Abstract
Summary
This study showed that about a half of the exercise-induced gain in dynamic balance and bone strength was maintained one year after cessation of the supervised high-intensity training of home-dwelling elderly women. However, to maintain exercise-induced gains in lower limb muscle force and physical functioning, continued training seems necessary.
Introduction
Maintenance of exercise-induced benefits in physical functioning and bone structure was assessed one year after cessation of 12-month randomized controlled exercise intervention.
Methods
Originally 149 healthy women 70–78 years of age participated in the 12-month exercise RCT and 120 (81%) of them completed the follow-up study. Self-rated physical functioning, dynamic balance, leg extensor force, and bone structure were assessed.
Results
During the intervention, exercise increased dynamic balance by 7% in the combination resistance and balance-jumping training group (COMB). At the follow-up, a 4% (95% CI: 1–8%) gain compared with the controls was still seen, while the exercise-induced isometric leg extension force and self-rated physical functioning benefits had disappeared. During the intervention, at least twice a week trained COMB subjects obtained a significant 2% benefit in tibial shaft bone strength index compared to the controls. A half of this benefit seemed to be maintained at the follow-up.
Conclusions
Exercise-induced benefits in dynamic balance and rigidity in the tibial shaft may partly be maintained one year after cessation of a supervised 12-month multi-component training in initially healthy elderly women. However, to maintain the achieved gains in muscle force and physical functioning, continued training seems necessary.
Similar content being viewed by others
Introduction
Falls and related fractures are a major and a worldwide healthcare problem causing functional decline and impaired quality of life in elderly people. On the other hand, physical limitations, such as impaired balance and mobility and decreased muscle strength of lower limbs predispose older adults to falls [1, 2]. Moreover, in conjunction with risk factors for falling, increased bone fragility attributable to osteopenia or osteoporosis is associated with low-energy fractures [3, 4].
Several randomized, controlled trials have found that exercise has beneficial effects on the risk factors of falls and fragility fractures of elderly people [5–10]. The participants in these studies have quite often been frail, with reduced physical function, low bone mass, and previous falls and fractures. However, in primary prevention it is important to start preventing functional impairments, bone loss and falls already among relatively healthy elderly individuals, since during the next few years many of these people will also be at risk for functional decline and fracture.
Intensity of effective exercise interventions, especially among the relatively healthy elderly persons, has often been rather high, requiring a lot of time, energy and motivation from participants. Thus, it is not very likely that many older people are able or willing to continue vigorous training on their own after cessation of supervised exercise intervention; therefore, it is important to understand the influence of reduced training on their functional ability and skeleton.
The effects of detraining on neuromuscular function and bone has been somewhat studied among different age groups including, older adults [11–15]. However, these results cannot be directly generalized to all elderly people due to large heterogeneity in the health status and functional ability in this age group. Thus, we cannot say, for example, if the residual bone benefits seen in exercised premenopausal middle-aged women could be seen among older women as well [13]. It is also unclear whether relatively healthy elderly women could partly maintain the exercise-induced benefits in risk factors for falls, as was seen in a study of at least mildly frail elderly women with low bone mass [15]. Additionally, the type and intensity of the exercise, as well as the length of training and detraining periods, are important. For instance, in the majority of the high-intensity training studies of healthy elderly adults, the training and detraining periods have lasted no more than a few months. Therefore, more studies are needed to describe the consequences of cessation of exercise interventions among older people with varying health and functioning status.
In our recent 12-month randomized exercise trial we showed that especially a combination of strength, balance, agility and jumping training prevented functional decline and bone fragility in relatively healthy home-dwelling elderly women [16]. The purpose of this study was to evaluate whether the observed exercise-induced benefits persisted one year after cessation of the exercise intervention.
Materials and methods
Design
This study is a one-year follow-up of a four-arm 12-month randomized, controlled exercise intervention trial comprising two different types of training programs, their combination, or controls. Thus, in this article the term “intervention” is used to mean the period of 12-month randomized, controlled exercise intervention. The results of the intervention have been reported previously [16]. A “follow-up” denotes the one-year period after the end of the intervention, and is the focus of this study.
