Abstract
Introduction
This study aimed to compare the sensitivity and specificity of various published indices for identifying elderly Chinese females at risk of osteoporosis in Singapore.
Methods
The indices considered were the Simple Calculated Osteoporosis Risk Estimation (SCORE), the Osteoporosis Risk Assessment Instrument (ORAI), the Age Bulk One or Never Estrogens (ABONE), body weight (WEIGHT), and the Osteoporosis Self-Assessment Tool for Asians (OSTA). Altogether, 135 postmenopausal Chinese female subjects aged 55 years and older participated in the study, and their bone mineral density (BMD) was measured with dual-energy x-ray absorptiometry. Subjects were classified as osteoporotic if their femoral neck BMD T-score was −2.5 or lower. Receiver operating characteristic (ROC) curves were generated to determine the indices’ cut-off points, sensitivity, and specificity.
Results
OSTA had the highest discriminatory power, with an estimated area under the ROC curve of 0.82. This was followed by SCORE (0.80), WEIGHT (0.78), ORAI (0.76), and ABONE (0.70). At the cut-off point of −2, OSTA achieved sensitivity and specificity of 91% and 59%, respectively.
Conclusion
The study showed that OSTA is an effective index for identifying postmenopausal women at risk for osteoporosis.
Similar content being viewed by others
Introduction
Osteoporosis, a systemic skeletal disease characterised by low bone mineral density (BMD), causes considerable morbidity and mortality. Older persons with the condition are at much greater risk for developing hip fractures from accidents such as falls. It is estimated that about 26% of the elderly who suffer osteoporotic hip fractures die within a year after the injury [1].
This is a major concern for Asian countries where populations are greying rapidly. It is projected that 50% of the world’s hip fractures will occur in that continent by the end of 2050 [2]. In view of the ageing demographic structure and rising osteoporotic hip fracture rate, Singapore is expected to experience substantial inflation in related health care costs [1, 3]. This poses a serious challenge to the nation.
Due to a natural decline in bone density after menopause, most osteoporotic fractures occur in older women. To permit prevention and early intervention, it is therefore important to identify postmenopausal women at risk of developing osteoporosis. However, mass screening using dual-energy x-ray absorptiometry (DXA), which is widely regarded as the gold standard for diagnosing osteoporosis, is not recommended owing to its cost [4–5]. As such, it is useful to consider several well-cited indices [6–10] for identifying elderly subjects at risk of developing osteoporosis. These indices aim to assess how risk factors, such as old age, low body weight, low estrogen level, and history of rheumatoid arthritis, are associated with low BMD.
Generally, these indices have moderate to high sensitivity but low specificity [11]. Although widely applied in the Caucasian and Asian populations, most of the indices were not validated in the Singaporean context. Therefore, this study aimed to compare the sensitivity and specificity of these indices [6–10] for identifying Chinese women in Singapore, aged 55 years and older, who were at risk for osteoporosis.
Methods
Sample
One hundred and thirty-five free-living ambulant Chinese postmenopausal women aged 55 years and older were recruited from the Tanjong Rhu community in the eastern part of Singapore. Using housing type as a surrogate measure for socioeconomic status, recruited subjects were representative of the socioeconomic status of Singaporeans and had a wide range of body mass index (BMI). The sample size was determined based on estimating the proportions of subjects in the different categories of BMI status: 50% in the normal range of 18.5–22.9 kg/m2, 30% in the overweight category of ≥23 kg/m2, and 20% in the underweight category of <18.5 kg/m2 [12, 13]. Dropouts were replaced by matching gender, housing type, and BMI. Approved by the Medical Ethics Committee, Health Promotion Board, Singapore, the study was scheduled to begin in March 2003.
Data
Upon giving their informed consent to participate in the study, eligible subjects were invited to Changi General Hospital, Singapore, to complete a short screening questionnaire and BMD measurements. The subjects were interviewed by a trained interviewer on diet, physical activity, quality of life, smoking status, and current medications.
BMD measurement of the femoral neck and lumbar spine was performed by DXA using a Hologic QDR 4500W densitometer (S/N 49088). All DXA measurements were conducted by a qualified radiologist. Body weight was measured on a calibrated mechanical scale, and height was measured with a wall-mounted stadiometer, with subjects wearing light indoor clothing only and without shoes. Food intake was also assessed using a validated interviewer-administered food frequency questionnaire [14].
