Abstract
Lithium (Li) represents a first choice mood stabilizer for bipolar disorder (BD). Despite extensive clinical use, questions regarding its mechanism of action and pathological mechanism of renal function impairment by Li remain open. The present study aimed to improve our knowledge in this area paying special attention to the relationship between the length of Li action, lipid peroxidation (LP), and Na+/K+-ATPase properties. The effects of therapeutic Li doses, administered daily to male Wistar rats for 1 (acute), 7 (short term) and 28 days (chronic), were studied. For this purpose, Na+/K+-ATPase activity measurements, [3H]ouabain binding and immunoblot analysis of α-Na+/K+-ATPase were performed. Li-induced LP was evaluated by determining the malondialdehyde concentration by HPLC. Sleep deprivation (SD) was used as an experimental approach to model the manic phase of BD. Results obtained from the kidney were compared to those obtained from erythrocytes and different brain regions in the same tested animals. Whereas treatment with therapeutic Li concentration did not bring any LP damage nor significant changes of Na+/K+-ATPase expression and [3H]ouabain binding in the kidney, it conferred strong protection against this type of damage in the forebrain cortex. Importantly, the observed changes in erythrocytes indicated changes in forebrain cortices. Thus, different resistance to SD-induced changes of LP and Na+/K+-ATPase was detected in the kidney, erythrocytes and the brain of Li-treated rats. Our study revealed the tissue-specific protective properties of Li against LP and Na+/K+-ATPase regulation.
Similar content being viewed by others
Introduction
Lithium (Li) is a first-line treatment for the prevention of recurrences of bipolar disorder (BD) (Vosahlikova and Svoboda 2016). Despite extensive clinical use, questions regarding its mechanism of action remain open. Li is not only used as a typical mood stabilizer for the treatment of BD but also as augmentation therapy for depression, and in contrast, antiepileptics, such as valproate or carbamazepine, can be effectively used for mood stabilization in BD (Baldessarini et al. 2019). The discrepancy between terminology and clinical effects, not only in case of mood stabilizers, results in a call to change the psychoactive drug nomenclature (Seifert and Schirmer 2020).
While clearly effective, Li has narrow therapeutic index - most patients need plasma levels between 0.6 and 1 mM for full clinical effect (Alda 2015), and levels above 1.5 mM are regarded as toxic (Young 2009). Even when correctly dosed, Li can cause side effects (Can et al. 2014).
One of the organs adversely affected by long-term Li therapy is the kidney (Kishore and Ecelbarger 2013). Li treatment often causes nephrogenic diabetes insipidus (NDI), a urinary concentrating defect, affecting approximately 20% of patients (Alsady et al. 2016; Behl et al. 2015). Although the renal side effects in patients with BD caused by chronic Li doses are well described, recent results obtained from animals suggest that low Li doses are useful in preventing kidney disease caused by nephrotoxic compounds, inflammation, or oxidative stress (Alsady et al. 2016). The optimal Li dose for treatment of kidney diseases in humans needs further exploration (Gong et al. 2016).
The mechanism of Li action in BD therapy remains only partially understood (Alda 2015; Vosahlikova and Svoboda 2016). Na+/K+-ATPase has been viewed as a critical factor in the pathogenesis of BD (el-Mallakh and Wyatt 1995), and growing body of evidence suggested the associations of BD with oxidative stress and lipid peroxidation (LP) (Zhang and Yao 2013). These two areas were also studied together because LP products, occurring in response to oxidative stress, can modify membrane proteins (Catalá 2009). Results indicated that Na+/K+-ATPase inhibition can lead to increased oxidative stress and a compromised antioxidant defence in the brain of rats (Riegel et al. 2010). It was also suggested that the Li-induced regulation of Na+/K+-ATPase activity may be a potential contributing factor for reducing oxidative stress in BD patients (Banerjee et al. 2012).
Li-related changes of Na+/K+-ATPase properties or oxidative stress parameters were also reported in rat kidney. It was suggested that the development of Li-induced NDI is associated with decreased mRNA levels of aquaporin-2 (AQP2) and Na+/K+-ATPase (Laursen et al. 2004). Recently, oxidative stress was identified as one of the mechanisms involved in the structural and functional alteration of the kidney after prolonged treatment with Li (Ossani et al. 2019).
The aim of our study was to better understand the effect of Li on the interplay between the Na+/K+-ATPase and LP in the kidney. Effects of therapeutic Li doses, administered daily to male Wistar rats for 1 (acute), 7 (short-term), and 28 days (chronic) were studied. For this purpose, Na+/K+-ATPase activity, [3H]ouabain binding, and α-Na+/K+-ATPase immunoblot assays were used. Li-induced LP was determined by measuring the malondialdehyde concentration by HPLC. We took advantage of using paradoxical sleep deprivation (SD) rat model as a useful insight into the pathophysiology of mania (Andrabi et al. 2019; Logan and McClung 2016), to analyse Li-induced changes. Above that, results obtained from rat kidney were compared to those obtained in rat brain of the same tested animals. Detailed analysis of different parts of the rat brain was performed in our previous study (Vosahlikova et al. 2020). In the absence of direct brain measures in clinical psychiatry, peripheral blood cells could be a useful proxy or a biomarker (Alda 2015; Can et al. 2014; Le-Niculescu et al. 2009; Le-Niculescu et al. 2013). For this reason, we determined above-mentioned characteristics also in blood erythrocytes.
