Abstract
Summary
It has been proved that extracorporeal shock wave therapy (ESWT) could promote new bone formation. Therefore, we designed an experiment to test the efficiency of ESWT on BMD in postmenopausal osteoporotic patients. The results showed that ESWT could effectively improve the local bone mass of the treated bone area within a short duration.
Introduction
This study evaluated the short-term effectiveness of extracorporeal shock wave therapy (ESWT) on bone mineral density (BMD).
Methods
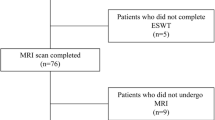
A total of 64 postmenopausal osteoporotic patients were recruited and randomized into 3 groups in 2015. Groups A (n = 20) and B (n = 21) patients received a single-session of low- or high-energy flux density (EFD) ESWT in the left hip, respectively, whereas group C (n = 23) patients served as controls without the ESWT treatment. All patients self-administered alendronate sodium tablets orally for a year. The BMD of the lumbar spine (L2-L4), femoral neck, great tuberosity, and total left hip was measured before ESWT treatment and at 3, 6, and 12 months using dual energy X-ray absorptiometry (DEXA).
Results
At 12 months, the lumbar spine, femoral neck, great tuberosity, and total left hip BMD in all patients had increased (p < 0.01). The increase in lumbar spine BMD in group A patients was higher than that in group B patients (p = 0.03); other between-group differences were not observed (p = 0.73, group A vs. C; p = 0.06, group B vs. C). The femoral neck, great tuberosity, and total left hip BMD increases in group B patients were higher than that in either group A or C (p < 0.01, group B vs. A; p < 0.01, group A vs. C).
Conclusion
This study showed that ESWT could efficiently improve the local BMD; relatively, the high dosage was effective.





Similar content being viewed by others
References
NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis. and Therapy (2001) Osteoporosis prevention, diagnosis, and therapy. JAMA 285(6): 785–795
Wark JD (1996) Osteoporotic fractures: background and prevention strategies. Maturitas 23(2):193–207
Kanis JA (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a who report. Who study group. Osteoporos Int 4(6):843:1–129
Giannoudis P, Tzioupis C, Almalki T, Buckley R (2007) Fracture healing in osteoporotic fractures: is it really different? Injury 38(1):S90–S99
Namkung-Matthai H, Appleyard R, Jansen J et al (2001) Osteoporosis influences the early period of fracture healing in a rat osteoporotic model. Bone 28(1):80–86
Kim J, Lee E, Kim S, Lee TJ (2016) Economic burden of osteoporotic fracture of the elderly in South Korea: a national survey. Value Health Reg Issues 9:36–41. doi:10.1016/j.vhri.2015.09.007
Lindsay R, Pack S, Li Z (2005) Longitudinal progression of fracture prevalence through a population of postmenopausal women with osteoporosis. Osteoporos Int 16(3):306–312. doi:10.1007/s00198-004-1691-5
Beck BR, Daly RM, Singh MA, Taaffe DR (2016) Exercise and Sports Science Australia (ESSA) position statement on exercise prescription for the prevention and management of osteoporosis. J Sci Med Sport. doi:10.1016/j.jsams.2016.10.001
Cosman F, De Beur SJ, Leboff MS et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25(10):2359–2381. doi:10.1007/s00198-014-2794-2
Khan M, Cheung AM, Khan AA (2017) Drug-related adverse events of osteoporosis therapy. Endocrinol Metab Clin N Am 46(1):181–192. doi:10.1016/j.ecl.2016.09.009
Romeo P, Lavanga V, Pagani D, Sansone V (2014) Extracorporeal shock wave therapy in musculoskeletal disorders: a review. Med Princ Pract 23(1):7–13. doi:10.1159/000355472
Ogden JA, Toth-Kischkat A, Schultheiss R (2001) Principles of shock wave therapy. Clin Orthop Relat Res 387:8–17