Indices
The various indices considered in this study were the Simple Calculated Osteoporosis Risk Estimation (SCORE), the Osteoporosis Risk Assessment Instrument (ORAI), the Age Bulk One or Never Estrogens (ABONE), body weight criterion (WEIGHT), and the Osteoporosis Self-Assessment Tool for Asians (OSTA) [6–10]. Table 1 shows the indices’ scoring systems and published results.
SCORE, one of the first attempts to develop predictive rules for screening osteoporotic patients, was developed in an American cohort of 1,102 postmenopausal women aged 45 years and older of all ethnic backgrounds [6]. ORAI was developed and validated in the Canadian Multicentre Osteoporosis Study comprising 926 noninstitutionalised female subjects aged 45 years and older [7]. ABONE was developed with the data of 1,610 postmenopausal white women [8], and WEIGHT was based on 175 randomly-selected women (aged 28–74 years) in Sweden [9]. OSTA was developed with 860 postmenopausal Asian women in eight countries (People's Republic of China, Taiwan, Hong Kong, Korea, Malaysia, Singapore, Thailand, and the Philippines) [10]. It had been validated in various studies consisting of postmenopausal Japanese, Korean, and Hong Kong women [10, 15, 16].
Statistical analysis
The primary outcome considered in this paper was femoral neck BMD on the left region as determined by DXA. In addition, the spine BMD was also analysed. Based on World Health Organization (WHO) criteria [17], the subjects were classified as osteoporotic (BMD T-score ≤ −2.5) or nonosteoporotic (BMD T-score >−2.5).
With the published cut-off points (Table 1), the sensitivity and specificity for the indices were computed in the study sample of 135 subjects. The receiver operating characteristic (ROC) curves [18–20] were then generated to empirically determine the indices’ optimal cut-off points, sensitivity, and specificity in the same study sample. The optimal cut-off of an index was identified at the point nearest the top left-hand corner of the ROC curve [21]. The indices were compared by means of area under the curves (AUC) at 1% level of significance, taking into account the numerical difference in AUCs and its standard error, which in turn depends on the correlation between ROC curves [20]. Other things being equal, a low correlation will result in a large standard error, thus suggesting the AUC difference to be nonsignificant.
The data was analysed with Stata 7.0 (Stata Corporation, Texas, USA).
Results
Interrupted by the severe acute respiratory syndrome (SARS) outbreak, the study was concluded in August 2003. Table 2 summarises the characteristics of subjects included in the study. The mean age of the postmenopausal women was about 68 years. Overall, the proportions of subjects found to be osteoporotic based on femoral neck BMD T-scores ≤−2.5 and spine BMD T-scores ≤−2.5 were 24% and 27%, respectively. The mean body weight and mean BMI were 58.8 kg and 25.4 kg/m2, respectively.
The sensitivity and specificity based on the published cut-off points of the indices (with femoral neck BMD) are presented in Table 3. SCORE, ORAI, and ABONE attained the maximum sensitivity of 100%, but their ability to correctly identify nonosteoporotic subjects was far from satisfactory. WEIGHT also had a high sensitivity of 97.0% and a low specificity of 18.6%. OSTA had the same sensitivity as WEIGHT, but its specificity was highest among all five indices (43.1%).
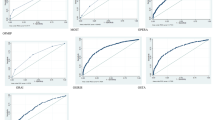
The results based on generated ROC curves are presented in Table 4. For OSTA and WEIGHT, lower cut-off values represent higher risk of osteoporosis (low BMD). On the other hand, higher values for the other indices, namely ORAI, SCORE, and ABONE, indicate higher risk of developing osteoporosis.
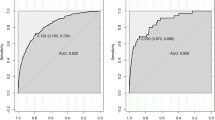
OSTA had the highest discriminatory power, with an estimated AUC of 0.82 (Fig. 1). At the cut-off point of −2, OSTA achieved sensitivity and specificity of 90.9% and 58.8%, respectively (Table 4). Note that the identified optimal cut-off was lower than the published cut-off point of −1 (Table 1).