Material and methods
Materials and chemicals
[3H]ouabain (30 Ci/mmol, NET211001MC) was purchased from Perkin Elmer (Waltham, MA, USA). Antibodies α-Na+/K+-ATPase (H-300: sc-28800), α-Na+/K+-ATPase (H-3: sc-48345), actin (I-19: sc-1616), β-actin (C4: sc-47778), and goat anti-rabbit IgG-HRP (sc-2004) were from Santa Cruz Biotechnology (Dallas, TX, USA). Other chemicals were commercially available reagent grade.
Treatment of rats with a clinically relevant concentration of lithium and sleep deprivation experiments
In this work, previously described experimental protocol for Li treatment and sleep deprivation (SD) was used (Fukumoto et al. 2001; Vosahlikova et al. 2020). Shortly, male Wistar rats (weight about 200 g, Animal Facility of the Institute of Physiology of the Czech Academy of Sciences) were fed control or Li diet (0.2% lithium carbonate; 2 g Li2CO3/kg, SSNIFF Spezialdiäten GmbH, Soest, Germany) for 1, 7, or 28 days, and then, on the same diet, exposed to 3-day SD induced by placing rats onto the small platforms surrounded by water (resulting groups of rats are presented in Table 1). The final number of rats in each experimental group was 9 (3 rats in 3 independent experiments).
All experiments were approved by Animal Care and Use Committee of the Institute of Physiology of the Czech Academy of Sciences in agreement with Animal Protection Law of the Czech Republic and European Communities Council directives 86/609/EEC.
Collection of kidney, blood, plasma and erythrocyte samples
Kidneys were removed from the animals, weighed, snap frozen in liquid nitrogen, and stored at − 80 °C. About 1 g of kidney tissue was cut into small pieces; diluted in STEM medium containing 250 mM sucrose, 20 mM Tris–HCl, 3 mM MgCl2, 1 mM EDTA, pH 7.6, fresh 1 mM PMSF and complete protease inhibitor cocktail; homogenized in Teflon glass homogenizer for 7 min at 1800 rpm (2 g w.w. per 10 ml); and centrifuged for 7 min at 1200×g to separate cell debris and nuclear fraction (remaining in the sediment) from post-nuclear supernatant fraction, PNS. Aliquots of PNS were snap frozen in liquid nitrogen and stored at − 80 °C. From each experimental group of animals, two independent PNS were made. Protein was determined by the Lowry method using bovine serum albumin as standard.
Blood was drawn directly into K3-EDTA-coated vacutainer tubes to prevent coagulation, and blood samples were immediately centrifuged at 500×g for 10 min at 4 °C. The plasma and buffy coat were removed by aspiration. The remaining erythrocytes were washed three times in saline solution. Erythrocyte membranes (ghosts) were isolated as described by Kassak et al. (2006). Obtained plasma and ghosts were rapidly frozen in liquid nitrogen and stored at − 80 °C until further use.
Determination of lithium in plasma by inductively coupled plasma mass spectrometry
Li plasma concentrations were analysed as published previously (Vosahlikova et al. 2020) using inductively coupled plasma mass spectrometry (ICP-MS).
[3H] ouabain binding
Na+/K+-ATPase content in kidney PNS was determined by [3H]ouabain-binding assay which was used in our previous study of Na+/K+-ATPase in rat brain (Vosahlikova et al. 2020) with SDS pre-treatment. PNS was pre-treated with SDS at a final concentration of 0.5 mg/ml for 30 min at room temperature. Then, PNS (0.5 mg) was incubated with saturating, 120 nM concentration of [3H]ouabain (30 Ci/mmol, NET211001MC, Perkin Elmer, Waltham, MA, USA) for 90 min at 30 °C in a total volume of 0.2 ml of 5 mM NaH2PO4, 5 mM MgCl2, 50 mM Tris-HCl, pH 7.6. Non-specific binding was determined in the presence of 100 μM unlabelled ouabain. Non-specific binding represented 50% of total binding when determined at 100 μM concentration of unlabelled ouabain.
Na+/K+-ATPase activity assay
The Na+/K+-ATPase activity was measured as the production of inorganic phosphate (Pi) as published previously (Vosahlikova et al. 2020) with SDS pre-treatment as mentioned above.