Link KA, Koenig JB, Silveira A, Plattner BL, Lillie BN (2013) Effect of unfocused extracorporeal shock wave therapy on growth factor gene expression in wounds and intact skin of horses. Am J Vet Res 74(2):324–332. doi:10.2460/ajvr.74.2.324
Rosso F, Bonasia DE, Marmotti A, Cottino U, Rossi R (2015) Mechanical stimulation (pulsed electromagnetic fields “PEMF” and extracorporeal shock wave therapy “ESWT”) and tendon regeneration: a possible alternative. Front Aging Neurosci 7:211. doi:10.3389/fnagi.2015.00211
Wang FS, Yang KD, Chen RF, Wang CJ, Sheen-Chen SM (2002) Extracorporeal shock wave promotes growth and differentiation of bone-marrow stromal cells towards osteoprogenitors associated with induction of TGF-beta1. J Bone Joint Surg Br 84(3):457–461
Mittermayr R, Antonic V, Hartinger J et al (2012) Extracorporeal shock wave therapy (ESWT) for wound healing: technology, mechanisms, and clinical efficacy. Wound Repair Regen 20(4):456–465. doi:10.1111/j.1524-475X.2012.00796.x
Kuo YR, Wang CT, Wang FS, Chiang YC, Wang CJ (2009) Extracorporeal shock-wave therapy enhanced wound healing via increasing topical blood perfusion and tissue regeneration in a rat model of STZ-induced diabetes. Wound Repair Regen 17(4):522–530. doi:10.1111/j.1524-475X.2009.00504.x
Stojadinovic A, Elster EA, Anam K et al (2008) Angiogenic response to extracorporeal shock wave treatment in murine skin isografts. Angiogenesis 11(4):369–380. doi:10.1007/s10456-008-9120-6
Zhao J, Xue Y, Yu J, Shi K, Xian C, Zhou X (2015) Advances in the research of mechanism of enhancement of wound healing with extracorporeal shock wave therapy. Zhonghua Shao Shang Za Zhi 31(4):315–317
Ikeda K, Tomita K, Takayama K (1999) Application of extracorporeal shock wave on bone: preliminary report. J Trauma 47(5):946–950
Van Der Jagt OP, Piscaer TM, Schaden W et al (2011) Unfocused extracorporeal shock waves induce anabolic effects in rat bone. J Bone Joint Surg Am 93(1):38–48. doi:10.2106/jbjs.i.01535
Wang CJ, Yang KD, Wang FS, Hsu CC, Chen HH (2004) Shock wave treatment shows dose-dependent enhancement of bone mass and bone strength after fracture of the femur. Bone 34(1):225–230. doi:10.1016/j.bone.2003.08.005
Mc DA, Frairia R, Romeo P et al (2016) Extracorporeal shockwaves as regenerative therapy in orthopedic traumatology: a narrative review from basic research to clinical practice. J Biol Regul Homeost Agents 30(2):323–332
Wang CJ (2012) Extracorporeal shockwave therapy in musculoskeletal disorders. J Orthop Surg Res 7:11. doi:10.1186/1749-799x-7-11
Zhang Q, Liu L, Sun W, Gao F, Cheng L, Li Z (2017) Extracorporeal shockwave therapy in osteonecrosis of femoral head: a systematic review of now available clinical evidences. Medicine (Baltimore) 96(4):e5897. doi:10.1097/md.0000000000005897
Alves EM, Angrisani AT, Santiago MB (2009) The use of extracorporeal shock waves in the treatment of osteonecrosis of the femoral head: a systematic review. Clin Rheumatol 28(11):1247–1251. doi:10.1007/s10067-009-1231-y
Kong FR, Liang YJ, Qin SG, Li JJ, Li XL (2010) Clinical application of extracorporeal shock wave to repair and reconstruct osseous tissue framework in the treatment of avascular necrosis of the femoral head (ANFH). Zhongguo Gu Shang 23(1):12–15
Gerdesmeyer L, Wagenpfeil S, Haake M et al (2003) Extracorporeal shock wave therapy for the treatment of chronic calcifying tendonitis of the rotator cuff: a randomized controlled trial. JAMA 290(19):2573–2580. doi:10.1001/jama.290.19.2573
Kanis JA, Mccloskey EV, Johansson H, Oden A, Melton LJ 3rd, Khaltaev N (2008) A reference standard for the description of osteoporosis. Bone 42(3):467–475. doi:10.1016/j.bone.2007.11.001
Cummings SR, Black DM, Nevitt MC et al (1993) Bone density at various sites for prediction of hip fractures. The Study of Osteoporotic Fractures Research Group. Lancet 341(8837):72–75
