quinn 2014; LeMoult and Gotlib 2019), this might also explain the discrepancy between the results. While our results cannot support an effect of ACE on attention bias, our results are in line with a study of Vrijsen et al. (Vrijsen et al. 2014) that investigated associations between ACE, biased information processing and depression onset and recurrence in a large sample of formerly depressed individuals, and found no evidence for an association between ACE and depression-related biased information processing. Taken together, the existing body of research provides insufficient information to explain fully how an attentional bias in MDD patients might be related (or not) to a history of ACE.
Of note, the reliability of the dot probe task has been subject to criticism. In his work, Schmukle (Schmukle 2005) fundamentally questioned the validity of the results and the test–retest reliability of the dot probe paradigm in non-clinical studies. He repeatedly administered the same task to a sample of healthy participants and found substantially divergent results. Further studies produced null results or found a lack of reliability as well, indicating an absence of emotional validity effects in the classical dot probe task using emotional words of facial expressions (Chapman et al. 2019; Puls and Rothermund 2018; Staugaard 2009). Similar problems exist with other behavioral response tasks that build on attentional allocation to task-irrelevant emotional faces (Tannert and Rothermund 2020; Victeur et al. 2020). This must be taken into account when interpreting our results. However, it is of importance that the studies criticizing the properties of the task were conducted with healthy participants. In clinical populations, the effects of emotional stimuli, with their ability to capture and bind attention, may be dissimilar and more pronounced (Yiend 2010). This again is also supported by the numerous previous studies listed in the introduction, which were able to demonstrate aberrant response patterns in patients with MDD (Armstrong and Olatunji 2012; Caseras et al. 2007; Mathews and MacLeod 2005; Peckham et al. 2010).
Limitations
The results of our study must be interpreted with caution due to some limitations. Firstly, our emotional stimuli material consisted of happy and sad facial expression only, which limits the comparability between different emotions. Especially for effects of ACE and NA effects, a further comparison with angry and fearful facial expressions as additional face stimuli would have been of great interest. Additionally, we only used short stimuli durations. Interestingly, this is the first study that could demonstrate an attentional bias in MDD patients even with short stimulus duration of 500 ms. However, we cannot exclude that effects of ACE and yohimbine might be found with longer stimuli durations. Even though a negative attentional bias has been more consistently found in MDD when face pictures compared to words were used as stimuli (for review (LeMoult and Gotlib 2019)), it is possible that using more personally relevant stimuli could have increased subjective salience and thus overall attentional vigilance toward the stimuli, which in turn might have led to detection of an effect in individuals with ACE. Furthermore, we did not use different dosages of yohimbine, which limits conclusions about potential dose–response-relations between noradrenergic activity and effects on attentional bias. Even though the results for blood pressure and salivary alpha-amylase indicate an increase in noradrenergic activity after yohimbine intake, it should be noted that these are only indirect measures of potential NA effects on a central level.
Conclusions
In summary, our study results are consistent with the hypothesis of a negative attentional bias in patients with MDD. In contrast to our hypotheses, we found no association of negative attentional bias with childhood adversity or with an acute stimulation of the noradrenergic system. Further research is needed to understand by which mechanisms childhood adversity increases the risk for MDD and to understand the biological basis of the MDD-related negative attentional bias.