Determination of malondialdehyde in kidney PNS
The concentration of MDA in PNS fractions prepared from kidney samples was determined by HPLC using derivatization with 2,4-dinitrophenylhydrazine (DNPH) and MDA concentrations normalized to the total protein contents as described before (Vosahlikova et al. 2020; Vosahlikova et al. 2019; Vosahlikova et al. 2018).
SDS-PAGE and immunoblotting
The α-subunit of Na+/K+-ATPase was determined by SDS-PAGE and immunoblotting with monoclonal H3 (sc-4835) antibody from Santa Cruz. Monoclonal β-actin antibody (C4: sc-47778) was used as a loading control. The aliquots of PM (20 μg of protein per sample) were mixed 1:1 with 2-fold concentrated Laemmli buffer (SLB) and heated for 3 min at 95 °C. Standard (10% w/v acrylamide/0.26% w/v bis-acrylamide) SDS electrophoresis was carried out as described before (Ujcikova et al. 2014; Vosahlikova et al. 2020, 2019, 2017).
Statistical analysis
All data are presented as mean ± SEM. Li concentration in plasma was measured separately in each animal in triplicate. In all other measurements, data are obtained from the analysis of two independent preparations of PNS isolated from each group of experimental animals (Table 1). Statistical analysis was carried out by ANOVA (all results excluding immunoblots; lithium and sleep deprivation as variables; pairwise comparison was performed separately by Newman-Keuls test) or unpaired Student’s t test (only immunoblots; statistical analysis was based on two immunoblots). The differences were considered significant at p < 0.05. Statistical analysis of immunoblots was carried out by unpaired Student’s t test of two immunoblots carried out with each PNS sample. The four control (Li-untreated) and four Li-treated PNS samples were run in the same gel and compared on the same blot. The differences among respective groups of experimental animals were considered significant at p < 0.05.
Results
Neither lithium nor sleep deprivation affects lipid peroxidation in the kidney unlike in the brain and erythrocytes
The effect of Li treatment on LP proceeding in PNS fractions prepared from the kidney of rats treated with Li for 1, 7, and 28 days was performed by determination of MDA by HPLC. Results presented in Table 2 show that the acute (1 day), short-term (7 days), and chronic (28 days) Li treatment did not influence MDA production (C1-SD vs. Li1-SD, ns p > 0.05; C7-SD vs. Li7-SD, ns p > 0.05; C28-SD vs. Li28-SD, ns p > 0.05). SD of control animals had no effect on concentration of MDA (C1-SD vs. C1+SD, ns p > 0.05; C7-SD vs. C7+SD, ns p > 0.05; C28-SD vs. C28+SD, ns p > 0.05), and the same situation occurred when compared C+SD and Li+SD groups (C1+SD vs. Li1+SD, ns p > 0.05; C7+SD vs. Li7+SD, ns p > 0.05; C28+SD vs. Li28+SD, ns p > 0.05).
Different results were obtained from MDA determinations in rat brain when compared with the kidney. Detailed rat brain analysis was published previously (Vosahlikova et al. 2020). Results in Table 3 show the difference between rat brain parts (forebrain cortex FBC and hippocampus HIPP), erythrocytes, and kidney isolated from the same animals. The sensitive tissues to Li treatment and SD in terms of LP changes were FBC, HIPP, and erythrocytes. On the other hand, MDA content in the kidney was not affected by Li treatment nor SD.
One day Li treatment of rats had no effect on MDA content in erythrocyte ghosts (Table 4; C1-SD vs. Li1-SD, ns p > 0.05). Long-term (7 and 28 days) treatment resulted in a decrease of MDA (C7-SD vs. Li7-SD, **p ˂ 0.01; C28-SD vs. Li28-SD, *p ˂ 0.05). SD, as in case of the brain, resulted in significant MDA increase in all control groups (C1-SD vs. C1+SD, ***p ˂ 0.001; C7-SD vs. C7+SD, ***p ˂ 0.001; C28-SD vs. C28+SD, **p ˂ 0.01). Increased MDA level due to SD was reversed after Li treatment in all groups (C1+SD vs. Li1+SD, ***p ˂ 0.001; C7+SD vs. Li7+SD, ***p ˂ 0.001; C28+SD vs. Li28+SD, **p ˂ 0.01).
Regulation of Na+/K+-ATPase activity but no effect on Na+/K+-ATPase expression and [3H]ouabain binding in the kidney of Li-treated sleep-deprived rats
Unlike the insensitivity of MDA concentration, long-term (28 days) Li treatment of rats significantly increased Na+/K+-ATPase activity in kidney PNS (Table 5, C28-SD vs. Li28-SD, *p ˂ 0.05). Acute (1 day) and short-term (7 days) treatment had no effect (C1-SD vs. Li1-SD, ns p > 0.05; C7-SD vs. Li7-SD, ns p > 0.05). SD alone results in increased Na+/K+-ATPase activity in all control groups (Table 5, C1-SD vs. C1+SD, *p ˂ 0.05; C7-SD vs. C7+SD, *p ˂ 0.05; C28-SD vs. C28+SD, *p ˂ 0.05) as was also observed in FBC and HIPP (Table 3). Chronic Li treatment before SD protected Na+/K+-ATPase against its SD-induced activity increase (C28+SD vs. Li28+SD, ns p > 0.05). Acute and short-term Li treatment significantly decreased Na+/K+-ATPase activity when compared with corresponding controls (C1+SD vs. Li1+SD, *p ˂ 0.05; C7+SD vs. Li7+SD, *p ˂ 0.05). Na+/K+-ATPase activity is increased as a result of SD no matter of a tested tissue, but the ability to reverse activity back to the control level is higher in the rat brain when compared with kidney fraction (Table 3).