All measurements were done at baseline, after intervention, and at follow-up. Of note, this follow-up study assesses only those physical performance or bone traits which showed a treatment-effect during the intervention [16], and the methods are described accordingly. In particular, after the intervention the treatment-effects were observed in dynamic balance, maximal isometric leg extension force, self-rated physical functioning, and bending strength of the tibial shaft and femoral neck.
Participants
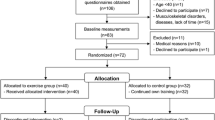
Originally, a questionnaire was sent to a random sample (n = 4,032) of 70-year-old to 79-year-old home-dwelling women in the city of Tampere, Finland, inquiring whether they were interested in participating randomized, controlled exercise intervention. Of 858 women who expressed their initial interest, 241 eligible women were invited to a screening examination. Of these women, 149 met the inclusion criteria (see below), and were randomly assigned to four groups: 1) a resistance training group (RES), 2) a balance-jumping training group (BAL), 3) a combination group doing resistance training and balance-jumping training (COMB), and 4) a non-training control group (CON). One hundred and forty-four women (97%) completed the intervention [16]. Of the 126 women who were willing to participate in the follow-up study, six withdrew before the follow-up measurements (Fig. 1).
In addition to age and willingness to participate, the inclusion criteria to the intervention study were the following: a full understanding of the study protocol, no history of any illness contraindicating exercise or limiting participation in the exercise program, no history of any illness affecting balance or bones, no uncorrected vision problems, and not taking medication known to affect balance or bone metabolism (for 12 months before the enrolment). A participant was excluded if she was involved in intense exercise more than twice a week or the T-score for femoral neck bone mineral density (BMD) was lower than −2.5.
Each participant provided her written informed consent before the study, and the study protocol was approved by the Ethics Committee of the Tampere University Hospital, Tampere, Finland.
Training programs (exercise intervention)
The supervised training programs during the intervention have been described in the original intervention report [16]. Briefly, exercise training classes were arranged 3 times a week for 12 months and were supervised by exercise leaders, who were trained to supervise these special training programs. All programs advanced progressively. The RES group training consisted of progressive resistance training (PRT) exercises for large muscle group exercises and the intensity increased from 50–60% of 1RM to 75–80% of 1RM (RM = repeated maximum). The BAL group training comprised modified aerobics and step aerobics, including a variety of balance, agility, and impact exercises. The degree of difficulty of movements, steps, impacts and jumps was gradually increased. The COMB training consisted of the above mentioned resistance and balance-jumping training in alternate weeks. The controls were asked to maintain their pre-study level of physical activity during the 12-month trial.
Questionnaires
In addition to baseline questionnaire of general health and habitual physical activity, all participants reported their health status and level of physical activity (type, frequency and duration) monthly during the intervention and follow-up. Reported weekly physical activity was converted to MET-hours/week [17].
Dietary intake and possible use of vitamin and mineral supplements were assessed by a complete 3-day (two weekdays and a Sunday) food record at baseline, after the intervention and at follow-up, and calculated by Micro-Nutrica software (Social Insurance Institution, Helsinki, Finland).
Physical functioning
Physical performance tests
Dynamic balance and agility was tested by a standardized figure-of-eight running test around two poles placed 10 m apart [18, 19]. The participant was asked to run or walk two laps of the course as fast as possible. The running time was measured using a stop-watch. The best attempt of two trials was recorded. The maximal isometric leg extension force was measured with a leg press dynamometer (Tamtron, Tampere, Finland) at a knee angle of 90 degrees with precision of about 5% [20].
Self-rated physical functioning
Self-rated physical functioning was assessed with the standardized Finnish Physical Functioning Scale of Rand 36-Item Health Survey [21, 22]. The participants filled in the questionnaire at home and it was checked together with the participant during her visit for the physical performance tests. The scale comprises ten questions on coping with daily activities, such as running, lifting heavy things, climbing stairs of several floors, and walking half a kilometer. Each item is scored as either a major restriction (0 points), minor restriction (50 points) or no restriction (100 points). An individual physical functioning index score is the mean of scores all answered items.