References
Armstrong T, Olatunji BO (2012) Eye tracking of attention in the affective disorders: a meta-analytic review and synthesis. Clin Psychol Rev 32(8):704–723. https://doi.org/10.1016/j.cpr.2012.09.004
Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, van, IMH (2007) Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychol Bull 133(1), 1-24. doi:https://doi.org/10.1037/0033-2909.133.1.1
Beck AT, Steer RA, Hautzinger M (1994) Beck-depressions-inventar:(bdi); testhandbuch. Huber
Behnken A, Bellingrath S, Symanczik JP, Rieck MJ, Zavorotnyy M, Domschke K, . . . Zwanzger P (2013) Associations between cognitive performance and cortisol reaction to the DEX/CRH test in patients recovered from depression. Psychoneuroendocrinology, 38(3), 447-454. https://doi.org/10.1016/j.psyneuen.2012.07.005
Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, . . . Zule W (2003) Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl 27(2), 169-190
Bodenschatz CM, Skopinceva M, Ruß T, Suslow T (2019) Attentional bias and childhood maltreatment in clinical depression - an eye-tracking study. J Psychiatr Res 112:83–88. https://doi.org/10.1016/j.jpsychires.2019.02.025
Bradley BP, Mogg K, Millar N (1996) Implicit memory bias in clinical and non-clinical depression. Behav Res Ther 34(11–12):865–879. https://doi.org/10.1016/s0005-7967(96)00074-5
Bremner JD, Krystal JH, Southwick SM, Charney DS (1996a) Noradrenergic mechanisms in stress and anxiety: I Preclinical Studies. Synapse 23(1):28–38. https://doi.org/10.1002/(sici)1098-2396(199605)23:1%3c28::Aid-syn4%3e3.0.Co;2-j
Bremner JD, Krystal JH, Southwick SM, Charney DS (1996b) Noradrenergic mechanisms in stress and anxiety: II Clinical Studies. Synapse 23(1):39–51. https://doi.org/10.1002/(sici)1098-2396(199605)23:1%3c39::Aid-syn5%3e3.0.Co;2-i
Bremner JD, Vermetten E, Mazure CM (2000) Development and preliminary psychometric properties of an instrument for the measurement of childhood trauma: the Early Trauma Inventory. Depress Anxiety 12(1):1–12. https://doi.org/10.1002/1520-6394(2000)12:1%3c1::aid-da1%3e3.0.co;2-w
Callado LF, Meana JJ, Grijalba B, Pazos A, Sastre M, Garcia-Sevilla JA (1998) Selective increase of alpha2A-adrenoceptor agonist binding sites in brains of depressed suicide victims. J Neurochem 70(3):1114–1123
Caseras X, Garner M, Bradley BP, Mogg K (2007) Biases in visual orienting to negative and positive scenes in dysphoria: an eye movement study. J Abnorm Psychol 116(3):491–497. https://doi.org/10.1037/0021-843x.116.3.491
Chamberlain SR, Robbins TW (2013) Noradrenergic modulation of cognition: therapeutic implications. J Psychopharmacol 27(8):694–718. https://doi.org/10.1177/0269881113480988
Chapman A, Devue C, Grimshaw GM (2019) Fleeting reliability in the dot-probe task. Psychol Res 83(2):308–320. https://doi.org/10.1007/s00426-017-0947-6
Cottingham C, Wang Q (2012) alpha2 adrenergic receptor dysregulation in depressive disorders: implications for the neurobiology of depression and antidepressant therapy. Neurosci Biobehav Rev 36(10):2214–2225. https://doi.org/10.1016/j.neubiorev.2012.07.011
de Punder K, Entringer S, Heim C, Deuter CE, Otte C, Wingenfeld K, Kuehl LK (2018) Inflammatory measures in depressed patients with and without a history of adverse childhood experiences. Front Psychiatry 9:610. https://doi.org/10.3389/fpsyt.2018.00610
