Abstract
Introduction
Rare bone diseases (RBDs) are a heterogenous group of disorders that are poorly understood and challenging to treat. This creates a plethora of unmet needs for people with RBDs as well as their families and care providers, including diagnostic delays, limited access to expert care, and a lack of specialized treatments. The RBD Summit, which took place across 2 days in November 2021, was a virtual meeting of 65 RBD experts from clinical, academic, and patient communities as well as the pharmaceutical industry. The first meeting of its kind, the RBD Summit aimed to facilitate dialog and information exchange between delegates to advance knowledge and awareness of RBDs and improve patient outcomes.
Methods
Key challenges were discussed, and actions for overcoming them were proposed, including how obstacles to diagnosis can be overcome by (a) improving awareness of RBDs, (b) the implementation of a person-centered care pathway, and (c) how to narrow the communication gap between patients and healthcare professionals.
Results
Agreed actions were categorized as short term and long term, and priorities determined.
Conclusion
In this position paper, we provide an overview of key discussions from the RBD Summit, summarize the subsequent action plan, and discuss the next steps in this continued collaboration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There are more than 771 rare bone diseases (RBDs) [1], accounting for approximately 5% of all rare diseases [2], yet most remain poorly understood and difficult to treat [2, 3]. The rarity of RBDs makes it likely that most healthcare professionals (HCPs), even those who specialize in bone health, may not see enough patients with RBD to build up critical expertise. This results in a lack of awareness and understanding of the complications and impact that living with a RBD has on patients [4]. In addition, advances in RBDs are limited by a shortfall in resources allocated to research, drug development, specialist centers, and educational programs [4], resulting in considerable challenges for patients and HCPs. Patients usually present first to their family physician, who may lack experience, training, or familiarity with diagnosing RBDs and thus fail to refer the patient to an expert team. These barriers can lead to potentially harmful diagnostic procedures with resultant delays in diagnosis. It is known that most patients only receive a correct diagnosis after a specialist referral [4] and people with rare diseases who have difficulty accessing disease-related information are two to five times more likely to receive a misdiagnosis [5]. Delayed care and misdiagnosis can have devastating effects on patients and their families, who may devote considerable time, energy, and money to their diagnostic journey [6]. Furthermore, undiagnosed patients are unlikely to receive appropriate monitoring, follow-up, and, in the limited number of RBDs with a medicinal product available, timely treatment. Instead, their condition may progress [6] and they can be subjected to inappropriate, or even harmful, medical procedures or treatments, which can have a devastating impact on their health and quality of life [4, 7, 8].
Globally, the extremely limited number of HCPs that are experts in a RBD, or group of RBDs, means that access to specialist care can pose tremendous challenges for patients. This varies significantly by country or region, with social and economic inequity in access to healthcare playing a major detrimental role. A dearth of expert physicians who specialize in RBDs may even exist in major cities and people living in such underserved areas are particularly affected as they are required to travel, if they are able, often long distances, to receive care and guidance, adding an extra burden to their time and finances [4].
Increasing awareness of RBDs and understanding the diversity among this heterogenous group of conditions are fundamental to highlighting the common challenges and formulating practical, feasible strategies to overcome them. To identify and address the most pressing unmet needs, it is imperative for all groups active in RBDs to work collaboratively on an aligned mission and vision. Thus, in 2021, a global steering committee was established that included expert HCPs (general practitioners, surgeons, oncologists, endocrinologists, nurses, and dentists) in the RBD field and scientists, alongside members of patient advocacy groups, medical and scientific societies, and the pharmaceutical industry. Through rigorous discussion, insight provision, and guidance, the steering committee created the Rare Bone Disease Summit, an annual convention for global multi-stakeholders active in RBD. The RBD Summit created a platform for open discussion, debate, and ideation to bring about change and advancement in the care of people living with RBD. In this position paper, we review the key discussions and decisions made at the summit and share considerations for the next steps on this journey.
Methodology
The meeting was devised by a steering committee of representatives from each stakeholder group from a range of geographical locations. The steering committee identified a list of organizations involved in RBDs, including patient advocacy groups, medical and scientific societies, medical education providers, and the pharmaceutical industry, and defined the roles and responsibilities of each party (Table 1). These organizations were then invited to send one representative to attend the meeting. Applications from the chosen representatives were then reviewed by the meeting organizers before being accepted. In total, 65 delegates attended the two 4-h virtual meetings comprised of short presentations and independently facilitated workshops.
