Abstract
Summary
We used conjoint analysis—a method that assesses complex decision making—to quantify patients’ choices when selecting an osteoporosis therapy. While 60% of people prioritized medication efficacy when deciding among treatments, the remaining 40% highly valued factors other than efficacy, suggesting the need for personalized shared decision-making tools.
Introduction
In this study, we aimed to examine patient decision-making surrounding osteoporosis medications using conjoint analysis.
Methods
We enrolled osteoporosis patients at an academic medical center to complete an online conjoint exercise which calculated each patient’s relative importance score of 6 osteoporosis medication attributes (higher = greater relative importance in decision-making). We used latent class analysis to identify distinct segments of patients with similar choice patterns and then used logistic regression to determine if demographics and osteoporosis disease features were associated with latent class assignment.
Results
Overall, 304 participants completed the survey. The rank order of medication attributes by importance score was the following: efficacy at preventing hip fractures (accounted for 31.0% of decision making), mode of administration (17.5%); risk of serious side effects (16.6%); dose frequency (13.9%); efficacy at preventing spine fractures (12.5%); risk of non-serious side effects (8.4%). We found that 60.9% of the cohort prioritized medication efficacy as their top factor when selecting among the therapies. Being a college graduate, having stronger beliefs on the necessity of using medications for osteoporosis, and never having used osteoporosis medicines were the only factors associated with prioritizing medication efficacy for fracture prevention over the other factors in the decision-making process.
Conclusions
While about 60% of patients prioritized efficacy when selecting an osteoporosis therapy, the remaining 40% valued other factors more highly. Furthermore, individual patient characteristics and clinical factors did not reliably predict patient decision making, suggesting that development and implementation of shared decision-making tools is warranted.
Similar content being viewed by others
Introduction
Understanding patient treatment preferences for osteoporosis, a condition characterized by decreased bone strength and increased fracture risk treatment, is critical as there are a growing number of treatment options [1, 2]. Moreover, the prevalence of osteoporosis is increasing; the age-adjusted prevalence of osteoporosis among US adults aged 50 years and older was estimated at 12.6% (19.6% in women, 4.4% in men) in 2017–2018 as compared to 9.4% in 2007–2008 [3]. The deleterious public health impact of osteoporosis and associated fragility fractures is also projected to increase in the coming years as the number of older Americans continues to expand. In addition, while many different treatments for osteoporosis exist to prevent further bone loss or even to rebuild bone and prevent fractures, there has been historically poor adherence to many of these medications [4,5,6,7], thereby supporting the need to select therapies that map to patients’ preferences and values.
Medical management options for osteoporosis differ in many ways including varying efficacy to prevent fractures, a range of potential side effects, variable cost, as well as different mode and frequency of administration. Determining which treatment is most likely to be beneficial to an individual patient and increasing the likelihood of adherence depends on how each unique person weighs the trade-offs of specific treatment attributes. Conjoint analysis—a form of tradeoff analysis that assesses how people make complex decisions—has been used previously to assess patient preferences in osteoporosis management [1, 2, 4, 8,9,10]. However, most of the conjoint analysis studies on osteoporosis treatments were conducted in Europe or were published over 10 years ago, prior to the availability of more recently approved treatments and contemporary information on safety concerns related to long term bisphosphonate use (e.g., osteonecrosis of the jaw). Thus, the differences in cultures and clinical medicine practices may reduce the generalizability of past patient preferences and shared decision-making methods. Moreover, with the ever-changing landscape of available medications, it is important to update our understanding on how patients approach the currently available options. To address these gaps, we used conjoint analysis to quantitatively examine patient decision-making when selecting a medical treatment for osteoporosis and better understand the tradeoffs they make during the decision-making process.
Methods
Study design
The study was approved by the Cedars-Sinai Institutional Review Board (STUDY1225). We performed a cross-sectional, online survey of patients with osteoporosis receiving care at Cedars-Sinai Medical Center (Los Angeles, CA), a community-based academic medical center serving a large catchment area in Southern California. The objective was to understand the tradeoffs patients make when deciding among osteoporosis treatment options using conjoint analysis.