Deuter CE, Wingenfeld K, Otte C, Bustami J, Kaczmarczyk M, Kuehl LK (2020) Noradrenergic system and cognitive flexibility: disentangling the effects of depression and childhood trauma. J Psychiatr Res 125:136–143. https://doi.org/10.1016/j.jpsychires.2020.03.017
Ebner NC, Riediger M, Lindenberger U (2010) FACES–a database of facial expressions in young, middle-aged, and older women and men: development and validation. Behav Res Methods 42(1):351–362. https://doi.org/10.3758/brm.42.1.351
Ehlers MR, Todd RM (2017) Genesis and maintenance of attentional biases: the role of the locus coeruleus-noradrenaline system. Neural Plast 2017:6817349. https://doi.org/10.1155/2017/6817349
Eizenman M, Yu LH, Grupp L, Eizenman E, Ellenbogen M, Gemar M, Levitan RD (2003) A naturalistic visual scanning approach to assess selective attention in major depressive disorder. Psychiatry Res 118(2):117–128. https://doi.org/10.1016/s0165-1781(03)00068-4
England-Mason G, Khoury J, Atkinson L, Hall GB, Gonzalez A (2018) Attentional avoidance of emotional stimuli in postpartum women with childhood history of maltreatment and difficulties with emotion regulation. Emotion 18(3):424–438. https://doi.org/10.1037/emo0000372
Eysenck MW, Fajkowska M (2018) Anxiety and depression: toward overlapping and distinctive features. Cogn Emot 32(7):1391–1400. https://doi.org/10.1080/02699931.2017.1330255
Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, . . . Whiteford HA (2013). Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med 10(11), e1001547. https://doi.org/10.1371/journal.pmed.1001547
Flugge G, van Kampen M, Meyer H, Fuchs E (2003) Alpha2A and alpha2C-adrenoceptor regulation in the brain: alpha2A changes persist after chronic stress. Eur J Neurosci 17(5):917–928
Gaddy MA, Ingram RE (2014) A meta-analytic review of mood-congruent implicit memory in depressed mood. Clin Psychol Rev 34(5):402–416. https://doi.org/10.1016/j.cpr.2014.06.001
Garcia-Sevilla JA, Escriba PV, Ozaita A, La Harpe R, Walzer C, Eytan A, Guimon J (1999) Up-regulation of immunolabeled alpha2A-adrenoceptors, Gi coupling proteins, and regulatory receptor kinases in the prefrontal cortex of depressed suicides. J Neurochem 72(1):282–291
Giustino TF, Maren S (2018) Noradrenergic modulation of fear conditioning and extinction. Front Behav Neurosci 12:43. https://doi.org/10.3389/fnbeh.2018.00043
Goddard AW, Ball SG, Martinez J, Robinson MJ, Yang CR, Russell JM, Shekhar A (2010) Current perspectives of the roles of the central norepinephrine system in anxiety and depression. Depress Anxiety 27(4):339–350. https://doi.org/10.1002/da.20642
Gomez RG, Fleming SH, Keller J, Flores B, Kenna H, DeBattista C, . . . Schatzberg AF (2006) The neuropsychological profile of psychotic major depression and its relation to cortisol. Biol Psychiatry, 60(5), 472-478. https://doi.org/10.1016/j.biopsych.2005.11.010
Gotlib IH, Krasnoperova E, Yue DN, Joormann J (2004) Attentional biases for negative interpersonal stimuli in clinical depression. J Abnorm Psychol 113(1):121–135. https://doi.org/10.1037/0021-843x.113.1.121
Günther V, Dannlowski U, Kersting A, Suslow T (2015) Associations between childhood maltreatment and emotion processing biases in major depression: results from a dot-probe task. BMC Psychiatry 15:123. https://doi.org/10.1186/s12888-015-0501-2
Harmer CJ, Hill SA, Taylor MJ, Cowen PJ, Goodwin GM (2003) Toward a neuropsychological theory of antidepressant drug action: increase in positive emotional bias after potentiation of norepinephrine activity. Am J Psychiatry 160(5):990–992. https://doi.org/10.1176/appi.ajp.160.5.990