Day 1 comprised three interactive workshops that ran in parallel, each facilitated by an independent moderator. The following three workshop topics were chosen by delegates through participation in a pre-meeting questionnaire: (a) overcoming obstacles to diagnosis by improving awareness of RBDs, (b) implementing person-centered care pathways, (c) narrowing the communication gap between patients and HCPs.
Delegates were assigned to a specific breakout group for participation in one of the workshops. Group allocation was determined ahead of day 1 and designed to ensure a mix of delegates from different backgrounds within each group, to promote rounded, non-biased discussions. The groups, led by members of the steering committee, discussed key unmet needs and challenges related to their topic(s) of interest and expertise in RBDs and identified actions that could be implemented to overcome them. Interactive whiteboards were used to allow delegates to individually answer discussion questions, ensuring participation from all and facilitating group discussion.
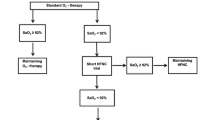
On day 2, the outcomes of each workshop were reported back to the full group, and further discussion took place on the importance of each identified gap, the feasibility of potential solutions, and whether any key factors had been missed. Four themes of outcomes were identified: (a) improving RBD awareness and education, (b) leveraging digital health, (c) removing silos and working collaboratively, and (d) establishing guidelines. Next, delegates agreed upon which outcomes could be actioned in the short-term and, using these outcomes, a vote was conducted to determine one key activity per workshop to move forward with.
Outcomes
Common challenges in RBDs
The delegates of the RBD Summit identified key unmet needs that they considered relevant, based on their expertise in a specific RBD or group of RBDs. A number of common themes arose from this initial deliberation. While the diagnostic delay in RBD has been reduced, it is still prevalent and was considered by many to be a major challenge for patients, their families, and care providers. It was discussed that the diagnostic delay is related to a lack of awareness of RBDs among HCPs, with many, including specialists, not recognizing concerning presenting features that should arouse suspicion of RBDs. Some of these features that were identified during the summit are shown in Fig. 1. Insufficient inclusion of materials related to RBDs in medical school curricula, limited HCP interest and time, a lack of perceived interest from the pharmaceutical industry, and time constraints on HCPs educational and patient-facing time were identified as critical factors that may contribute to poor understanding of RBDs by HCPs. In addition, an absence of appropriate assessment tools or guidelines may also impede a timely, accurate diagnosis.
Once diagnosed, patients should be on a pathway to receive specialized, targeted and personalized care, and dedicated support. However, many aspects of the patient care pathway were highlighted as challenges for patients and caregivers. Primary care physicians are not always aware of how to refer patients or who to refer them to. In addition, in underserved communities, a specialist referral can cause burdensome, costly journeys, or be hampered by language barriers. This lack of effective and timely referrals leaves patients stuck in a diagnostic limbo, during which they do not receive appropriate care nor support. Furthermore, even after patients have been referred and have accessed specialist care, further referrals might be needed for specific treatments. A lack of awareness of the importance of a multidisciplinary team (MDT), and the absence of RBD experts in many countries and regions, can also result in a barrier to care. Loss of MDT care is particularly prevalent during the transition from pediatric to adult and adult to geriatric care. These transitions were described, almost universally, as poor; many patients and caregivers bravely becoming their own care coordinators, while others fall behind into an unsupported path. The RBD Summit attendees identified a need for RBD referral networks, with information about how to refer patients and the location of specialized care centers (SCCs) and experts, as well as more centralized services and SCCs to be set up in countries with fewer specialized medical resources. In areas where there are few experts available, educational resources, checklists, and guidelines in local languages are needed to improve knowledge among local HCPs.