Ettinger MP (2003) Aging bone and osteoporosis: strategies for preventing fractures in the elderly. Arch Intern Med 163(18):2237–2246. doi:10.1001/archinte.163.18.2237
Gollwitzer H, Gloeck T, Roessner M et al (2013) Radial extracorporeal shock wave therapy (rESWT) induces new bone formation in vivo: results of an animal study in rabbits. Ultrasound Med Biol 39(1):126–133. doi:10.1016/j.ultrasmedbio.2012.08.026
Tam KF, Cheung WH, Lee KM, Qin L, Leung KS (2009) Shockwave exerts osteogenic effect on osteoporotic bone in an ovariectomized goat model. Ultrasound Med Biol 35(7):1109–1118. doi:10.1016/j.ultrasmedbio.2009.01.001
Chen XF, Huang HM, Li XL, Liu GJ, Zhang H (2015) Slightly focused high-energy shockwave therapy: a potential adjuvant treatment for osteoporotic fracture. Int J Clin Exp Med 8(4):5044–5054
Wang P, Liu C, Yang XT et al (2014) Effect of extracorporeal shock wave therapy on cartilage and subchondral bone remodeling in rabbits with ACLT-induced osteoarthritis. Sichuan Da Xue Xue Bao Yi Xue Ban 45(1):120–125
Wang L, Qin L, Lu HB et al (2008) Extracorporeal shock wave therapy in treatment of delayed bone-tendon healing. Am J Sports Med 36(2):340–347. doi:10.1177/0363546507307402
Peng YZ, Zheng K, Yang P et al (2015) Shock wave treatment enhances endothelial proliferation via autocrine vascular endothelial growth factor. Genet Mol Res 14(4):19203–19210. doi:10.4238/2015.December.29.30
Ma HZ, Zeng BF, Li XL, Chai YM (2008) Temporal and spatial expression of BMP-2 in sub-chondral bone of necrotic femoral heads in rabbits by use of extracorporeal shock waves. Acta Orthop 79(1):98–105. doi:10.1080/17453670710014833
Tischer T, Milz S, Weiler C et al (2008) Dose-dependent new bone formation by extracorporeal shock wave application on the intact femur of rabbits. Eur Surg Res 41(1):44–53. doi:10.1159/000128279
Delius M, Draenert K, Al Diek Y, Draenert Y (1995) Biological effects of shock waves: in vivo effect of high energy pulses on rabbit bone. Ultrasound Med Biol 21(9):1219–1225
Kaulesar Sukul DM, Johannes EJ, Pierik EG, Van Eijck GJ, Kristelijn MJ (1993) The effect of high energy shock waves focused on cortical bone: an in vitro study. J Surg Res 54(1):46–51
Tam KF, Cheung WH, Lee KM, Qin L, Leung KS (2005) Delayed stimulatory effect of low-intensity shockwaves on human periosteal cells. Clin Orthop Relat Res 438:260–265
Acknowledgments
We would like to thank all the patients who participated in this study. We thank our colleagues and all the staff members involved in this trial for their enormous efforts in collecting and ensuring the accuracy and completeness of all the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All patients provided written informed consent before participating in the prospective trial, and prior approval for this study was obtained from the Scientific Review Board of China-Japan Friendship Hospital.
Ethical approval
All procedures performed in this study involving human participants were in compliance with the Ethical Standards of the Institutional and/or National Research Committee and the 1964 Helsinki Declaration and its later amendments.
Funding
This study was supported by the Beijing Natural Science Foundation (7174346), the National Natural Science Foundation of China (81372013, 81672236), the Research Fund of China-Japan Friendship Hospital (2014-4-QN-29), and the China-Japan Friendship Hospital Youth Science and Technology Excellence Project (2014-QNYC-A-06).
Conflict of interest
None.
Additional information
Lijun Shi and Fuqiang Gao are joint first authors.
Rights and permissions
About this article
Cite this article
Shi, L., Gao, F., Sun, W. et al. Short-term effects of extracorporeal shock wave therapy on bone mineral density in postmenopausal osteoporotic patients. Osteoporos Int 28, 2945–2953 (2017). https://doi.org/10.1007/s00198-017-4136-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4136-7