Harmer CJ, O'Sullivan U, Favaron E, Massey-Chase R, Ayres R, Reinecke A, . . . Cowen PJ (2009) Effect of acute antidepressant administration on negative affective bias in depressed patients. Am J Psychiatry, 166(10), 1178-1184. https://doi.org/10.1176/appi.ajp.2009.09020149
Harmer CJ, Shelley NC, Cowen PJ, Goodwin GM (2004) Increased positive versus negative affective perception and memory in healthy volunteers following selective serotonin and norepinephrine reuptake inhibition. Am J Psychiatry 161(7):1256–1263
Hedges DW, Woon FL (2011) Early-Life Stress and Cognitive Outcome. Psychopharmacology (berl) 214(1):121–130. https://doi.org/10.1007/s00213-010-2090-6
Heim C, Nemeroff CB (2002) Neurobiology of early life stress: clinical studies. Semin Clin Neuropsychiatry 7(2):147–159
Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R, . . . Nemeroff CB (2000) Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA, 284(5), 592-597
Herzog S, D’Andrea W, DePierro J, Khedari V (2018) When stress becomes the new normal: Alterations in attention and autonomic reactivity in repeated traumatization. J Trauma Dissociation 19(3):362–381. https://doi.org/10.1080/15299732.2018.1441356
Hinkelmann K, Moritz S, Botzenhardt J, Riedesel K, Wiedemann K, Kellner M, Otte C (2009) Cognitive impairment in major depression: association with salivary cortisol. Biol Psychiatry 66(9):879–885. https://doi.org/10.1016/j.biopsych.2009.06.023
Hinkelmann K, Muhtz C, Dettenborn L, Agorastos A, Moritz S, Wingenfeld K, . . . Otte C (2013) Association between cortisol awakening response and memory function in major depression. Psychol Med, 43(11), 2255-2263. https://doi.org/10.1017/s0033291713000287
Joormann J, Gotlib IH (2007) Selective attention to emotional faces following recovery from depression. J Abnorm Psychol 116(1):80–85. https://doi.org/10.1037/0021-843x.116.1.80
Joormann J, Quinn ME (2014) Cognitive processes and emotion regulation in depression. Depress Anxiety 31(4):308–315. https://doi.org/10.1002/da.22264
Kircanski K, Gotlib IH (2015) Processing of emotional information in major depressive disorder: Toward a dimensional understanding. Emot Rev 7(3):256–264
Klein AM, de Voogd L, Wiers RW, Salemink E (2018) Biases in attention and interpretation in adolescents with varying levels of anxiety and depression. Cogn Emot 32(7):1478–1486. https://doi.org/10.1080/02699931.2017.1304359
Kuehl LK, Deuter CE, Hellmann-Regen J, Kaczmarczyk M, Otte C, Wingenfeld K (2019) Enhanced noradrenergic activity by yohimbine and differential fear conditioning in patients with major depression with and without adverse childhood experiences. Prog Neuropsychopharmacol Biol Psychiatry, 109751. https://doi.org/10.1016/j.pnpbp.2019.109751
Kuehl LK, Deuter CE, Hellmann-Regen J, Kaczmarczyk M, Otte C, Wingenfeld K (2020) Enhanced noradrenergic activity by yohimbine and differential fear conditioning in patients with major depression with and without adverse childhood experiences. Prog Neuropsychopharmacol Biol Psychiatry 96:109751. https://doi.org/10.1016/j.pnpbp.2019.109751
Kuras YI, McInnis CM, Thoma MV, Chen X, Hanlin L, Gianferante D, Rohleder N (2017) Increased alpha-amylase response to an acute psychosocial stress challenge in healthy adults with childhood adversity. Dev Psychobiol 59(1):91–98. https://doi.org/10.1002/dev.21470
Ladd CO, Owens MJ, Nemeroff CB (1996) Persistent changes in corticotropin-releasing factor neuronal systems induced by maternal deprivation. Endocrinology 137(4):1212–1218. https://doi.org/10.1210/endo.137.4.8625891