Patient-HCP communication may also be challenging for patients and care providers, and the RBD Summit delegates agreed that gaps in communication need to be overcome. Most patients may have difficulty understanding medical terminology, knowing which problems are most relevant/urgent, and expressing how they are feeling. Some have reported feeling like it is their responsibility to explain their diagnosis to physicians to ensure continuation of their own care, again highlighting the need for improved awareness of RBDs among the healthcare community. HCPs, on the other hand, may not be providing the patient with sufficiently detailed information about their case. The latter leads to a lack of patient understanding about their condition and how it may progress, removes patient autonomy, and impedes shared and informed decision-making, crucial to providing optimal care. Examples of the identified communication gaps are highlighted in Fig. 2. To help close the communication gap, patient focus groups, patient registries following FAIR principles (a set of guidelines which aim to improve Findability, Accessibility, Interoperability and Reuse of digital assets) [9] such as the European Registry for Rare Bone and Mineral Conditions [10], electronic surveys and burden of illness studies were suggested as methods for learning more about the patient experience. Resources for patients and HCPs could also be useful, including simple infographics to help explain a patient’s condition in local languages and digital platforms where patients and HCPs could ask questions and access test results.
Finally, cultural differences were flagged during the summit as a barrier to accessing care, from diagnosis to effective management. RBDs are stigmatized in some communities, mainly due to their effects on physical appearance, and families may hide their children from society and doctors for fear of being ostracized. The availability of patient advocacy groups and the quality/quantity of information they provide also vary across the world, increasing inequalities and leaving many patients feeling isolated or underinformed. In communities where patient advocacy groups are rare, HCPs may not be aware of them, or not be in contact with them, and therefore are unable to inform their patients of how to access them. Even if patient support and advocacy groups exist, funding and manpower constraints may limit their profile and minimize accessibility for patients.
Overcoming barriers
During the RBD Summit, four main categories of activities that could help in overcoming the barriers to optimal RBD care were identified: (a) improving awareness and education, (b) leveraging digital health, (c) removing silos and working collaboratively, and (d) establishing guidelines. Proposed actions were split into those that could be actioned in the short-term (2022/2023) and those that would be more long-term goals (2024 and beyond). Delegates voted for the highest priority actions within each category. The identified activities are described below and are summarized in Table 2.
Improving RBD awareness and education
Short-term actions:
-
Publish a position/consensus paper based on the outcomes of the summit in a leading musculoskeletal journal with a large, multinational, and multidisciplinary readership
-
Highlight RBDs in existing initiatives such as “Rare Disease Day”
-
Develop a communication plan for a potential Rare Bone Disease Month (similar to the awareness campaign that is centered around breast cancer every October [12])
-
Commitment from authors to utilize open access publishing for all papers originating from the summits and summit-related work, so that HCPs in all countries have access to relevant study results, as well as to produce plain language summaries that will be useful to the lay public
Longer-term actions:
-
Create a new platform to be a central and unified hub for people living with RBDs, their caregivers, or HCPs looking for information about RBDs. The platform will include information about all RBDs, lists of key experts and referral centers, and an organizational chart to help patients navigate all RBD patient organizations and societies that work in the realm of RBD. Search engine optimization and links on global medical sites already frequented both by HCPs and the public will ensure that the platform is readily accessible to the RBD community
-
Work collaboratively with patients, HCPs, and continuing/independent medical education providers to create easy to find, engaging, informative, and resonating content, including meaningful medical education programs that can be adapted to different languages and formats and shared globally across a wide range of platforms
-
Devise ways to encourage incorporation of educational materials on RBDs into medical school curricula
-
Increase awareness of RBDs by partnering with medical and scientific societies to ensure that RBDs are added as agenda items to meetings and conferences
-
Partner with relevant journals or medical and scientific societies to ensure that RBDs are included in publications likely to be read by relevant specialists and in abstracts presented at regional and international conferences
-
Fund travel grants for HCPs, researchers, and patient representatives from underserved regions to attend relevant conferences related to RBDs
-
Conduct search engine optimizations of educational platforms to ensure the distribution of existing information to patients and HCPs
-
Establish a social media presence in native languages to improve awareness in underserved communities
Leveraging digital health
Short-term actions:
-
Conduct a patient/caregiver survey to understand the patient experience and care pathway and identify telemedicine needs and possibilities
-
Create an online consultation guide for patients to help them navigate care and facilitate discussions with their HCPs