Receiver operating characteristic curves based on femoral neck bone mineral density T-score ≤−2.5 (n=135). a Simple Calculated Osteoporosis Risk Estimation(SCORE). b Osteoporosis Risk Assessment Instrument (ORAI). c Age, Bulk, One or Never Estrogens (ABONE). d Osteoporosis Self-Assessment Tool for Asians (OSTA). e Body weight criterion (WEIGHT)
The next index with the largest estimated AUC was SCORE, with ≥8 identified as the optimum cut-off point (sensitivity 93.9%, specificity 60.8%). This optimal cut-off point, determined empirically from the analysis, was higher than the published result (Table 1).
The body weight criterion, with an estimated AUC of 0.78, identified 54.0 kg as the optimum cut-off point. As such, the criterion suggests that subjects weighing <54.0 kg were at risk. While its sensitivity was about 70%, the criterion managed to identify 77.5% of the nonosteoporotic subjects correctly.
With an estimated AUC of 0.76, ORAI correctly identified about 76% of the osteoporotic subjects at an optimum cut-off point of ≥20. Its specificity was about 67%.
The AUC of ABONE was 0.70. In terms of sensitivity, ABONE correctly identified about 82% of the osteoporotic subjects at cut-off point 3 (possible range: 1–3). However, its specificity of 55.9% was lowest among the indices considered in this study.
Results with lumbar spine BMD are reported in Table 5. OSTA and WEIGHT reported the largest estimated AUC at 0.73, followed by SCORE (0.72) and ORAI (0.68). ABONE had the lowest AUC at 0.66.
There was no significant difference in AUC among OSTA, SCORE, ORAI, ABONE, and WEIGHT in the two above-mentioned analyses in which femoral neck and lumbar spine BMD were used [20]. Although the numerical difference in AUCs between OSTA and ABONE was more than 10% when femoral neck BMD was considered (Table 4), the result was not significant in view of the low correlation between the two ROC curves [20].
Discussion
Simple risk assessment tools provide a quick and inexpensive way for identifying persons at risk of osteoporosis and hip fractures. Such indices are extremely useful in communities where access to BMD measurement is limited and costly.
This empirical study showed that the various indices considered were useful in identifying postmenopausal elderly Chinese females with osteoporosis. Based on ROC analysis with femoral neck BMD, the sensitivity of the indices was above 69% (Table 4). A high sensitivity is essential because it provides reliable evidence for physicians to start early treatment for patients at risk of osteoporosis. All indices yielded a specificity of no less than 55% (Table 4).
Numerically, OSTA yielded the highest AUC at 0.82, with sensitivity and specificity of 91% and 59%, respectively (Table 4). While its AUC was not significantly higher than SCORE, OSTA is a more convenient tool in the sense that only age and body weight are required in computation. This is a desirable feature of OSTA because other indices require more detailed information such as that regarding estrogen use and history of rheumatoid arthritis. While more complicated than WEIGHT, OSTA yielded a higher AUC and sensitivity.
There was no significant difference in AUCs among OSTA, SCORE, ORAI, ABONE, and WEIGHT. This could be partly due to the limited sample size [19]. Moreover, the correlations between ROC curves were generally low. It is also not clinically significant in detecting a less than 10% difference in AUCs (Table 4).
It is worthwhile to note that the original published cut-off of OSTA was ≤−1, based on femoral neck BMD of a cohort of 860 women in eight Asian countries (Table 1). On the other hand, this study suggests a lower cut-off at −2 (Table 4). The difference in cut-off points may be explained by demographic differences in the samples. The cohort in the original OSTA study included younger women (reported age range 45–88 years), whereas this study considered only postmenopausal women aged 55 years and older. This highlights that OSTA’s optimal cut-off point may vary with different age groups. Moreover, the original OSTA study used sensitivity to select the optimum cut-off, whereas this study adopted the conventional approach by giving equal attention to both sensitivity and specificity.
As such, further studies should be carried out to determine how OSTA performs in different age groups (for example, 55–69 years, 70–80 years, and ≥80 years) of postmenopausal women. In addition, subjects from other ethnic groups may also be included in future studies. With diversified demographic characteristics in subjects and a larger sample, a more conclusive answer to the index’s generalisability and applicability may be derived.