Laux L, Glanzmann P, Schaffner P, Spielberger CD (1981) Das State-Trait-Angstinventar (Testmappe mit Handanweisung, Fragebogen STAI-G Form X1 und Fragebogen STAI-G Form X2). Beltz, Weinheim, (Spielberger, C.D., Gorsuch, R.L. & Lushene, R.E. (1970) „State-Trait Anxiety Inventory, Manual for the State-Trait Anxiety Inventory“; PaloAlto, CA:Consulting Psychologist Press)
Lawson C, MacLeod C, Hammond G (2002) Interpretation revealed in the blink of an eye: depressive bias in the resolution of ambiguity. J Abnorm Psychol 111(2):321–328. https://doi.org/10.1037//0021-843x.111.2.321
Lee JS, Mathews A, Shergill S, Yiend J (2016) Magnitude of negative interpretation bias depends on severity of depression. Behav Res Ther 83:26–34. https://doi.org/10.1016/j.brat.2016.05.007
LeMoult J, Gotlib IH (2019) Depression: A cognitive perspective. Clin Psychol Rev 69:51–66. https://doi.org/10.1016/j.cpr.2018.06.008
Lorentz K, Gutschow B, Renner F (1999) Evaluation of a direct alpha-amylase assay using 2-chloro-4-nitrophenyl-alpha-D-maltotrioside. Clin Chem Lab Med 37(11–12):1053–1062. https://doi.org/10.1515/cclm.1999.154
Lovallo WR, Farag NH, Sorocco KH, Acheson A, Cohoon AJ, Vincent AS (2013) Early life adversity contributes to impaired cognition and impulsive behavior: studies from the Oklahoma Family Health Patterns Project. Alcohol Clin Exp Res 37(4):616–623. https://doi.org/10.1111/acer.12016
MacLeod C, Mathews A (1988) Anxiety and the allocation of attention to threat. Q J Exp Psychol A 40(4):653–670. https://doi.org/10.1080/14640748808402292
MacLeod C, Mathews A, Tata P (1986) Attentional bias in emotional disorders. J Abnorm Psychol 95(1):15–20. https://doi.org/10.1037//0021-843x.95.1.15
Mather M, Clewett D, Sakaki M, Harley CW (2016) Norepinephrine ignites local hotspots of neuronal excitation: how arousal amplifies selectivity in perception and memory. Behav Brain Sci 39:e200. https://doi.org/10.1017/s0140525x15000667
Mathews A, MacLeod C (2005) Cognitive vulnerability to emotional disorders. Annu Rev Clin Psychol 1:167–195. https://doi.org/10.1146/annurev.clinpsy.1.102803.143916
Meana JJ, Barturen F, Garcia-Sevilla JA (1992) Alpha 2-adrenoceptors in the brain of suicide victims: increased receptor density associated with major depression. Biol Psychiatry 31(5):471–490
Meaney MJ, O'Donnell D, Rowe W, Tannenbaum B, Steverman A, Walker M, . . . Lupien S (1995) Individual differences in hypothalamic-pituitary-adrenal activity in later life and hippocampal aging. Exp Gerontol, 30(3-4), 229-251
Montgomery SA, Asberg M (1979) A new depression scale designed to be sensitive to change. Br J Psychiatry 134:382–389
Murphy SE, Yiend J, Lester KJ, Cowen PJ, Harmer CJ (2009) Short-term serotonergic but not noradrenergic antidepressant administration reduces attentional vigilance to threat in healthy volunteers. Int J Neuropsychopharmacol 12(2):169–179. https://doi.org/10.1017/s1461145708009164
Nelson J, Klumparendt A, Doebler P, Ehring T (2017) Childhood maltreatment and characteristics of adult depression: meta-analysis. Br J Psychiatry 210(2):96–104. https://doi.org/10.1192/bjp.bp.115.180752
Nemeroff CB (2016) Paradise lost: the neurobiological and clinical consequences of child abuse and neglect. Neuron 89(5):892–909. https://doi.org/10.1016/j.neuron.2016.01.019
O’Carroll RE, Drysdale E, Cahill L, Shajahan P, Ebmeier KP (1999) Stimulation of the noradrenergic system enhances and blockade reduces memory for emotional material in man. Psychol Med 29(5):1083–1088