-
Organize a patient/patient advocacy interactive forum to gather insights into the patient experience, the care pathway, and the need (or lack thereof) for telemedicine
-
Collaborate with patient organizations to audit the existing information about patient experiences (requires multilingual teams) and classify it by age groups and priorities
Longer-term actions:
-
Map the status of existing virtual/hybrid clinics and telemedicine platforms for RBDs
-
Create a new telemedicine platform or modify existing platforms to make them more appropriate for RBDs and to increase access to specialist care centers
-
Contribute to help develop unified national policies to codify access to specialist care centers via telemedicine
-
Develop collaborative projects with professional teams to build artificial intelligence differential diagnostic tools for specific RBDs
Removing silos and working collaboratively
Short-term actions:
-
Conduct a landscape analysis to understand the collaborative gaps and silos within the RBD community, including those among HCPs, the pharmaceutical industry, and patient advocacy groups
-
Fund travel grants for academic experts to visit underserved/remote areas and invite (and fund) researchers, physicians, and expert patients from these areas to attend international conferences and leverage their communication skills to share the gained information nationally and locally
-
Organize scientific/medical events in underserved/remote areas or provide HCPs in these areas with access to online such events
Longer-term actions:
-
Build robust global and localized “clinicians collectives,” i.e., groups of clinicians who are educated about RBDs, well-connected, and who can then work collaboratively with patient organizations
-
Create knowledge-sharing initiatives (e.g., preceptorships and rotations through specialty clinics)
-
Develop referral networks or dedicated RBD departments/international virtual RBD clinics
-
Connect with other organizations, such as “Doctors Without Borders,” to help identify patients with RBDs, spread information, and share RBD resources on a global scale
Establishing diagnostic, care, and treatment guidelines
Short-term actions:
-
Collate examples of best practice guidelines
-
Publish a consensus paper on best practice guidelines for RBD management
-
Identify which RBDs have existing guidelines to understand which should be prioritized when developing new guidelines
-
Create educational materials (e.g., diagnostic guidelines, infographics, and checklists) to raise awareness of common concerning presenting features for RBDs and prompt referral when necessary
Longer-term actions:
-
Bring together multiple stakeholders and global experts to create detailed guidelines for HCPs to improve knowledge of HCPs at all levels and specialties
-
Create plain language summaries of existing guidelines to be disseminated through patient organizations
-
Translate existing guidelines into native languages with region-specific information about centers and experts to improve referral rates and care pathways throughout the world
-
Create diagnostic checklists or short appropriate care guidelines (such as those available for osteoporosis) [11] that will help to inform clinical care for specific RBDs and can serve as a starting point for more comprehensive guidelines
Summary
People living with RBDs often experience debilitating, painful symptoms, and clinical manifestations that may impact their appearance, mobility, and quality of life. The effects of RBDs extend into all aspects of life, including psychological, social, and financial [4].
The RBD Summit was a unique and important altruistic, and entirely voluntary collaboration between the clinical, academic and patient communities, and the pharmaceutical industry, with the aim to improve the care and quality of life of people living with RBDs. The global multi-stakeholder group discussed common unmet needs and barriers to improving care in RBDs. They then developed and prioritized short-term actions and longer-term strategies for overcoming these barriers, split into four categories: (a) improving awareness and education, (b) leveraging digital health, (c) removing silos and working collaboratively, and (d) establishing guidelines. The action plan developed by the summit in 2021 provides a necessary starting point for the improvement of the care of people living with RBDs.
Future directions
The RBD Summit was disease and drug agnostic, and future activities will continue to be so. Given that there are more than 700 RBDs, it would not be feasible to discuss each one separately in a single meeting. Hence, some of the more prevalent RBDs, those that have management protocols in place, and/or have clear therapies available, will be discussed in a holistic manner with common themes covered in future summits. To accomplish the strategies derived from the summit, continued collaboration is now essential. Activities such as collating best practice guidelines, producing an organogram of RBD patient organizations, and creating educational materials to increase knowledge of RBD concerning presenting features are being prioritized in the short term to raise awareness of RBDs and to maintain the current momentum generated by the summit. The next RBD Summit will include discussions around logistical aspects, such as funding, timelines, and roles and responsibilities that will be required to implement longer-term actions and encourage further stakeholder engagement. These will contribute towards the long-term goal of improving the lives of patients and emphasize the importance of continued collaboration of HCPs, societies, patients and patient organizations, pharmaceutical organizations, and independent medical education providers, in RBDs as well as other therapeutic areas.