Bone measurements
The right proximal femur was measured with dual-energy X-ray absorptiometry (DXA, Norland XR-26, Norland Inc., Fort Atkinson, WI, USA), according to our standard procedures [23]. Then, the gross structure of the narrowest section of femoral neck was analyzed using the hip structure analysis (HSA) [24]. In this study, section modulus (Z) (as an index of bending strength) was used. The in vivo precision of Z is about 5% [25].
The peripheral quantitative computed tomography (pQCT), (XCT 3000, Stratec Medizintechnik GmbH, Pforzheim, Germany) was performed at midshaft (cortical bone) of the tibia, according to our standard procedures [26]. The density-weighted polar section modulus (BSI, an index of torsion bending strength) was used. In our laboratory, the in vivo precision of this measurement is 2.5% [26].
Statistical analyses
All results were based on the intention-to-treat analyses (ITT) of all available participants. In addition to the ITT analyses, efficacy analyses for the exercise were done. The inclusion criterion for the efficacy analysis was that the average training frequency of an individual was twice a week or more during the trial. It is recalled, that only those variables which showed a significant treatment-effect after the intervention were used as outcome variables in this study.
Linear mixed models with the restricted maximum likelihood estimation (REML) were used to assess the effects of exercise intervention at 12 months and the one-year follow-up. This type of analysis for repeated measures allows incorporation of incomplete longitudinal data into the models. Post hoc between-group comparisons were performed using Sidak’s adjustment for multiple comparisons. Due to the skewed distributions in some outcome variables and obtain the relative between-group differences, log-transformed variables of outcome were used in the linear mixed model. Proportional (%) differences and their 95% confidence intervals (CI) were achieved by antilog of mean difference in changes between the groups.
Results
Attendance at the follow-up study
The follow-up assessment was done to 120 (81%) women. There were ten non-attendants (refused and withdrew) in the CON group and from four to six in the training groups. (Fig. 1). The CON group non-attendants were slightly older and heavier, and more of them reported a decline in the self-rated physical functioning during the intervention as compared to the attendants. The baseline bone values of the non-attendants did not differ from the attendants, except slightly higher femoral neck section modulus (Z) among the attendants of the RES group. Also, the attendants had slightly better baseline dynamic balance and agility in the RES and CON groups, and isometric leg extension force in the COMB group compared to the respective non-attendants. In the training groups, the training compliance was somewhat better among the follow-up attendants than non-attendants.
Descriptive characteristics
Descriptive baseline characteristics of the study groups are given in Table 1. At baseline there were no between-group differences. The mean duration of moderate physical activity (4.5 MET) between the groups varied from 4 to 6 hours per week during the follow-up, and did not significantly differ from non-intervention-related physical activity during the intervention period. Six women in the RES group and eight in the COMB group continued resistance training at least at some level during the follow-up. Additionally, four women in the BAL group and one of the controls started resistance training during the follow-up.
During the one year follow-up period, participants reported 11 falls in the RES and BAL groups each, 13 falls in the COMB group and 14 falls in the CON group. In detail, nine women (27%) in the RES group, 10 (32%) in the BAL group, six (20%) in the COMB group, and ten (39%) in the CON group fell at least once during the follow-up period. One woman in the COMB group suffered a hip fracture due to a bicycle accident, and another woman in the RES group suffered a hip fracture along with a rib fracture as consequence of a fall from over 1 meter height. Also, one woman in the BAL group had a shoulder fracture and one woman in the control group had a patella fracture, both caused by a fall.
Physical functioning
Physical performance
The absolute values at baseline and exercise effect on physical performance variables after the intervention and at the follow-up are given in Table 2.
After the intervention, mean gain in leg extension isometric force was statistically significantly greater in the RES group (12%; 95% CI: 4 to 20) and in the COMB group (9%; 1 to 17) compared to the controls. However, at the follow-up, no between-group differences were seen (Fig. 2).