O'Hara R, Schroder CM, Mahadevan R, Schatzberg AF, Lindley S, Fox S, . . . Hallmayer JF (2007) Serotonin transporter polymorphism, memory and hippocampal volume in the elderly: association and interaction with cortisol. Mol Psychiatry 12(6), 544-555. https://doi.org/10.1038/sj.mp.4001978
Oliva M, Anikin A (2018) Pupil dilation reflects the time course of emotion recognition in human vocalizations. Sci Rep 8(1):4871. https://doi.org/10.1038/s41598-018-23265-x
Orchard F, Pass L, Reynolds S (2016) “It Was All My Fault”; Negative Interpretation Bias in Depressed Adolescents. J Abnorm Child Psychol 44(5):991–998. https://doi.org/10.1007/s10802-015-0092-x
Ordway GA, Schenk J, Stockmeier CA, May W, Klimek V (2003) Elevated agonist binding to alpha2-adrenoceptors in the locus coeruleus in major depression. Biol Psychiatry 53(4):315–323
Otte C, Gold SM, Penninx BW, Pariante CM, Etkin A, Fava M, . . . Schatzberg AF (2016) Major depressive disorder. Nat Rev Dis Primers 2 16065. https://doi.org/10.1038/nrdp.2016.65
Otte C, Neylan TC, Pole N, Metzler T, Best S, Henn-Haase C, . . . Marmar CR (2005) Association between childhood trauma and catecholamine response to psychological stress in police academy recruits. Biol Psychiatry, 57(1), 27-32. https://doi.org/10.1016/j.biopsych.2004.10.009
Pechtel P, Pizzagalli DA (2011) Effects of early life stress on cognitive and affective function: an integrated review of human literature. Psychopharmacology 214(1):55–70. https://doi.org/10.1007/s00213-010-2009-2
Peckham AD, McHugh RK, Otto MW (2010) A meta-analysis of the magnitude of biased attention in depression. Depress Anxiety 27(12):1135–1142
Peskind ER, Wingerson D, Murray S, Pascualy M, Dobie DJ, Le Corre P, . . . Raskind MA (1995) Effects of Alzheimer's disease and normal aging on cerebrospinal fluid norepinephrine responses to yohimbine and clonidine. Arch Gen Psychiatry, 52(9), 774-782
Pfaltz MC, Passardi S, Auschra B, Fares-Otero NE, Schnyder U, Peyk P (2019) Are you angry at me? Negative interpretations of neutral facial expressions are linked to child maltreatment but not to posttraumatic stress disorder. Eur J Psychotraumatol 10(1):1682929. https://doi.org/10.1080/20008198.2019.1682929
Plotsky PM, Meaney MJ (1993) Early, postnatal experience alters hypothalamic corticotropin-releasing factor (CRF) mRNA, median eminence CRF content and stress-induced release in adult rats. Brain Res Mol Brain Res 18(3):195–200
Power MJ, Dalgleish T, Claudio V, Tata P, Kentish J (2000) The directed forgetting task: application to emotionally valent material. J Affect Disord 57(1–3):147–157. https://doi.org/10.1016/s0165-0327(99)00084-1
Puls S, Rothermund K (2018) Attending to emotional expressions: no evidence for automatic capture in the dot-probe task. Cogn Emot 32(3):450–463. https://doi.org/10.1080/02699931.2017.1314932
Rivero G, Gabilondo AM, Garcia-Sevilla JA, La Harpe R, Callado LF, Meana JJ (2014) Increased alpha2- and beta1-adrenoceptor densities in postmortem brain of subjects with depression: differential effect of antidepressant treatment. J Affect Disord 167:343–350. https://doi.org/10.1016/j.jad.2014.06.016
Saarni SI, Suvisaari J, Sintonen H, Pirkola S, Koskinen S, Aromaa A, Lönnqvist J (2007) Impact of psychiatric disorders on health-related quality of life: general population survey. Br J Psychiatry 190:326–332. https://doi.org/10.1192/bjp.bp.106.025106