Participant recruitment and study population
We used Deep6, an artificial intelligence cohort builder, to identify outpatients throughout the Cedars-Sinai medical network who had an ICD-10 diagnosis of osteoporosis and who had a visit with a Cedars-Sinai healthcare provider within the past 2 years. We excluded patients with osteoporosis who had a comorbid cancer/malignant neoplasm diagnosis (e.g., ICD-10: C00 to D49) and patients admitted as a hospital inpatient at the time of the Deep6 search.
Between July 2021 and September 2021, study invitation emails with survey links were sent to eligible patients. All respondents who accessed the survey were first presented with eligibility questions. Individuals were excluded if they did not self-report having been previously diagnosed with osteoporosis by a healthcare provider or if they had an active cancer diagnosis. Those not excluded were then prompted to review a study information page and provided consent before proceeding with the survey.
Survey Instrument
The Supplement shows the survey instrument, consisting of multiple choice-questions, conjoint analysis exercises, and open-ended responses. Prior to deploying the survey, we tested the instrument with 8 patients through online conferencing meetings and on the phone using a semi-structured interview and think-aloud method to ensure understandability and usability of the instrument [11].
Conjoint analysis exercises to assess patient preferences for osteoporosis treatment
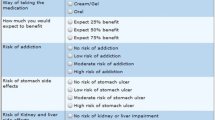
Conjoint analysis is a form of tradeoff analysis that elucidates the basis on which people make complex decisions [12,13,14]. We describe conjoint analysis in detail elsewhere [15], but in brief this approach is based on the idea that any product (e.g., a medicine) can be described by its attributes (e.g., mode of administration) and is valued based on the levels (e.g., IV infusion; oral; skin patch; subcutaneous injection) of these attributes. It is conducted with computer-based exercises where respondents evaluate competing profiles (e.g., of medicines) and select their preferred profile for achieving the stated objective (Fig. 1). The results for each individual are reported as preference scores called part-worth utilities. Part-worth utilities are calculated for each level within an attribute; summing part-worth utilities across the levels within each attribute equals 0. Levels with positive part-worth utilities are more preferred, while levels with negative part-worth utilities are less preferred. The choice-based conjoint (CBC) software also calculates importance scores for each attribute, which are derived by calculating the delta between the part-worth utilities for the most important and least important levels of each attribute. The importance score is between 0 and 100%, where a higher value denotes a more preferred attribute.
Example of an online conjoint exercise. Respondents evaluated side-by-side profiles of three hypothetical osteoporosis medicines at a time (each of which varied in the levels of six attributes) and were asked to choose their preferred therapy, if any. Respondents were presented with a random set of 8 comparisons
To quantify and rank preferences regarding the various osteoporosis treatment options, we employed CBC analysis. CBC presents a full profile of each treatment (i.e., all attributes). Participants were presented with three hypothetical osteoporosis medicines at a time, each of which varied the levels of each treatment attribute and asked to choose their preferred therapy (Fig. 1); respondents were ultimately presented with 8 comparisons. To avoid bias with any specific brands, the medicines were unbranded and presented as generic, hypothetical profiles.
When developing the conjoint analysis exercises, we followed best practices endorsed by the International Society for Pharmacoeconomic and Outcomes Research [12]. Selection of the attributes and levels for the conjoint analysis were informed by insights from the published literature [1, 8,9,10, 20,21,22,23,24,25,26,27,28,29,30,31,32,33]`, US Food and Drug Administration labels [34,35,36,37] for currently available osteoporosis medications, and input from a domain expert on the research team (J.R.C.). Table 1 presents the final attributes and levels that were tested in the survey.