Physical functioning variables: The trainees’ age-adjusted percentage differences in change compared to controls (mean, 95% CI) after the intervention (12 months) and at the one-year follow-up (24 months) (ITT analysis). A = leg extensor force, B = dynamic balance and agility, C = self-rated physical functioning RES, resistance training group; BAL, balance-jumping training group; COMB, combination training group
Twenty-three subjects (19%) were unable to perform the figure-of-eight running test in the follow-up measurements with no between-group differences. Exercise intervention significantly improved the figure-of-eight running time in the COMB (7%; 3% to 10%) and BAL (5%; 1% to 8%) groups, respectively, compared to the CON group. At the follow-up, a 4% training effect (1% to 8%) was still observed in the COMB group compared with the CON group (Fig. 2). Furthermore, in the efficacy-analysis the exercise-effect seen at the follow-up enhanced and was also seen in the BAL group (trained at least twice a week during the intervention) (Table 2).
Self-rated physical functioning
Borderline statistical difference was seen in the self-rated physical functioning between the COMB and CON groups (9%; 0 to 19%) after the intervention, favoring the combination training. At the follow-up, the within-group variance had increased and the between-group difference had disappeared (Fig. 2).
Bone rigidity
Exercise effects on bone traits after 12-month intervention and one-year follow-up are given in Table 2. After the intervention, there was a significant between-group difference in the section modulus (Z) at the femoral neck between the RES and COMB groups (4%; 0% to 7%) favoring the resistance training. However, the difference was diminished at the follow-up, and did not reach statistical significance (Fig. 3).
Bone variables: The trainees’ age-adjusted percentage differences in change compared to controls (mean, 95% CI) after the intervention (12 months) and at the one-year follow-up (24 months). A = section modulus (Z) of the femoral neck (ITT analysis), B = tibial shaft bone strength index (BSI) (efficacy analysis*) RES, resistance training group; BAL, balance-jumping training group; COMB, combination training group. * Trainees who trained an average a twice a week or more
In contrast, there was a borderline trend that the 1.9% exercise benefit in the tibial shaft bone strength index in those COMB trainees who trained at least twice a week, was still partly maintained at the follow-up (1.3%; −0.1 to 2.7%, p = 0.065) (Fig. 3).
Discussion
In this one-year follow-up of the 12-month randomized, controlled exercise trial among healthy elderly women, some exercise-induced benefits in the dynamic balance and rigidity of the tibia were still seen one year after cessation of the supervised training. However, the training effect in muscle force and self-rated physical functioning had disappeared.
Previously it has been shown that gains in balance achieved by intensive balance training can be maintained to some extent by one weekly low-intensity Tai Chi training among community-dwelling elderly people [27]. However, in studies where supervised training has been completely stopped, exercise-induced benefits in balance and agility have been lost [14, 28–30]. In contrast to these latter findings, we found that about half of the training benefits in dynamic balance and agility were still seen in the COMB group at the follow-up, one year after the end of the supervised training. In addition, training effect was partly maintained among the active BAL trainees. Shorter training and follow-up periods, different designs (non-RCT) and methods to assess balance and agility [28–30], as well as younger [14] or frailer participants [28] may at least partly explain why the previous studies have obtained different results than we did.
In contrast to the partial maintenance of dynamic balance and agility, the training effect on the lower limb muscle force and physical functioning disappeared during the one-year follow-up time. It is well known that after cessation of strength training the training-induced muscle force begins to decrease, although muscle force gains among older adults achieved by strength training can be maintained to some extent from 5 to 27 weeks [31–33]. However, one year appears to be too long a period to maintain major gains in lower limb muscle force [34] unless the strength training is continued at least at some level [31, 34, 35].
An additional year increases older person’s risk to become ill and thus may well decline or even collapse her or his functional ability. This was also seen in this follow-up study. The ~10% beneficial treatment effect seen in self-rated physical functioning of the COMB group women had vanished—partly due to large within-group variability at the follow-up. In this context, it is recalled that those women in the control group who participated in the follow-up study were slightly younger and fewer of them had negative changes in the self-rated physical functioning during the intervention than the non-attending control persons. This was not the case in the training groups, and thus this fact may partly explain the reduced functionality differences between the training groups and control group at the follow-up.