References
Unger S, Ferreira CR, Geert R, Mortier H et al (2023) Nosology of genetic skeletal disorders: 2023 revision. Am J Med Genet 1–46. https://onlinelibrary.wiley.com/doi/epdf/10.1002/ajmg.a.63132
Tosi LL, Rajah EN, Stewart MH, Gillies AP, Hart TS, Lewiecki M (2020) The rare bone disease TeleECHO program: leveraging telehealth to improve rare bone disease. Care Curr Osteoporos Rep 18:344–349. https://doi.org/10.1007/s11914-020-00595-2
Sabir AH, Cole T (2019) The evolving therapeutic landscape of genetic skeletal disorders. Orphanet J Rare Dis 14:300. https://doi.org/10.1186/s13023-019-1222-2
The Economist Intelligence Unit. Leaving the darkness, seeing the light: a focus on people living with rare bone diseases. https://impact.economist.com/perspectives/sites/default/files/eiu_rare_bone_diseases.pdf. Accessed 1 December 2022
Dong D, Chung RY, Chan RH, Gong S, Xu RH (2020) Why is misdiagnosis more likely among some people with rare diseases than others? Insights from a population-based cross-sectional study in China. Orphanet J Rare Dis 15:307. https://doi.org/10.1186/s13023-020-01587-2
NORD Rare Insights. Barriers to rare disease diagnosis, care and treatment in the US: a 30-year comparative analysis. https://rarediseases.org/wp-content/uploads/2020/11/NRD-2088-Barriers-30-Yr-Survey-Report_FNL-2.pdf. Accessed 9 January 2023
Kitterman JA, Kantanie S, Rocke DM, Kaplan FS (2005) Iatrogenic harm caused by diagnostic errors in fibrodysplasia ossificans progressiva. Pediatrics 116:e654–e661. https://doi.org/10.1542/peds.2005-0469
Skrabl-Baumgartner A, Singer P, Greimel T, Gorkiewicz G, Hermann J (2019) Chronic non-bacterial osteomyelitis: a comparative study between children and adults. Pediatr Rheumatol Online J 17:49. https://doi.org/10.1186/s12969-019-0353-2
Wilkinson MD, Dumontier M, Aalbersberg IJ, Appleton G et al (2016) The FAIR Guiding Principles for scientific data management and stewardship. Scientific data 3. https://doi.org/10.1038/sdata.2016.18
European Registries for Rare Bone and Mineral Conditions (EuRR-Bone). https://eurr-bone.com. Accessed 9 January 2023
Agency for Care Effectiveness (ACE), ACE Clinical Guidances (ACGs). Osteoporosis – identification and management in primary care. https://www.ace-hta.gov.sg/healthcare-professionals/ace-clinical-guidances-(acgs)/details/osteoporosis-identification-and-management-in-primary-care. Accessed 9 January 2023
World Health Organization (WHO). Breast Cancer Awareness Month. https://www.who.int/europe/news-room/events/item/2022/10/01/default-calendar/breast-cancer-awareness-month. Accessed 13 March 2023
Acknowledgements
A full list of the steering committee members and organizations that were represented at the RBD Summit is provided in the Appendix.
Funding
The RBD Summit was sponsored by Ipsen. Medical writing support for this article was sponsored by Ipsen, Alexion, AstraZeneca Rare Disease, and Kyowa Kirin. However, the views and opinions of the authors are not those of the sponsors. Authors did not receive payment for their attendance at the RBD Summit or for their contribution to the development of the manuscript. Medical writing assistance was provided by Gabrielle Olley, Rock Unlimited. The authors retained final control of the content and editorial decisions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflicts of interest
MC has received honoraria for speaking and chairing engagements from Kyowa Kirin. TOC receives clinical trial research support through his institution from Ultragenyx for studies related to XLH and Osteogenesis Imperfecta. He has received consulting fees and honoraria from Alexion, Inozyme (Medical Advisory Board), Ipsen, Kyowa Kirin (Advisory Board), Ultragenyx, and Viridian. TOC serves in an unpaid capacity on the Medical Advisory Board for the FD/MAS Alliance, and the Scientific Advisory Boards of the XLH-Network, and Soft Bones (the US Hypophosphatasia Foundation). ECH receives clinical trial research support through his institution from Clementia Pharmaceuticals, an Ipsen Company, for studies related to FOP. He received prior clinical trials research support from Ultragenyx, Inc. for clinical trials research support through his institution for studies in osteogenesis imperfecta. ECH serves in an unpaid capacity on the Medical Advisory Board for the FD/MAS Alliance, on the Medical Registry Advisory Board of the International FOP Association, and on the International Clinical Council for FOP. AP is employee of and may own stock/options in Alexion, AstraZeneca Rare Disease. MS is an employee and shareholder of Ipsen. MD is a volunteer for the Rare Bone Disease Alliance Steering Committee. IA and JOS have no conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Manju Chandran and Ines Alves are co-first authors.