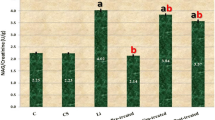
Different results from the measurement of Na+/K+-ATPase activity are obtained by [3H]ouabain-binding experiments (Table 6) and immunoblot analysis of Na+/K+-ATPase α-subunit (Fig. 1, Table 7) in kidney PNS. These two assays brought the same results: Li did not influence [3H]ouabain binding and Na+/K+-ATPase α-subunit (C-SD vs. Li-SD and C+SD vs. Li + SD groups) expression regardless of treatment length or SD (C1-SD vs. Li1-SD, ns p > 0.05; C7-SD vs. Li7-SD, ns p > 0.05; C28-SD vs. Li28-SD, ns p > 0.05; C1-SD vs. C1+SD, ns p > 0.05; C7-SD vs. C7+SD, ns p > 0.05; C28-SD vs. C28+SD, ns p > 0.05; C1+SD vs. Li1 + SD, ns p > 0.05; C7+SD vs. Li7+SD, ns p > 0.05; C28+SD vs. Li28+SD, ns p > 0.05).
Immunoblot analysis of α-Na+/K+-ATPase and β-actin in PNS isolated from rat kidney. Immunoblot assay was performed as described in Materials and methods. Statistical analysis is based on two immunoblots made from each PNS preparation (Supplementary Figure 1); the four controls and four Li-treated PNS samples were run in the same gel and compared on the same blot. Results were expressed as % of appropriate controls, 100%. Data were analysed using the unpaired Student’s t test. Statistical significance was marked as follows: ns p ˃ 0.05. Actin was used as a loading control
Based on these results, we could conclude that increased Na+/K+-ATPase activity due to SD occurred not only in the brain but also in the kidney (Table 3). Li administration to rats increased this enzyme activity after 28 days but did not influence α-subunit expression or [3H]ouabain binding (Fig. 1, Table 4). Li treatment before SD decreased activity in case of acute and short-term treatment and increased in case of long-term treatment, expression level, and [3H]ouabain binding remained the same.
Measurement of Na+/K+-ATPase activity was also performed in erythrocyte ghosts with the following results. One day Li treatment of rats had no effect on Na+/K+-ATPase activity (Table 7; C1-SD vs. Li1-SD, ns p > 0.05). Long-term (7 and 28 days) Li treatment resulted in a decrease of Na+/K+-ATPase activity (C7-SD vs. Li7-SD, *p ˂ 0.05; C28-SD vs. Li28-SD, *p ˂ 0.05). SD, as in case of brain and kidney, resulted in significant Na+/K+-ATPase activity increase in all control groups (C1-SD vs. C1+SD, *p ˂ 0.05; C7-SD vs. C7+SD, *p ˂ 0.05; C28-SD vs. C28+SD, **p ˂ 0.01). Increased Na+/K+-ATPase activity due to SD was reversed after Li treatment in groups with long-term exposure to Li (C1+SD vs. Li1+SD, ns p > 0.05; C7+SD vs. Li7+SD, **p ˂ 0.01; C28+SD vs. Li28+SD, **p ˂ 0.01).
Relevant lithium plasma concentrations
Our protocol for Li treatment of rats (Methods 2.1) was successfully used in previous studies (Fukumoto et al. 2001; Vosahlikova et al. 2020) and is a guarantee that 0.2% lithium carbonate diet results in a therapeutic concentration of Li in plasma of rats. Therefore, Li concentrations in plasma samples collected from all experimental groups of rats determined by ICP-MS are in desired therapeutic range 0.5–1.2 mmol/l (Table 2 in Vosahlikova et al. (2020)).
Discussion
Li therapy is accompanied by an increased diagnostic incidence of renal function impairment (Azab et al. 2015), but the underlying pathological mechanisms are not fully known (Ossani et al. 2019).