The “use it or lose it” principle applies also to maintenance of improved bone rigidity after cessation of (vigorous) exercise. However, this notion arises largely from assessment of bone mass rather than structure or geometry [36–38]. It is well known that DXA in itself is not an adequate tool to assess cortical and trabecular density or other structural particulars [39]. However, these structural traits are pertinent to bone rigidity [40]. Moreover, they may change without changes in BMD or BMC [41–43]. Recently Sornay-Rendu and co-workers [4] found that fragility fractures among elderly women were associated with architectural alterations of trabecular and cortical bone which were partly independent of low BMD. In our study, apparently the weight-bearing tibia was particularly loaded during our exercises, and ~2% training effect was seen in the bone strength index at the tibial shaft among active COMB trainees after the intervention. More than a half of this effect in bone rigidity appeared to be maintained one year after cessation of the training program. However, this finding was based on a statistical borderline trend, and need therefore to be confirmed in future studies.
As far as we know, this is the first study to demonstrate possible maintenance of dynamic balance and agility one year after cessation of supervised high-intensity training in relatively healthy elderly women. Furthermore, a positive sign was seen that some benefits in bone strength might still be present. There are many possible explanations for these observations. Firstly, the most effective training program (COMB) was high-intensity in nature combining many effective training components, such as versatile balance and agility exercises, jumping exercises and progressive resistance training. Secondly, the participants performed intensive training (twice a week on average) for 12 months enabling one to achieve larger and probably more permanent effects, perhaps not only on balance and agility per se, but also on overall mobility functions. Thirdly, the participants of our study did not stop exercise entirely after the training intervention. Average moderate physical activity varied from 4 to 6 hours per week between groups during the follow-up period, being highest in the COMB group. Thus, habitual physical activity may also play a role in maintenance of the achieved benefits. As shown earlier, the benefits can, at least partly, be maintained if exercise is continued, even at lower level [11, 27]. However, in our study a lower volume resistance training and general physical activity were only weakly associated with the changes seen at the follow-up.
There are several strengths in this study. First, this follow-up study evaluated the maintenance of the treatment-effects of a randomized controlled exercise intervention trial of a well-defined group of elderly women. Second, bone structure, instead of conventional BMC or BMD, was assessed, and third, two different training programs, and their combination, were compared.
Our study had also some limitations. All participants did not continue to the follow-up study, although the participation rate was yet quite high (81%) at the follow-up. In addition, as noted above, the attending controls were slightly younger and maintained their self-rated physical functioning better during the intervention than their non-attendants counterparts, a fact that may have led to underestimation of actual maintenance of exercise-induced benefits. Finally, we had some missing data at the follow-up. This was taken into consideration in the used statistical method allowing incorporation of incomplete longitudinal data into the model.
In summary, exercise-induced benefits in dynamic balance and agility of initially healthy elderly women may be partly maintained at least for one year after cessation of 12-month high-intensity resistance and balance-jumping training. The same might concern the rigidity of the loaded tibia. However, in order to maintain the achieved training effects in the other relevant factors related to independent living and prevention of falls and fracture, such as muscle force or physical functioning, moderate-to-vigorous exercise probably should be continued at some level.
In terms of clinical importance, the present findings may help to devise training programs for prevention of falls and fragility fractures of healthy elderly people. Since it is unlikely that elderly people are able or willing to continue high-intensity training for years, the supervised intensive training should, perhaps, be delivered periodically, an approach in which habitual physical exercise is applied between the high-intensity training periods. However, future long-term studies are needed to test the usefulness and effectiveness of periodical training.