Sara SJ (2016) Locus coeruleus reports changes in environmental contingencies. Behav Brain Sci 39:e223. https://doi.org/10.1017/s0140525x15001946
Schlosser N, Wolf OT, Wingenfeld K (2011) Cognitive correlates of hypothalamic-pituitary-adrenal axis in major depression. Expert Rev Endocrinol Metab 6(1):109–126. https://doi.org/10.1586/eem.10.79
Schmukle SC (2005) Unreliability of the dot probe task. Eur J Pers 19(7):595–605. https://doi.org/10.1002/per.554
Schulz A, Deuter CE, Breden IH, Vögele C, Wingenfeld K, Otte C, Kuehl LK (2021) Noradrenergic activation induced by yohimbine decreases interoceptive accuracy in healthy individuals with childhood adversity. Dev Psychopathol, 1-12. https://doi.org/10.1017/s0954579420001613
Seifert J, Britz P (2007) Rqube (Version 1.00. 8.100). In: University of Trier Trier, Germany
Soeter M, Kindt M (2011) Noradrenergic enhancement of associative fear memory in humans. Neurobiol Learn Mem 96(2):263–271. https://doi.org/10.1016/j.nlm.2011.05.003
Soeter M, Kindt M (2012) Stimulation of the noradrenergic system during memory formation impairs extinction learning but not the disruption of reconsolidation. Neuropsychopharmacology 37(5):1204–1215. https://doi.org/10.1038/npp.2011.307
Staugaard SR (2009) Reliability of two versions of the dot-probe task using photographic faces. Psychol Sci Q 51(3):339–350. https://doi.org/10.1080/02699930903205698
Tanaka M, Yoshida M, Emoto H, Ishii H (2000) Noradrenaline systems in the hypothalamus, amygdala and locus coeruleus are involved in the provocation of anxiety: basic studies. Eur J Pharmacol 405(1–3):397–406. https://doi.org/10.1016/s0014-2999(00)00569-0
Tannert S, Rothermund K (2020) Attending to emotional faces in the flanker task: Probably much less automatic than previously assumed. Emotion 20(2):217–235. https://doi.org/10.1037/emo0000538
Taylor JL, John CH (2004) Attentional and memory bias in persecutory delusions and depression. Psychopathology 37(5):233–241. https://doi.org/10.1159/000080719
Tsumura H, Shimada H (2012) Acutely elevated cortisol in response to stressor is associated with attentional bias toward depression-related stimuli but is not associated with attentional function. Appl Psychophysiol Biofeedback 37(1):19–29
Vasa RA, Pine DS, Masten CL, Vythilingam M, Collin C, Charney DS, . . . Bruck M (2009) Effects of yohimbine and hydrocortisone on panic symptoms, autonomic responses, and attention to threat in healthy adults. Psychopharmacology (Berl), 204(3), 445-455
Victeur Q, Huguet P, Silvert L (2020) Attentional allocation to task-irrelevant fearful faces is not automatic: experimental evidence for the conditional hypothesis of emotional selection. Cogn Emot 34(2):288–301. https://doi.org/10.1080/02699931.2019.1622512
Voncken MJ, Bögels SM, Peeters F (2007) Specificity of interpretation and judgemental biases in social phobia versus depression. Psychol Psychother 80(Pt 3):443–453. https://doi.org/10.1348/147608306x161890
Vrijsen JN, Becker ES, Arias-Vásquez A, van Dijk MK, Speckens A, Oostrom I (2014) What is the contribution of different cognitive biases and stressful childhood events to the presence and number of previous depressive episodes? Psychiatry Res 217(3):134–142. https://doi.org/10.1016/j.psychres.2014.02.033
Vrijsen JN, Tendolkar I, Arias-Vásquez A, Franke B, Schene AH, Fernández G, van Oostrom I (2015) Interaction of the 5-HTTLPR and childhood trauma influences memory bias in healthy individuals. J Affect Disord 186:83–89. https://doi.org/10.1016/j.jad.2015.06.008