Objectives
• Highlight the barriers, challenges, and limited information available on diagnosis and management pathways for rare bone diseases (RBDs).
• Advance knowledge, awareness, and communication about RBDs.
• Bring attention to concerning presenting features in RBDs and how they can be communicated to the different stakeholders involved in the patient pathway to increase awareness, improve diagnosis and access to personalized care.
• Outline common patient experiences as well as communication gaps and challenges between the patient, family members and care providers, and healthcare professionals, and how they can be overcome.
• Increase awareness and education on challenges faced by people living with RBDs and drive actions proposed during the RBD Summit to help address unmet needs and gaps to improve their quality of life.
Appendix
Appendix
Steering committee members and the organization/rare disease group represented
Inês Alves: European Rare Bone Forum (ERBF).
Charlene Waldman: Rare Bone Disease Consultant.
Manju Chandran: Skeletal Rare Disorders Academy, International Osteoporosis Foundation, Asia Pacific Consortium on Osteoporosis.
Oliver Semler: The Osteogenesis Imperfecta Federation Europe (OIFE).
Michelle Davis: International Fibrodysplasia Ossificans Progressiva Association (IFOPA).
Federico Moscogiuri: International Federation of Musculoskeletal Research Societies (IFMRS).
Edward Hsiao: The International Clinical Council (ICC) on Fibrodysplasia Ossificans Progressiva (FOP).
Eric Rush: Hypophosphatasia (HPP) Expert.
Tom Carpenter: X-linked hypophosphatemia (XLH) Expert.
Sue Wood: Global Medical Affairs, Kyowa Kirin.
Anna Petryk: Global Medical Affairs, Alexion, AstraZeneca Rare Disease.
Jenny McCue: Global Patient Affairs, Ultragenyx.
Marwan Sleiman: Global Medical Affairs, Ipsen.
Organizations represented by meeting attendees
Advocacy Service for Rare and Intractable Diseases (ASRID), Alexion, American Society of Bone and Mineral Research (ASBMR), AstraZeneca Rare Disease, COR2ED, European Calcified Tissue Society (ECTS), European Paediatric Orthopaedic Society (EPOS), European Rare Bone Forum (ERBF), European Society of Endocrinology (ESE), European Reference Network on Rare Bone Disorders (ERN-BOND), Fibrous Dysplasia Foundation, International Conference on Children’s Bone Health (ICCBH), International Federation of Musculoskeletal Research Societies (IFMRS), International Fibrodysplasia Ossificans Progressiva Association (IFOPA), Ipsen, Instituto de Diagnóstico e Investigaciones Metabólicas, International (IDIM), International Clinical Council on Fibrodysplasia Ossificans Progressiva (ICC FOP), International Osteoporosis Foundation (IOF), International X-Linked Recessive (XLR) Alliance, Kyowa Kirin, Lymphangiomatosis and Gorham’s Disease Alliance, Osteogenesis Imperfecta Federation Europe (OIFE), Rare Bone Disease (RBD) Alliance, Soft Bones, The Jansen’s Foundation, Tin Soldiers, Ultragenyx, XLR Network.
RBD Summit sponsors
Ipsen.
Strategic partners
Kyowa Kirin, Alexion, AstraZeneca Rare Disease, Ultragenyx.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chandran, M., Alves, I., Carpenter, T. et al. Improving care pathways for people living with rare bone diseases (RBDs): outcomes from the first RBD Summit. Osteoporos Int 34, 1301–1310 (2023). https://doi.org/10.1007/s00198-023-06791-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06791-x