References
Carter ND, Kannus P, Khan KM (2001) Exercise in the prevention of falls in older people: a systematic literature review examining the rationale and evidence. Sports Med 31:427–438
Tinetti ME (2003) Preventing of falls in the elderly persons. N Engl J Med 348:42–49
Cummings SR, Nevitt MC, Browner WS et al (1995) Risk factors for hip structure in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332:814–815
Sornay-Rendu E, Bountroy S, Munoz F et al (2007) Alterations of cortical and trabecular architecture are associated with fractures in postmenopausal women, partially independent of decreased BMD measured by DXA: The OFELY Study. J Bone Miner Res 22:425–433
Gillespie LD, Gillespie WJ, Robertson MC et al. (2003) Interventions for preventing falls in elderly people. The Cochrane Database of Systematic Reviews, Issue 4
Bonaiuti D, Shea B, Iovine R et al. (2002) Exercise for preventing and treating osteoporosis in postmenopausal women. The Cochrane Database of Systematic Reviews, Issue 2
Liu-Ambrose T, Khan KM, Eng JJ et al (2004) Resistance and agility training reduce fall risk in women aged 75 to 85 with low bone mass: A 6-month randomized, controlled trial. J Am Geriatr Soc 52:657–665
Englund U, Littbrand H, Sondell A et al (2005) A 1-year combined weight-bearing training program is beneficial for bone mineral density and neuromuscular function in older women. Osteoporos Int 16:1117–1123
Korpelainen R, Keinänen-Kiukaanniemi S, Heikkinen J et al (2006) Effect of impact exercise on bone mineral density in elderly women with low BMD: a population-based randomized controlled 30-month intervention. Osteoporos Int 17:109–118
Korpelainen R, Keinänen-Kiukaanniemi S, Heikkinen J et al (2006) Effects of exercise on extraskeletal risk factors for hip fractures in elderly women with low BMD: A population-based randomized controlled trial. J Bone Miner Res 21:772–779
Heinonen A, Kannus P, Sievänen H et al (1999) Good maintenance of high-impact activity-induced bone gain by voluntary, unsupervised exercises: an 8-month follow-up of a randomized controlled trial. J Bone Miner Res 14:125–128
Häkkinen K, Alen M, Kallinen M et al (2000) Neuromuscular adaptation during prolonged strength training, detraining and re-strength-training in middle-aged and elderly people. Eur J Appl Physiol 83:51–62
Kontulainen S, Heinonen A, Kannus P et al. (2004) Former exercisers of an 18-month intervention display residual aBMD benefits compared with control women 3.5 years post-intervention: a follow-up of a randomized controlled high-impact trial. 15:248–251
Uusi-Rasi K, Sievänen H, Heinonen A et al (2004) Effect of discontinuation of alendronate treatment and exercise on bone mass and physical fitness: 15-month follow-up of a randomized, controlled trial. Bone 35:799–805
Liu-Ambrose TY, Khan KM, Eng JJ et al (2005) The beneficial effects of group-based exercises on fall risk profile and physical activity persist 1 year postintervention in older women with low bone mass: Follow-up after withdrawal of exercise. J Am Geriatr Soc 53:1767–1773
Karinkanta S, Heinonen A, Sievänen H et al (2007) A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: randomized, controlled trial. Osteoporos Int 18:453–462
Ainsworth BE, Hashell WL, Whitt MC et al (2000) Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 32:S498–S516
Carter ND, Khan KM, McKay HA et al (2002) Community-based exercise program reduces risk factors for falls in 65- to 75-year old women with osteoporosis: randomized controlled trial. CMAJ 167:997–1004
Uusi-Rasi K, Kannus P, Cheng S et al (2003) Effect of alendronate and exercise on bone and physical performance of postmenopausal women: a randomized controlled trial. Bone 33:132–143
Heinonen A, Sievänen H, Viitasalo J et al (1994) Reproducibility of computer measurement of maximal isometric strength and electromyography in sedentary middle-aged women. Eur J Appl Physiol 348:1343–1347
Hays RD, Donald Sherbourne C, Mazel RM (1993) The RAND 36-item Health Survey 1.0. Health Econ 2:217–227
Aalto AM, Aro AR, Teperi J (1999) Rand-36 as a measure of health-related quality of life. Reliability, construct validity and reference values in the Finnish general population. (In Finnish with an English summary) Research Reports, The National Research and Development Center for Welfare and Health (STAKES), Helsinki, Finland, vol 101