Watkins PC, Martin CK, Stern LD (2000) Unconscious memory bias in depression: perceptual and conceptual processes. J Abnorm Psychol 109(2):282–289
Watkins PC, Vache K, Verney SP, Muller S, Mathews A (1996) Unconscious mood-congruent memory bias in depression. J Abnorm Psychol 105(1):34–41. https://doi.org/10.1037//0021-843x.105.1.34
Wells TT, Vanderlind WM, Selby EA, Beevers CG (2014) Childhood abuse and vulnerability to depression: cognitive scars in otherwise healthy young adults. Cogn Emot 28(5):821–833. https://doi.org/10.1080/02699931.2013.864258
Williams JB, Kobak KA (2008) Development and reliability of a structured interview guide for the Montgomery Asberg Depression Rating Scale (SIGMA). Br J Psychiatry 192(1):52–58. https://doi.org/10.1192/bjp.bp.106.032532
Winer ES, Salem T (2016) Reward devaluation: dot-probe meta-analytic evidence of avoidance of positive information in depressed persons. Psychol Bull 142(1):18–78. https://doi.org/10.1037/bul0000022
Wingenfeld K, Kuffel A, Uhlmann C, Terfehr K, Schreiner J, Kuehl LK, . . . Spitzer C (2013) Effects of noradrenergic stimulation on memory in patients with major depressive disorder. Stress, 16(2), 191-201. https://doi.org/10.3109/10253890.2012.708951
Wingenfeld K, Schafer I, Terfehr K, Grabski H, Driessen M, Grabe H, . . . Spitzer C (2011) The reliable, valid and economic assessment of early traumatization: first psychometric characteristics of the German version of the Adverse Childhood Experiences Questionnaire (ACE). Psychother Psychosom Med Psychol, 61(1), e10-14. doi:https://doi.org/10.1055/s-0030-1263161
Wingenfeld K, Spitzer C, Mensebach C, Grabe H. J, Hill A., Gast U, . . . Driessen M (2010) The German version of the Childhood Trauma Questionnaire (CTQ): preliminary psychometric properties. Psychother Psychosom Med Psychol 60(11), 442-450. https://doi.org/10.1055/s-0030-1247564
Wittchen H-U, Zaudig M, Fydrich T (1997) Skid. Strukturiertes klinisches Interview für DSM-IV. Achse I und II. Handanweisung
Yang W, Zhang JX, Ding Z, Xiao L (2016) Attention bias modification treatment for adolescents with major depression: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 55(3):208-218.e202. https://doi.org/10.1016/j.jaac.2015.12.005
Yiend J (2010) The effects of emotion on attention: A review of attentional processing of emotional information. Cogn Emot 24(1):3–47. https://doi.org/10.1080/02699930903205698
Zhou Z, Cao S, Li H, Li Y (2015) Treatment with escitalopram improves the attentional bias toward negative facial expressions in patients with major depressive disorders. J Clin Neurosci 22(10):1609–1613. https://doi.org/10.1016/j.jocn.2015.03.036
Funding
Open Access funding enabled and organized by Projekt DEAL. Linn Kuehl, Katja Wingenfeld, and Christian Otte were supported by the grant “Effects of increased noradrenergic activity by yohimbine administration on learning and attention in patients with major depression disorder,” funded by the German Research Foundation (Deutsche Forschungsgemeinschaft/ DFG, project KU 3106/2-1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kuehl, L.K., Deuter, C.E., Nowacki, J. et al. Attentional bias in individuals with depression and adverse childhood experiences: influence of the noradrenergic system?. Psychopharmacology 238, 3519–3531 (2021). https://doi.org/10.1007/s00213-021-05969-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-021-05969-7