Once the attributes and levels were finalized, they were inputted into a conjoint analysis platform (Lighthouse Studio 9.11.0, Sawtooth Software, North Orem, Utah). Participants were shown a random set of 8 side-by-side profiles (Fig. 1). Participants were instructed to “select which [medicine], if any, you would be most likely to choose for your osteoporosis medical treatment” and to “assume that medical insurance will cover each one and that you will not have any out-of-pocket costs.” The decision to instruct patients to ignore out-of-pocket costs was made in light of the consideration that out-of-pocket cost might be highly variable between patients, will change over time (e.g., as generic and biosimilar medications become available), and is often difficult to predict in advance. Prior to completing the conjoint exercises, respondents were provided information on the characteristics of osteoporosis medications (see Supplemental File).
Other considerations when selecting an osteoporosis medicine
After respondents completed the conjoint exercises, they were asked “Are there any other considerations that might affect your decision-making process regarding osteoporosis medications?” This allowed participants to describe any other attributes not presented in the CBC exercises that may influence their decision making. The content of each response was qualitatively analyzed, with sufficiently similar responses categorized as falling under a common factor that was not included as one of the six attributes in the conjoint exercises.
Covariates
The survey collected self-reported sociodemographic information, including age, sex, race/ethnicity, education, marital status, employment status, total household income, health insurance status, height, weight, tobacco use, and alcohol use. Participants were asked about their comorbidities, long-term steroid use, time first diagnosed with osteoporosis, medications currently and previously used to treat osteoporosis, bone fracture/fall history, and self-perceived fall risk. They were also asked about their beliefs about medications, self-reported health status, and beliefs about complementary and alternative medicine [33, 38,39,40,41].
Sample size calculation
Based on conjoint analysis sample size precedents and recommendations from the software provider, we aimed to recruit at least 300 adults with osteoporosis to complete the conjoint analysis survey [13]. So as to not markedly overshoot our sample size goal, we invited patients in batches of 100 at a time and closely monitored survey completions.
Statistical analyses of conjoint results
The software employed hierarchical Bayes regression to estimate individual-level importance scores and part-worth utilities [43, 44]. With respect to our primary aim for determining patients’ preferences and values when deciding among treatment options for osteoporosis, we performed descriptive analyses to calculate mean importance values and part-worth utilities for each test attribute and their corresponding levels, respectively. We then listed attributes in rank order from highest to lowest relative importance among the overall cohort. The software also used latent class analysis to identify distinct segments of respondents with similar choice patterns [45]. Given that the latent class analysis revealed only two distinct categories (see results below), we then performed a multivariable logistic regression analysis to determine if any patient demographics or osteoporosis disease features were associated with latent class assignment. Variables with a p < 0.20 in bivariate analyses were included in the regression model, and results were reported as adjusted odds ratios (aOR) with 95% confidence intervals (CI). All analyses were performed using R (version 4.1.2; R Core Team, 2021).
Results
Study population
Among 3500 eligible patients who were emailed the study invitation, 556 (15.9%) accessed the survey. We excluded those who started but did not complete the survey (n = 191) and who did not consent for the study (n = 61). Thus, 304 patients were included in the final dataset, and Table 2 presents their demographics. Most of the participants were over 60 years old, female, non-Hispanic White, and college graduates.
Table 3 shows the osteoporosis characteristics of the study population. Nearly 80% of patients were diagnosed with osteoporosis at least 2 years ago, and more than half were currently taking a medication to treat their condition. About 20% of participants had broken a bone commonly associated with osteoporosis (i.e., hip, spine or wrist) over the age of 50 years; prior research estimated that 40% of women and 13% of men with osteoporosis in the USA had at least one fracture in their lifetime [46, 47]. More than one-fourth had fallen and landed on the ground or fallen and hit an object like a table or chair in the last 6 months. The respondents also reported PROMIS global health scores that were average for the US general population [33].