Some studies attributed the adverse effects of Li in the kidney or liver to oxidative stress (Kielczykowska et al. 2004; Nciri et al. 2012; Oktem et al. 2005). Protective properties of Li against LP were previously demonstrated in model cell lines (SH-SY5Y (Gawlik-Kotelnicka et al. 2016; Nciri et al. 2013) and Jurkat (Vosahlikova et al. 2019)), primary neuronal cell line prepared from the cerebral cortex of rats (Shao et al. 2005), in the FBC of rats treated with Li (Vosahlikova et al. 2020) and in the blood of healthy human subjects (Khairova et al. 2012). Protective effects of Li towards LP were also tested in red blood cells (Banerjee et al. 2012) and plasma (Machado-Vieira et al. 2007) of BD patients. On the other hand, the increased or unchanged LP after Li was observed in HEK293 cells (Vosahlikova et al. 2017), in the prefrontal cortex and HIPP isolated from rats (de Vasconcellos et al. 2006; Frey et al. 2006) and in human plasma under in vitro conditions (Gawlik-Kotelnicka et al. 2015).
Increased rat renal MDA levels after 1 month of Li treatment were published previously (Nciri et al. 2012; Oktem et al. 2005; Ossani et al. 2019). All of these studies used thiobarbituric acid (TBA) assay. Contradictory results showing no Li-induced LP (TBA assay) were obtained in mouse liver and kidney (Nciri et al. 2010) and rat plasma, liver, and kidney, whereas in the brain, evidence of a protective effect was observed (Kielczykowska et al. 2006).
Discrepancies in results of above-mentioned studies may be caused by the different length of Li treatment, type of Li salts used, the way of Li-administration, samples handling, type of MDA determination assay, different species/tissues/cell lines used, or final Li concentration in plasma. Our present study took into consideration all of above-mentioned differences in experimental procedures, and at the same time, it was methodologically built on our previous work (Vosahlikova et al. 2017, 2018, 2019, 2020). Results presented in this work showed no Li effect on MDA production in rat kidney. However, the protective effect of Li against LP was observed in erythrocytes.
Oxidative stress is one of the pathogenic mechanisms underlying kidney damage secondary to chronic Li administration (Ossani et al. 2019). The results of our study are inclined to believe that long-term administration of therapeutic Li does not damage lipids in the kidneys in terms of their peroxidation. Clinical application of LP products as biomarkers is a current topic, but further studies are needed as the accurate determination is complicated (Yoshida et al. 2013).
In contrast to the rat brain (Vosahlikova et al. 2020), SD and Li treatment did not affect [3H]ouabain binding and α-Na+/K+-ATPase content in rat kidney PNS tested in this work. Rats on Li diet had a marked decrease in the brain α-Na+/K+-ATPase levels as evidenced by [3H]ouabain binding. These results are consistent with previously published data of Guerri et al. (1981). The level of α1-mRNA Na+/K+-ATPase in the kidney cortex of Li-treated rats was unchanged compared with controls but altered in inner and outer medulla (Laursen et al. 2004).
Although Li did not affect [3H]binding and α-Na+/K+-ATPase content, the situation was different in the case of Na+/K+-ATPase activity. Enzyme activity was decreased by long-term Li treatment. Li also prevented SD-induced activity increase. Similar effects were observed in erythrocyte ghosts.
The effect of Li on microsomal Na+/K+-ATPase activity in different kidney regions was tested in the male rats by Gutman et al. (1973). Rats were injected intraperitoneally with 2 mEq/kg of LiCl for 14 days. These experimental conditions resulted in an increase of Na+/K+-ATPase activity in the medulla and papilla but not in the cortex of the kidney. The difference was ascribed to different physiological functions of respective kidney parts. The effect of acute (3 days) Li on renal morphology and Na+/K+-ATPase activity was tested in dogs (intraperitoneally 125 mg/kg/day) with the conclusion that Li did induce morphological changes in the distal nephron but had no effect on the cortical and medullary Na+/K+-ATPase activity (Easley 1982).
We can conclude that results of this study, when combined with those found in rat brain (Vosahlikova et al. 2020), revealed the tissue-specific protective properties of Li against LP and Na+/K+-ATPase regulation confirming the fact that Li effects may differ in different tissues. Whereas treatment of rats with therapeutic Li concentration for 1, 7, and 28 days did not bring any LP damage of kidney or significant changes of Na+/K+-ATPase expression and [3H]ouabain binding, it resulted in strong protection against this type of damage in the FBC.
Kidney and brain have a relatively high tissue density of Na+/K+-ATPase but a different abundance of n-3 and n-6 polyunsaturated fatty acids (PUFAs) in their membrane lipids (Wu et al. 2001). Physical properties of membrane lipid packing have the potential to influence Na+/K+-ATPase (Wu et al. 2001). LP is a process during which oxidants attack lipids containing carbon-carbon double bonds, especially in PUFAs (Ayala et al. 2014), and modifies the assembly of biological membranes (Catala 2014). The relative content of phospholipid-containing PUFAs is approximately 60% in the brain, whereas it is over 90% in other tissues (Choi et al. 2018).