Sievänen H, Kannus P, Nieminen V et al (1996) Estimation of various mechanical characteristics of human bones using dual energy x-ray absorptiometry: Methodology and precision. Bone 18:17S–27S
Beck TJ, Looker AC, Ruff CB et al (2000) Structural trends in the aging femoral neck and proximal shaft: analysis of third national health and nutrition examination survey dual-energy X-ray absorptiometry data. J Bone Miner Res 15:2297–2304
Nikander R, Sievänen H, Heinonen A et al (2005) Femoral neck structure in adult female athletes subjected to different loading modalities. J Bone Miner Res 20:520–528
Sievänen H, Koskue V, Rauhio A et al (1998) Peripheral quantitative computed tomography in human long bones: evaluation of in vitro and in vivo precision. J Bone Miner Res 13:871–882
Wolfson L, Whipple R, Derby C et al (1996) Balance and strength training in older adults: Intervention gains and Tai Chi maintenance. J Am Geriatr Soc 44:498–506
Helbostad JL, Sletvold O, Moe-Nilssen R (2004) Effects of home exercises and group training on functional abilities in home-dwelling older persons with mobility and balance problems. A randomized study. Aging Clin Exp Res 16:113–121
Toraman NF, Ayceman N (2005) Effects of six weeks of detraining on retention of functional fitness of old people after nine weeks of multicomponent training. Br J Sports Med 39:565–568
Toulette C, Thevenon A, Fabre C (2006) Effects of training and detraining on the static and dynamic balance in elderly fallers and non-fallers: A pilot study. Disabil Rehabil 28(2):125–133
Lexell J, Downham DY, Larsson Y et al (1995) Heavy-resistance training in older Scandinavian men and women: short- and long-term effects on arm and leg muscles. Scand J Med Sci Sports 5:329–341
Sforzo GA, McManis BG, Black D et al (1995) Resilience to exercise detraining in healthy older adults. J Am Geriatr Soc 43:209–215
Taaffe DR, Marcus R (1997) Dynamic muscle strength alterations to detraining and retraining in elderly men. Clin Physiol 17:311–324
Porter MM, Nelson ME, Fiatarone Singh MA et al (2002) Effects of long-term resistance training and detraining on strength and physical activity in older women. J Aging Phys Act 10:260–720
Trappe S, Williamson D, Godard M (2002) Maintenance of whole muscle strength and size following resistance training in older men. J Gerontol Biol Sci Med Sci 57A:B138–B143
Karlsson MK (2003) The skeleton in long-term perspective - Are exercise induced benefits eroded by time? J Musculoskel Neuron Interact 3:348–351
Dalsky GP, Stocke KS, Ehsani AA et al (1988) Weight-bearing exercise training andlumbar bone mineral content in postmenopausal women. Ann Intern Med 108:824–828
Iwamoto J, Takeda T, Ichimura S (2001) Effect of exercise training and detraining on bone mineral density in postmenopausal women with osteoporosis. J Orthop Sci 6:128–132
Sievänen H (2000) A physical model for dual-energy X-ray absorptiometry—derived bone mineral density. Invest Radiol 35:325–330
Currey JD (2001) Bone strength: what are we trying to measure? Calsif Tissue Int 68:205–210
Järvinen TLN, Kannus P, Sievänen H et al (1998) Randomized controlled study of effects of sudden impact loading on rat femur. J Bone Miner Res 13:1475–1482
Adami S, Gatti D, Braga V et al (1999) Site-specific effects of strength training on bone structure and geometry of ultradistal radius in postmenopausal women. J Bone Miner Res 14:120–124
Warden SJ, Fuchs RK, Castillo AB et al (2007) Exercise when young provides lifelong benefits to bone structure and strength. J Bone Miner Res 22:251–259
Acknowledgments
We thank all the study participants for taking part of this study. We also thank statistician Matti Pasanen, MSc, for statistical consultation, Katriina Ojala, MSc, for physical performance measurements, and Virpi Koskue for DXA and pQCT measurements. The work was financially supported by the Finnish Ministry of Education, Medical Research Fund of the Tampere University Hospital, and the Miina Sillanpää foundation.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karinkanta, S., Heinonen, A., Sievänen, H. et al. Maintenance of exercise-induced benefits in physical functioning and bone among elderly women. Osteoporos Int 20, 665–674 (2009). https://doi.org/10.1007/s00198-008-0703-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0703-2