Conclusion
This empirical study showed that OSTA is an effective index for identifying postmenopausal Chinese women at risk for osteoporosis. To ensure its applicability, further work should be done to evaluate its performance in different age range and other ethnic groups in Singapore.
References
Wong MK, Arjandas, Ching LK, Lim SL, Lo NN (2002) Osteoporotic hip fractures in Singapore: costs and patient’s outcome. Ann Acad Med Singapore 31:3–7
Cooper C, Campian G, Melton LJ (1992) Hip fracture in the elderly: a worldwide projection. Osteoporos Int 2:285–289
Koh LKH, Saw SM, Lee JJM, Leong KH, Lee J (2001) Hip fracture incidence rates in Singapore 1991–1998. Osteoporos Int 12:311–318
Scientific Advisory Board, Osteoporosis Society of Canada (1996) Clinical practice guidelines for the diagnosis and management of osteoporosis. CMAJ 155:1113–1133
Council of the National Osteoporosis Foundation (1996) Guidelines for the early detection of osteoporosis and prediction of fracture risk. S Afri Med J 86:1113–1116
Lydick E, Cook K, Turpin J, Melton M, Stine R, Byrnes C (1998) Development and validation of a simple questionnaire to facilitate identification of women likely to have low bone density. Am J of Manag Care 4:37–48
Cadarette SM, Jaglal SB, Kreiger N, McIssac WJ, Darlington GA, Tu JV (2000) Development and validation of the osteoporosis risk assessment instrument to facilitate selection of women for bone densitometry. CMAJ 162:1289–1294
Weinstein L, Ullery B (2000) Identification of at-risk women for osteoporosis screening. Am J Obstet Gynecol 183:547–549
Michaelsson K, Bergstrom R, Mallmin H, Holmberg L, Wolk A, Ljunghall S (1996) Screening for osteoporosis: selection by body composition. Osteoporos Int 6: 120–126
Koh LKH, Sedrine WB, Torralba TP, Kung A, Fujiwara S, Chan SP, Huang QR, Rajatanavin R, Tsai KS, Park HM, Reginster JY (2001) A simple tool to identify Asian women at increased risk of osteoporosis. Osteoporos Int 12:699–705
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measure of bone mineral density predicts occurrence of osteoporotic fractures. BMJ 312:1254–1259
Scheaffer RL, Mendenhall W, Ott L (1990) Elementary survey sampling 4th edn. PWS Kent, Boston
Ministry of Health (2000) National health survey 1998. Ministry of Health, Singapore
Food and Nutrition Department (1994) Food consumption study 1993. Ministry of Health, Singapore
Park HM, Sedrine WB, Reginster JY, Ross PD, OSTA (2003) Korean experience with the OSTA risk index for osteoporosis: a validation study. J Clin Densitom 6:247–250
Kung AW, Ho AY, Sedrine WB, Reginster JY, Ross PD (2003) Comparison of a simple clinical risk index and quantitative bone ultrasound for identifying women at increased risk of osteoporosis. Osteoporos Int 14:716–721
Ministry of Health, National Medical Research Council, Osteoporosis Society of Singapore (2002) Clinical practice guideline: osteoporosis. Ministry of Health, Singapore
Metz CE (1978) Basic principles of ROC analysis. Semin Nucl Med 8:283–298
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36
Hanley JA, McNeil BJ (1983) A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 148:839–843
Altman DG (1999) Practical statistics for medical research. Chapman & Hall, Boca Raton
Acknowledgements
We would like to express our appreciation to the Ministry of Health, Singapore, for providing sampling support and for liaising with the authorities for conducting the study. Special thanks go to Dr. Paul Deurenberg, Nutrition Consultant, for reviewing the paper. The study was funded by the Health Promotion Board, Singapore.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chan, SP., Teo, C.C., Ng, S.A. et al. Validation of various osteoporosis risk indices in elderly Chinese females in Singapore. Osteoporos Int 17, 1182–1188 (2006). https://doi.org/10.1007/s00198-005-0051-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-005-0051-4