Changes concomitantly observed in the brain and blood of REM sleep-deprived rat model, an animal model of mania-like behaviour (Andrabi et al. 2019), may represent useful proxies or candidate biomarkers (Le-Niculescu et al. 2009; Le-Niculescu et al. 2013), especially in the absence of direct brain measures in clinical psychiatry. Importantly, the determinations of LP and Na+/K+-ATPase parameters within this study clearly demonstrated that changes observed in blood erythrocytes indicated changes in forebrain cortices.
Relationships between of Na+/K+-ATPase and parameters describing the surrounding membrane lipids in context with Li treatment and mood disorders need further research; however, it is necessary to take into account a tissue specificity of Li effects and its complex regulatory networks.
References
Alda M (2015) Lithium in the treatment of bipolar disorder: pharmacology and pharmacogenetics. Mol Psychiatry 20:661–670. https://doi.org/10.1038/mp.2015.4
Alsady M, Baumgarten R, Deen PM, de Groot T (2016) Lithium in the kidney: friend and foe? J Am Soc Nephrol 27:1587–1595. https://doi.org/10.1681/asn.2015080907
Andrabi M et al (2019) Lithium acts to modulate abnormalities at behavioral, cellular, and molecular levels in sleep deprivation-induced mania-like behavior. Bipolar Disord. https://doi.org/10.1111/bdi.12838
Ayala A, Muñoz MF, Argüelles S (2014) Lipid peroxidation: production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxidative Med Cell Longev 2014:360438. https://doi.org/10.1155/2014/360438
Azab AN, Shnaider A, Osher Y, Wang D, Bersudsky Y, Belmaker RH (2015) Lithium nephrotoxicity. Int J Bipolar Disord 3:28. https://doi.org/10.1186/s40345-015-0028-y
Baldessarini RJ, Tondo L, Vazquez GH (2019) Pharmacological treatment of adult bipolar disorder. Mol Psychiatry 24:198–217. https://doi.org/10.1038/s41380-018-0044-2
Banerjee U, Dasgupta A, Rout JK, Singh OP (2012) Effects of lithium therapy on Na + -K + -ATPase activity and lipid peroxidation in bipolar disorder. Prog Neuro-Psychopharmacol Biol Psychiatry 37:56–61. https://doi.org/10.1016/j.pnpbp.2011.12.006
Behl T, Kotwani A, Kaur I, Goel H (2015) Mechanisms of prolonged lithium therapy-induced nephrogenic diabetes insipidus. Eur J Pharmacol 755:27–33. https://doi.org/10.1016/j.ejphar.2015.02.040
Can A, Schulze TG, Gould TD (2014) Molecular actions and clinical pharmacogenetics of lithium therapy. Pharmacol Biochem Behav 123:3–16. https://doi.org/10.1016/j.pbb.2014.02.004
Catalá A (2009) Lipid peroxidation of membrane phospholipids generates hydroxy-alkenals and oxidized phospholipids active in physiological and/or pathological conditions. Chem Phys Lipids 157:1–11. https://doi.org/10.1016/j.chemphyslip.2008.09.004
Catala A (2014) Lipid peroxidation modifies the assembly of biological membranes “The Lipid Whisker Model”. Front Physiol 5:520. https://doi.org/10.3389/fphys.2014.00520
Choi J, Yin T, Shinozaki K, Lampe JW, Stevens JF, Becker LB, Kim J (2018) Comprehensive analysis of phospholipids in the brain, heart, kidney, and liver: brain phospholipids are least enriched with polyunsaturated fatty acids. Mol Cell Biochem 442:187–201. https://doi.org/10.1007/s11010-017-3203-x
de Vasconcellos AP et al (2006) Chronic lithium treatment has antioxidant properties but does not prevent oxidative damage induced by chronic variate stress. Neurochem Res 31:1141–1151. https://doi.org/10.1007/s11064-006-9139-2
Easley JR (1982) The effect of lithium chloride on renal structure and sodium-potassium-adenosine triphosphatase activity in dogs. Vet Pathol 19:38–45. https://doi.org/10.1177/030098588201900107
el-Mallakh RS, Wyatt RJ (1995) The Na,K-ATPase hypothesis for bipolar illness. Biol Psychiatry 37:235–244. https://doi.org/10.1016/0006-3223(94)00201-D
Frey BN et al (2006) Effects of lithium and valproate on amphetamine-induced oxidative stress generation in an animal model of mania. J Psychiatry Neurosci 31:326–332
Fukumoto T, Morinobu S, Okamoto Y, Kagaya A, Yamawaki S (2001) Chronic lithium treatment increases the expression of brain-derived neurotrophic factor in the rat brain. Psychopharmacology 158:100–106. https://doi.org/10.1007/s002130100871
Gawlik-Kotelnicka O, Mielicki W, Rabe-Jabłońska J, Lazarek J, Strzelecki D (2016) Impact of lithium alone or in combination with haloperidol on oxidative stress parameters and cell viability in SH-SY5Y cell culture. Acta Neuropsychiatr 28:38–44. https://doi.org/10.1017/neu.2015.47
