Abstract
Summary
Children with severe cerebral palsy are prone to low bone mineral density. No clear recommendation exists for an optimal use of standing frame to enhance bone health in this context. Used in real life, this study suggests for the first time that standing practice improved bone mineralization by limiting bone resorption.
Introduction
To compare the bone health of children with severe cerebral palsy who use a static standing frame in real life to that of children who do not.
Methods
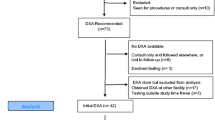
A total of 24 children with severe cerebral palsy GMFCS IV & V were included in the study and were divided into two groups: 13 were using a passive standing frame and 11 were not. We performed a single center retrospective cross-sectional study comparing the two groups using dual X-ray absorptiometry data and tests on biological samples, including bone remodeling factors.
Results
Total body (less head) bone mineral content was significantly higher in children who used a standing frame for an average of 30 min/day. This was confirmed in the lumbar spine. Although the total body bone mineral density (less head and proximal femur) densitometric data were not significantly higher, a positive trend favored the use of a standing frame in the children. Bone resorptive factors (CTX) were higher in the non-standing-frame group, whereas there was no difference among osteoformation factors. No difference in fracture history was found.
Conclusions
We show that non-ambulant children with cerebral palsy who use a static standing frame in real life have better bone health, with lower bone resorption, than children who do not. Further studies are needed to determine how standing practice could impact bone mineralization over time in real life and to explore more bone remodeling factors.


Similar content being viewed by others
References
Sadowska M, Sarecka-Hujar B, Kopyta I (2020) Cerebral palsy: current opinions on definition, epidemiology, risk factors, classification and treatment options. Neuropsychiatr Dis Treat 16:1505–1518
Mergler S, Evenhuis HM, Boot AM et al (2009) Epidemiology of low bone mineral density and fractures in children with severe cerebral palsy: a systematic review. Dev Med Child Neurol 51:773–778
Pin TW (2007) Effectiveness of static weight-bearing exercises in children with cerebral palsy: PediatrPhys Ther 19:62–73
Kim SJ, Kim S-N, Yang Y-N et al (2017) Effect of weight bearing exercise to improve bone mineral density in children with cerebral palsy: a meta-analysis. Bone 7:89–93
Damcott M, Blochlinger S, Foulds R (2013) Effects of passive versus dynamic loading interventions on bone health in children who are nonambulatory: Pediatr Phys Ther 25:248–255
Caulton JM (2004) A randomised controlled trial of standing programme on bone mineral density in non-ambulant children with cerebral palsy. Arch Dis Child 89:131–135
Chad KE, Bailey DA, McKay HA et al (1999) TThe effect of a weight-bearing physical activity program on bone mineral content and estimated volumetric density in children with spastic cerebral palsy. J Pediatr 135:115–117
Han EY, Choi JH, Kim S-H et al (2017) The effect of weight bearing on bone mineral density and bone growth in children with cerebral palsy: a randomized controlled preliminary trial. Medicine (Baltimore) 96:e5896
Gudjonsdottir et al. Effect of dynamic VS static prone stander on bone mineral density and behaviour in four children with cerebral palsy. Pediatr Phys Ther 14:38–46
Dalén Y, Sääf M, Ringertz H et al (2010) Effects of standing on bone density and hip dislocation in children with severe cerebral palsy. Adv Physiother 12:187–193
Palisano RJ, Cameron D, Rosenbaum PL et al (2006) Stability of the gross motor function classification system. Dev Med Child Neurol 48:424–428
Fardellone P, Sebert JL, Bouraya M, et al (1991) Evaluation of the calcium content of diet by frequential self-questionnaire. Rev Rhum Mal Osteoartic 58: 99–103
Internationnal Society For Clinical Densitometry (2019) Official positions pediatric: https://iscd.org/learn/official-positions/pediatric-positions/
Ctr M-P, Bma H, S N, et al (2019) Low bone mineral density in ambulatory persons with cerebral palsy? A systematic review. Disabil Rehabil; 41. Epub ahead of print October. https://doi.org/10.1080/09638288.2018.1470261.
Di Iorgi N, Maruca K, Patti G et al (2018) Update on bone density measurements and their interpretation in children and adolescents. Best Pract Res Clin Endocrinol Metab 32:477–498
Shrader MW, Wimberly L, Thompson R (2019) Hip surveillance in children with cerebral palsy. J Am Acad Orthop Surg 27:9
Ho S-T (2012) Review of fractures and low bone mass in children with cerebral palsy. J Orthop Trauma Rehabil 16:45–50
Kim W, Lee SJ, Yoon Y-K et al (2015) Adults with spastic cerebral palsy have lower bone mass than those with dyskinetic cerebral palsy. Bone 71:89–93
Shin Y-K, Yoon YK, Chung KB et al (2017) Patients with non-ambulatory cerebral palsy have higher sclerostin levels and lower bone mineral density than patients with ambulatory cerebral palsy. Bone 103:302–307
O’Brien CA, Plotkin LI, Galli C et al (2008) Control of bone mass and remodeling by PTH receptor signaling in osteocytes. PLoS ONE 3:e2942
Chen X, Macica CM, Ng KW et al (2005) Stretch-induced PTH-related protein gene expression in osteoblasts. J Bone Miner Res Off J Am Soc Bone Miner Res 20:1454–1461
Bellido T, Ali AA, Gubrij I et al (2005) Chronic elevation of parathyroid hormone in mice reduces expression of sclerostin by osteocytes: a novel mechanism for hormonal control of osteoblastogenesis. Endocrinology 146:4577–4583
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study has been declared to the National Commission for Freedom of Information Technology Act, number PI2021_843_0036.
Consent to participate
Oral consent was obtained from all children’s parents and an information sheet was sent to them.
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barbier, V., Goëb, V., Klein, C. et al. Effect of standing frames used in real life on bone remodeling in non-walking children with cerebral palsy. Osteoporos Int 33, 2019–2025 (2022). https://doi.org/10.1007/s00198-022-06436-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06436-5