Conjoint analysis to assess decision making on medical management of osteoporosis
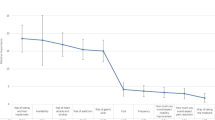
Across the entire sample, the rank order of medication attributes by importance score was the following (Fig. 2): efficacy at preventing hip fractures (31.0%, standard deviation [SD] 11.1%), mode of administration (17.5%, SD 8.8%); risk of serious side effects (16.6%, SD 6.5%); dose frequency (13.9%, SD 6.8%); efficacy at preventing spine fractures (12.5%, SD 4.8%); risk of non-serious side effects (8.4%, SD 3.8%). Part-worth utilities for mode of administration were the following: oral (37.2); skin patch (21.5); injected under skin (− 10.4); IV infusion (− 48.3).
Latent class analysis revealed that patients could be classified into one of two categories as related to decision-making: 185 (60.9%) respondents predominantly prioritized efficacy of the medicine at preventing hip or spine fractures in their decision making, over all other factors. Conversely, 119 (39.1%) people prioritized all factors equally or strongly valued other factors aside from efficacy. When stratifying the results by history of a broken hip, spine, or wrist over the age of 50, we found no statistically significant difference between groups with respect to latent class assignments (p = 0.916). Among 59 participants who broke their hip, spine, or wrist, 37 (62.7%) prioritized medication efficacy, whereas among the 225 participants without a prior fracture, 137 (60.9%) highly valued efficacy. We excluded 20 participants from the subgroup analysis because they were either below the age of 50 or did not remember whether they had a fracture.
Table 4 presents results from the regression on strongly prioritizing efficacy in fracture prevention. Most demographics and osteoporosis characteristics were not associated with decision making, save for a few exceptions. Namely, people who graduated from college (OR 2.14; 95% CI 1.11–4.13) and who had stronger beliefs on the necessity of using medications for osteoporosis (OR 1.14; 95% CI 1.05–1.23) were more likely to highly value efficacy of the medicine in preventing fractures when selecting a medicine. Conversely, those who never used osteoporosis medicines (OR 0.31; 95% CI 0.14-–0.66) were less likely to prioritize medication efficacy in their decision making.
Qualitative analyses of open-ended question
Overall, 105 analyzable responses were provided for the open-ended question on additional considerations for choosing osteoporosis medicines. No statistically significant differences in demographics or clinical characteristics were found between participants who did and did not answer the question (Supplementary Table 1, 2). Factors identified that may also influence the decision-making process included: potential interactions with other current medical conditions or medicines (n = 28, 26.7%); convenience of getting the medicine (e.g., requiring visits to infusion center or doctor’s office vs. at home; n = 18, 17.1%); physician’s recommendations (n = 17, 16.2%); costs (n = 10, 9.5%); availability of less invasive, preventive, or alternative medications (n = 8, 7.6%); real world evidence for the medication (n = 5, 4.8%); long-term efficacy (n = 5, 4.8%); patient’s age (n = 4, 3.8%); quality of life (n = 3, 2.9%); availability of medication (n = 2, 1.9%); family history (n = 2, 1.9%); protection against other fractures (n = 2, 1.9%); medical history (n = 2, 1.9%); how long the medication has been on the market (n = 2, 1.9%); comfort (n = 1, 1%); whether patients have access to new developments and research (n = 1, 1%); osteoporosis severity (n = 1, 1%); whether osteoporosis was caused by other diseases or medications (n = 1, 1%).
Discussion
This study assessed patient decision-making surrounding osteoporosis medications using conjoint analysis among 304 patients. We found that about 60% of osteoporosis patients prioritized medication efficacy while nearly 40% prioritized non-efficacy factors when deciding among treatments. Furthermore, most individual patient characteristics and clinical factors did not reliably predict what patients valued most when selecting among osteoporosis treatments, suggesting that in the future, developing and scaling shared decision-making tools is warranted.