Gawlik-Kotelnicka O, Mielicki W, Rabe-Jabłońska J, Strzelecki D (2015) Impact of lithium alone or in combination with haloperidol on selected oxidative stress parameters in human plasma in vitro. Redox Rep. https://doi.org/10.1179/1351000215y.0000000030
Gong R, Wang P, Dworkin L (2016) What we need to know about the effect of lithium on the kidney. Am J Physiol Ren Physiol 311:F1168–F1171. https://doi.org/10.1152/ajprenal.00145.2016
Guerri C, Ribelles M, Grisolía S (1981) Effects of lithium, and lithium and alcohol administration on (Na + K)-ATPase. Biochem Pharmacol 30:25–30
Gutman Y, Hochman S, Wald H (1973) The differential effect of Li + on microsomal ATPase in cortex, medulla and papilla of the rat kidney. Biochim Biophys Acta 298:284–290
Kassak P, Sikurova L, Kvasnicka P, Bryszewska M (2006) The response of Na+/K+ -ATPase of human erythrocytes to green laser light treatment. Physiol Res 55:189–194
Khairova R et al (2012) Effects of lithium on oxidative stress parameters in healthy subjects. Mol Med Rep 5:680–682. https://doi.org/10.3892/mmr.2011.732
Kielczykowska M, Pasternak K, Musik I, Wroniska J (2004) The effect of lithium administration in a diet on the chosen parameters of the antioxidant barrier in rats. Ann Univ Mariae Curie Sklodowska Med 59:140–145
Kielczykowska M, Pasternak K, Musik J, Wronska-Tyra J, Hordyjewska A (2006) The influence of different doses of lithium administred in drinking water on lipid peroxidation and the activity of antioxidant enzymes in rats. Pol J Environ Stud 15:747–751
Kishore BK, Ecelbarger CM (2013) Lithium: a versatile tool for understanding renal physiology. Am J Physiol Ren Physiol 304:F1139–F1149. https://doi.org/10.1152/ajprenal.00718.2012
Laursen UH, Pihakaski-Maunsbach K, Kwon TH, Østergaard Jensen E, Nielsen S, Maunsbach AB (2004) Changes of rat kidney AQP2 and Na,K-ATPase mRNA expression in lithium-induced nephrogenic diabetes insipidus. Nephron Exp Nephrol 97:e1–e16. https://doi.org/10.1159/000077593
Le-Niculescu H et al (2009) Identifying blood biomarkers for mood disorders using convergent functional genomics. Mol Psychiatry 14:156–174. https://doi.org/10.1038/mp.2008.11
Le-Niculescu H et al (2013) Discovery and validation of blood biomarkers for suicidality. Mol Psychiatry 18:1249–1264. https://doi.org/10.1038/mp.2013.95
Logan RW, McClung CA (2016) Animal models of bipolar mania: The past, present and future. Neuroscience 321:163–188. https://doi.org/10.1016/j.neuroscience.2015.08.041
Machado-Vieira R et al (2007) Oxidative stress parameters in unmedicated and treated bipolar subjects during initial manic episode: a possible role for lithium antioxidant effects. Neurosci Lett 421:33–36. https://doi.org/10.1016/j.neulet.2007.05.016
Nciri R, Allagui MS, Bourogaa E, Saoudi M, Murat JC, Croute F, Elfeki A (2012) Lipid peroxidation, antioxidant activities and stress protein (HSP72/73, GRP94) expression in kidney and liver of rats under lithium treatment. J Physiol Biochem 68:11–18. https://doi.org/10.1007/s13105-011-0113-3
Nciri R, Allagui MS, Vincent C, Murat JC, Croute F, El Feki A (2010) Chronic lithium administration triggers an over-expression of GRP94 stress protein isoforms in mouse liver. Food Chem Toxicol 48:1638–1643. https://doi.org/10.1016/j.fct.2010.03.038
Nciri R, Desmoulin F, Allagui MS, Murat JC, Feki AE, Vincent C, Croute F (2013) Neuroprotective effects of chronic exposure of SH-SY5Y to low lithium concentration involve glycolysis stimulation, extracellular pyruvate accumulation and resistance to oxidative stress. Int J Neuropsychopharmacol 16:365–376. https://doi.org/10.1017/s1461145712000132
Oktem F, Ozguner F, Sulak O, Olgar S, Akturk O, Yilmaz HR, Altuntas I (2005) Lithium-induced renal toxicity in rats: protection by a novel antioxidant caffeic acid phenethyl ester. Mol Cell Biochem 277:109–115. https://doi.org/10.1007/s11010-005-5426-5
Ossani GP, Uceda AM, Acosta JM, Lago NR, Repetto MG, Martino DJ, Toblli JE (2019) Role of oxidative stress in lithium-induced nephropathy. Biol Trace Elem Res. https://doi.org/10.1007/s12011-018-1617-2
Riegel RE et al (2010) Intracerebroventricular ouabain administration induces oxidative stress in the rat brain. Int J Dev Neurosci 28:233–237. https://doi.org/10.1016/j.ijdevneu.2010.02.002
Seifert R, Schirmer B (2020) A simple mechanistic terminology of psychoactive drugs: a proposal. Naunyn Schmiedeberg's Arch Pharmacol 393:1331–1339. https://doi.org/10.1007/s00210-020-01918-x