Our findings are mostly consistent with previous research, almost all of which have identified effectiveness or efficacy of preventing fracture as the most prioritized attribute by the patients [1, 2, 4, 9]. For instance, a conjoint analysis by Silverman et al. in 2013 among 367 postmenopausal women found that patients from 4 racial/ethnic groups in the United States prioritized efficacy in their decision making [4]. Another study in 2007 assessing 999 American women aged 50 or above with or at risk of osteoporosis also found effectiveness as the most important determinant of preferences for osteoporosis medications [48]. Nevertheless, most of the previous studies only assessed women with osteoporosis, were conducted outside of the United States, or only performed a head-to-head comparison between two medication profiles, although yielded a similar result as ours [4, 9, 48,49,50]. In terms of other attributes, they were not ranked in the same order as in other studies mainly because each study used a slightly different attribute list or a different study sample. For example, cost is an attribute that was not included in our study but was considered as the third important attribute in the study by Silverman et al. [4].
In terms of patient demographics and clinical factors, we found that only education, osteoporosis medication use history, and perceived necessity of using osteoporosis medications were associated with patient preferences. These findings are contrary to previous studies revealing that—in addition to education—age, income, and fracture history were associated with patient decision making [4, 51]. On the whole, though, our results are consistent with other studies that found variations in medication decision making across different patient populations [51, 52]. Moreover, save for a few exceptions, most sociodemographic and osteoporosis-related factors were not associated with patients’ preferences. This points to the need for development and validation of novel decision aids to support patients and their providers when selecting an osteoporosis medicine.
Our study has several strengths. First, to our knowledge, this osteoporosis-focused conjoint analysis is the only one conducted in the US within the past decade and thus modeled the attributes of all currently available therapies. Second, we employed latent class analysis to identify (through probabilistic modelling and statistical inference) discrete groups of individuals that have similar choice patterns. This approach has grown in popularity across many disciplines of medicine due to its utility in addressing a number of methodological challenges confronted with traditional subgroup analysis, which would aim to determine differences in decision-making based on one or more measured characteristics [53, 54]. Finally, we attempted to determine sociodemographic and clinical factors associated with decision making, but found that most factors were not associated with decision making. This again emphasizes the need for decision aids to support patients and providers when choosing a therapy.
This study also has limitations. First, study participants were recruited from a single urban academic medical center; we opted for this approach so that we could examine respondents’ charts to confirm their osteoporosis diagnosis. Nonetheless, our results may not fully generalize to patients seeking care in community clinics or rural areas, and additional research examining patient preferences for osteoporosis therapies in other clinical settings is warranted. Second, our findings may not generalize to groups who are underrepresented in our study sample, as most of our respondents were female, non-Hispanic White, and had high educational attainment. Future studies assessing osteoporosis medication decision making should further diversify study cohorts (e.g., higher proportion of racial/ethnic minorities, younger individuals with osteoporosis resulting from long term medication use such as glucocorticoids). Third, given that we conducted our study only in the US, our findings may not be generalizable to other countries. Fourth, we employed an online survey and our results may not generalize to individuals who lack basic computing skills. However, in 2021, 96% and 75% of 50–64 and ≥ 65 year-old individuals, respectively, used the internet [55].
Fifth, we limited the conjoint analysis to six major attributes; there may have been other factors that affected people’s decision making such as medication costs, their prior osteoporosis medications, and previous discussion with physicians about the medication options. This was reflected in the responses to the open-ended questions where some respondents stated that their physician’s recommendation (16.2%) and cost (9.5%) would be important factors in their decision-making process. However, conjoint surveys can become unwieldy with too many attributes, and we chose to focus on six core attributes based on the existing literature [1, 8,9,10, 20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37], input from domain experts, and feedback from patients during our pilot testing. Relatedly, we opted to not include improvement in bone mineral density as an attribute; we decided to not include bone mineral density as it strongly correlates with fracture risk [56, 57] and the latter is more patient-centric. It is also possible that mechanism of action (e.g., anabolic vs. anti-resorptive) could be a factor that matters to some patients, although this did not emerge in our qualitative feedback from patients. Finally, 85% of our sample had current or past use of osteoporosis medication. Our results might differ when examining treatment preferences among patients who are treatment-naïve; this is worthy of further research.
In summary, while we found that about 60% of people with osteoporosis prioritized medication efficacy at preventing fracture when selecting among treatments, the remaining 40% placed greater value on non-efficacy factors. Furthermore, patient demographics and clinical factors minimally helped to classify what patient value most when selecting an osteoporosis treatment. Thus, to better align patients’ preferences with their medication choice, development of osteoporosis decision aids that can facilitate shared decision-making is warranted.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at Cedars-Sinai Medical Center.
References
Hiligsmann M, Dellaert BG, Dirksen CD, van der Weijden T, Goemaere S, Reginster JY, Watson V, Boonen A (2014) Patients’ preferences for osteoporosis drug treatment: a discrete-choice experiment. Arthritis Res Ther 16:R36
Hiligsmann M, Dellaert BG, Dirksen CD et al (2017) Patients’ preferences for anti-osteoporosis drug treatment: a cross-European discrete choice experiment. Rheumatology 56:1167–1176
Sarafrazi N, Wambogo EA, Shepherd JA (2021) Osteoporosis or Low Bone Mass in Older Adults: United States, 2017-2018. NCHS Data Brief (405):1–8
Silverman S, Calderon A, Kaw K, Childers T, Stafford B, Brynildsen W, Focil A, Koenig M, Gold D (2013) Patient weighting of osteoporosis medication attributes across racial and ethnic groups: a study of osteoporosis medication preferences using conjoint analysis. Osteoporos Int 24:2067–2077
Solomon DH, Avorn J, Katz JN, Finkelstein JS, Arnold M, Polinski JM, Brookhart MA (2005) Compliance with osteoporosis medications. Arch Intern Med 165:2414–2419
Klop C, Welsing P, Elders PJ, Overbeek J, Souverein PC, Burden AM, van Onzenoort HA, Leufkens H, Bijlsma J, de Vries F (2015) Long-term persistence with anti-osteoporosis drugs after fracture. Osteoporos Int 26:1831–1840
Netelenbos J, Geusens P, Ypma G, Buijs S (2011) Adherence and profile of non-persistence in patients treated for osteoporosis—a large-scale, long-term retrospective study in The Netherlands. Osteoporos Int 22:1537–1546
Darba J, Restovic G, Kaskens L, Balbona MA, Carbonell A, Cavero P, Jordana M, Prieto C, Molina A, Padro I (2011) Patient preferences for osteoporosis in Spain: a discrete choice experiment. Osteoporos Int 22:1947–1954
de Bekker-Grob EW, Essink-Bot ML, Meerding WJ, Pols HA, Koes BW, Steyerberg EW (2008) Patients’ preferences for osteoporosis drug treatment: a discrete choice experiment. Osteoporos Int 19:1029–1037
Fraenkel L, Gulanski B, Wittink D (2006) Patient treatment preferences for osteoporosis. Arthritis Rheum 55:729–735
Ericsson KA, Simon HA (1984) Protocol analysis: Verbal reports as data. the MIT Press
Bridges JF, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, Johnson FR, Mauskopf J (2011) Conjoint analysis applications in health–a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health 14:403–413
Orme BK (2010) Getting started with conjoint analysis: strategies for product design and pricing research. Research Publishers
Ryan M, Farrar S (2000) Using conjoint analysis to elicit preferences for health care. BMJ 320:1530–1533
Almario CV, Keller MS, Chen M, Lasch K, Ursos L, Shklovskaya J, Melmed GY, Spiegel BMR (2018) Optimizing Selection of biologics in inflammatory bowel disease: development of an online patient decision aid using conjoint analysis. Am J Gastroenterol 113:58–71
Luce RD, Tukey JW (1964) Simultaneous conjoint measurement: A new type of fundamental measurement. J Math Psychol 1:1–27
Anderson NH (1970) Functional measurement and psychophysical judgment. Psychol Rev 77:153
McFadden D (1973) Conditional logit analysis of qualitative choice behavior. Frontiers in Econometrics