Shao L, Young LT, Wang JF (2005) Chronic treatment with mood stabilizers lithium and valproate prevents excitotoxicity by inhibiting oxidative stress in rat cerebral cortical cells. Biol Psychiatry 58:879–884. https://doi.org/10.1016/j.biopsych.2005.04.052
Ujcikova H et al (2014) Opioid-Receptor (OR) Signaling cascades in rat cerebral cortex and model cell lines: the role of plasma membrane structure. Physiol Res 63:S165–S176
Vosahlikova M, Roubalova L, Ujcikova H, Hlouskova M, Musil S, Alda M, Svoboda P (2019) Na(+)/K(+)-ATPase level and products of lipid peroxidation in live cells treated with therapeutic lithium for different periods in time (1, 7, and 28 days); studies of Jurkat and HEK293 cells Naunyn Schmiedebergs. Arch Pharmacol 392:785–799. https://doi.org/10.1007/s00210-019-01631-4
Vosahlikova M, Svoboda P (2016) Lithium - therapeutic tool endowed with multiple beneficiary effects caused by multiple mechanisms. Acta Neurobiol Exp 76:1–19
Vosahlikova M, Ujcikova H, Chernyayskiy O, Brejchova J, Roubalova L, Alda M, Svoboda P (2017) Effect of therapeutic concentration of lithium on live HEK293 cells; increase of Na+/K + -ATPase, change of overall protein composition and alteration of surface layer of plasma membrane. Biochim Biophys Acta-Gen Subj 1861:1099–1112. https://doi.org/10.1016/j.bbagen.2017.02.011
Vosahlikova M, Ujcikova H, Hlouskova M, Musil S, Roubalova L, Alda M, Svoboda P (2018) Induction of oxidative stress by long-term treatment of live HEK293 cells with therapeutic concentration of lithium is associated with down-regulation of δ-opioid receptor amount and function. Biochem Pharmacol 154:452–463. https://doi.org/10.1016/j.bcp.2018.06.004
Vosahlikova M et al. (2020) Na(+)/K(+)-ATPase and lipid peroxidation in forebrain cortex and hippocampus of sleep-deprived rats treated with therapeutic lithium concentration for different periods of time. Prog Neuropsychopharmacol Biol Psychiatry 109953 doi:https://doi.org/10.1016/j.pnpbp.2020.109953
Wu BJ, Else PL, Storlien LH, Hulbert AJ (2001) Molecular activity of Na(+)/K(+)-ATPase from different sources is related to the packing of membrane lipids. J Exp Biol 204:4271–4280
Yoshida Y, Umeno A, Shichiri M (2013) Lipid peroxidation biomarkers for evaluating oxidative stress and assessing antioxidant capacity in vivo. J Clin Biochem Nutr 52:9–16. https://doi.org/10.3164/jcbn.12-112
Young W (2009) Review of lithium effects on brain and blood. Cell Transplant 18:951–975. https://doi.org/10.3727/096368909X471251
Zhang XY, Yao JK (2013) Oxidative stress and therapeutic implications in psychiatric disorders. Prog Neuro-Psychopharmacol Biol Psychiatry 46:197–199. https://doi.org/10.1016/j.pnpbp.2013.03.003
Funding
This work was supported by the Czech Science Foundation GA CR (GA17-07070S) and from the institutional project of the Institute of Physiology of the Czech Academy of Sciences (RVO:67985823).
Author information
Authors and Affiliations
Contributions
LR: experimental methodology, formal analysis, investigation, project administration. MV: conceptualization, experimental methodology, formal analysis, investigation, writing original draft, visualization, project administration. JS: experimental methodology, investigation. JK: formal analysis, investigation. MA: review and editing, supervision. PS: conceptualization, review and editing, supervision. All data were generated in-house and no paper mill was used.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent to participate
Not applicable
Consent to publish
Not applicable
Availability of data and materials
Data available within the article or its supplementary materials.
Ethical approval
All the animal handling procedures and experimental protocols were approved by the Animal Care and Use Committee of the Institute of Physiology of the Czech Academy of Sciences in agreement with Animal Protection Law of the Czech Republic and European Communities Council directives 86/609/EEC.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roubalová, L., Vošahlíková, M., Slaninová, J. et al. Tissue-specific protective properties of lithium: comparison of rat kidney, erythrocytes and brain. Naunyn-Schmiedeberg's Arch Pharmacol 394, 955–965 (2021). https://doi.org/10.1007/s00210-020-02036-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-020-02036-4