Cattin P, Wittink DR (1982) Commercial use of conjoint analysis: a survey. J Mark 46:44–53
Black DM, Delmas PD, Eastell R et al (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356:1809–1822
Cummings SR, San Martin J, McClung MR et al (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361:756–765
Neer RM, Arnaud CD, Zanchetta JR et al (2001) Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344:1434–1441
Miller PD, Hattersley G, Riis BJ, Williams GC, Lau E, Russo LA, Alexandersen P, Zerbini CA, Hu M-y, Harris AGJJ (2016) Effect of abaloparatide vs placebo on new vertebral fractures in postmenopausal women with osteoporosis: a randomized clinical trial. JAMA 316:722–733
Saag KG, Petersen J, Brandi ML, Karaplis AC, Lorentzon M, Thomas T, Maddox J, Fan M, Meisner PD, Grauer A (2017) Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med 377:1417–1427
Cosman F, Crittenden DB, Adachi JD, Binkley N, Czerwinski E, Ferrari S, Hofbauer LC, Lau E, Lewiecki EM, Miyauchi A (2016) Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med 375:1532–1543
Black DM, Thompson DE, Bauer DC, Ensrud K, Musliner T, Hochberg MC, Nevitt MC, Suryawanshi S, Cummings SR, Group FR (2000) Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial. J Clin Endocrinol Metab 85:4118–4124
Martino S, Disch D, Dowsett SA, Keech CA, Mershon JL (2005) Safety assessment of raloxifene over eight years in a clinical trial setting. Curr Med Res Opin 21:1441–1452
Black DM, Kelly MP, Genant HK, Palermo L, Eastell R, Bucci-Rechtweg C, Cauley J, Leung PC, Boonen S, Santora A (2010) Bisphosphonates and fractures of the subtrochanteric or diaphyseal femur. N Engl J Med 362:1761–1771
Lamy O, Gonzalez-Rodriguez E, Stoll D, Hans D, Aubry-Rozier B (2017) Severe rebound-associated vertebral fractures after denosumab discontinuation: 9 clinical cases report. J Clin Endocrinol Metab 102:354–358
Anastasilakis AD, Polyzos SA, Makras P, Aubry-Rozier B, Kaouri S, Lamy O (2017) Clinical features of 24 patients with rebound-associated vertebral fractures after denosumab discontinuation: systematic review and additional cases. J Bone Miner Res 32:1291–1296
McClung M, Wagman RB, Miller P, Wang A, Lewiecki E (2017) Observations following discontinuation of long-term denosumab therapy. Osteoporos Int 28:1723–1732
Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL (2004) Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg 62:527–534
Hays RD, Schalet BD, Spritzer KL, Cella D (2017) Two-item PROMIS® global physical and mental health scales. J Patient Rep Outcomes 1:1–5
Merck & Co. I (2012) Fosamax (alendronate sodium) tablets label. U.S. Food and Drug Administration. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/021575s017lbl.pdf. Accessed December 23 2022
Corporation NP (2017) Reclast® (zoledronic acid) Injection label. U.S. Food and Drug Administration. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/021817s027lbl.pdf. Accessed December 23 2022
Inc. A (2018) Prolia® (denosumab) Injection, for subcutaneous use label. U.S. Food and Drug Administration. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/125320s186lbl.pdf. Accessed December 23 2022
Inc. A (2019) EVENITY™ (romosozumab-aqqg) injection, for subcutaneous use label. U.S. Food and Drug Administration. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/761062s000lbl.pdf. Accessed December 23 2022
Horne R, Weinman J, Hankins M (1999) The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health 14:1–24
Patterson C, Arthur H (2009) A complementary alternative medicine questionnaire for young adults. Integr Med Insights 4:IMI.S2281
Neame R, Hammond A (2005) Beliefs about medications: a questionnaire survey of people with rheumatoid arthritis. J Rheumatol 44:762–767
Hyland M, Lewith G, Westoby C (2003) Developing a measure of attitudes: the holistic complementary and alternative medicine questionnaire. Complement Ther Med 11:33–38
Orme BK (2006) Getting started with conjoint analysis: strategies for product design and pricing research
Cunningham CE, Deal K, Chen Y (2010) Adaptive choice-based conjoint analysis: a new patient-centered approach to the assessment of health service preferences. Patient 3:257–273
Lichtenstein GR, Waters HC, Kelly J, McDonald SS, Zanutto EL, Hendricks D, Rahman MI (2010) Assessing drug treatment preferences of patients with Crohn’s disease. Patient - Patient-Centered Outcomes Res 3:113–123
Software S (2019) The latent class: technical paper V4. Sawtooth Software. https://sawtoothsoftware.com/resources/technical-papers/latent-class-technical-paper. Accessed 23 Mar 2022
Melton LJ 3rd, Chrischilles EA, Cooper C, Lane AW, Riggs BL (1992) Perspective. How many women have osteoporosis? J Bone Miner Res 7:1005–1010
Office of the Surgeon General (US). Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville (MD): Office of the Surgeon General (US); 2004
Weiss TW, McHorney CA (2007) Osteoporosis medication profile preference: results from the PREFER-US study. Health Expect 10:211–223
de Bekker-Grob EW, Essink-Bot M-L, Meerding WJ, Koes BW, Steyerberg EW (2009) Preferences of GPs and patients for preventive osteoporosis drug treatment. Pharmacoeconomics 27:211–219
Duarte JW, Bolge SC, Sen SS (2007) An evaluation of patients’ preferences for osteoporosis medications and their attributes: the PREFER-International study. Clin Ther 29:488–503
Cornelissen D, Boonen A, Bours S, Evers S, Dirksen C, Hiligsmann M (2020) Understanding patients’ preferences for osteoporosis treatment: the impact of patients’ characteristics on subgroups and latent classes. Osteoporos Int 31:85–96
Hiligsmann M, Bours SP, Boonen A (2015) A Review of Patient Preferences for Osteoporosis Drug Treatment. Curr Rheumatol Rep 17:61
Horn JL (1965) A rationale and test for the number of factors in factor analysis. Psychometrika 30:179–185
Sinha P, Calfee CS, Delucchi KL (2021) Practitioner’s Guide to Latent Class Analysis: Methodological Considerations and Common Pitfalls. J Crit Care Med 49:e63
Pew Research Center (2021) Internet/Broadband Fact Sheet. https://www.pewresearch.org/internet/fact-sheet/internet-broadband/. Accessed September 8 2021
Black DM, Bauer DC, Vittinghoff E, Lui L-Y, Grauer A, Marin F, Khosla S, de Papp A, Mitlak B, Cauley JA (2020) Treatment-related changes in bone mineral density as a surrogate biomarker for fracture risk reduction: meta-regression analyses of individual patient data from multiple randomised controlled trials. Lancet Diabetes Endocrinol 8:672–682
Bouxsein ML, Eastell R, Lui LY et al (2019) Change in Bone Density and Reduction in Fracture Risk: A Meta-Regression of Published Trials. J Bone Miner Res 34:632–642
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium This study was supported by Amgen. The study sponsor did not have a role in the collection, analysis, or interpretation of data, or drafting of the manuscript. The Cedars-Sinai Center for Outcomes Research and Education (CS-CORE) is supported by The Marc and Sheri Rapaport Fund for Digital Health Sciences & Precision Health. Dr. Curtis receives salary support from NIAMS P30 AR072583.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Liu, X., Makaroff, K.E., Almario, C.V. et al. Determining patient preferences for the medical management of osteoporosis using conjoint analysis. Osteoporos Int 35, 153–164 (2024). https://doi.org/10.1007/s00198-023-06882-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06882-9