Abstract
Introduction and hypothesis
Urinary incontinence (UI) is a widespread issue in women that severely impacts quality of life. The addition of sugar is associated with multiple adverse effects on health. This study examined the potential association between added sugar intake and UI.
Methods
Adult females from the National Health and Nutrition Examination Survey database (2005–2018) were included in this study. The primary outcomes were the prevalence of stress urinary incontinence (SUI), urge urinary incontinence (UUI), and mixed urinary incontinence (MUI). Weighted logistic regression, stratified logistic regression, restricted cubic spline regression, and sensitivity analyses were utilized to determine whether added sugar was associated with UI after multivariate adjustment.
Results
A total of 14,927 participants met the inclusion criteria. The results revealed a heightened prevalence of SUI, UUI, and MUI in the fourth quartile of added sugar energy percentage (OR = 1.304, 95% confidence interval [CI] = 1.105–1.539; OR = 1.464, 95% CI = 1.248–1.717; OR = 1.657, 95% CI = 1.329–2.065 respectively). The effect was more pronounced in young women and the subgroup analyses did not reveal any noteworthy interaction effects. According to the sensitivity analyses, the results for SUI and the MUI were consistent with those of the primary analyses.
Conclusions
The excessive intake of added sugar among women may increase their risk of SUI and MUI. Our study highlights the negative effects of added sugar on female genitourinary health and highlights the need for universal access to healthy diets.

Similar content being viewed by others
Data Availability
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
References
Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology of lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21(2):167–78. https://doi.org/10.1002/nau.10052.
Abufaraj M, Xu T, Cao C, et al. Prevalence and trends in urinary incontinence among women in the United States, 2005–2018. Am J Obstet Gynecol. 2021;225(2):166.e1–12. https://doi.org/10.1016/j.ajog.2021.03.016.
Wood LN, Anger JT. Urinary incontinence in women. BMJ. 2014;349:g4531. https://doi.org/10.1016/10.1136/bmj.g4531.
Maserejian NN, Giovannucci EL, McVary KT, McGrother C, McKinlay JB. Dietary macronutrient and energy intake and urinary incontinence in women. Am J Epidemiol. 2010;171(10):1116–25. https://doi.org/10.1093/aje/kwq065.
Phillips JA. Dietary guidelines for Americans, 2020–2025. Workplace Health Saf. 2021;69(8):395. https://doi.org/10.1177/21650799211026980.
World Health Organization. Guideline: sugars intake for adults and children. 2015. https://pubmed.ncbi.nlm.nih.gov/25905159. Accessed 1 December 2023.
Pacheco LS, Lacey JV, Martinez ME, et al. Sugar-sweetened beverage intake and cardiovascular disease risk in the California teachers study. J Am Heart Assoc. 2020;9(10):e014883. https://doi.org/10.1161/jaha.119.014883.
Paglia L. The sweet danger of added sugars. Eur J Paediatr Dent. 2019;20(2):89. https://doi.org/10.23804/ejpd.2019.20.02.01.
Rogo-Gupta LJ, Yang L, Stefanick ML, et al. Low-fat dietary pattern reduces urinary incontinence in postmenopausal women: post hoc analysis of the women’s health initiative diet modification trial. AJOG Glob Rep. 2022;2(1):100044. https://doi.org/10.1016/j.xagr.2021.100044.
Sun Y, Chen H, Bai Y, Zhang T, Bai W, Jiang B. Ketogenic diet may be a new approach to treatment stress urinary incontinence in obese elderly women: report of five cases. BMC Womens Health. 2022;22(1):402. https://doi.org/10.1186/s12905-022-01987-5.
Ying Y, Xu L, Huang R, et al. Relationship between blood glucose level and prevalence and frequency of stress urinary incontinence in women. Female Pelvic Med Reconstr Surg. 2022;28:304–10. https://doi.org/10.1097/SPV.0000000000001112.
Haring B, Crandall CJ, Wu C, et al. Dietary patterns and fractures in postmenopausal women results from the Women’s Health Initiative. JAMA Intern Med. 2016;176(5):645–52. https://doi.org/10.1001/jamainternmed.2016.0482.
Bowman SA, Clemens JC, Shimizu M, Friday JE. Food patterns equivalents database 2017–2018: methodology and user guide. Beltsville, Maryland: Food Surveys Research Group, Beltsville Human Nutrition Research Center, Agricultural Research Service, US Department of Agriculture. 2020. http://www.arsusdagov/nea/bhnrc/fsrg. Accessed 1 December 2023.
Yin S, Yang Z, Zhu P, et al. Association between added sugars and kidney stones in US adults: data from national health and nutrition examination survey 2007–2018. Front Nutr. 2023;10:1226082. https://doi.org/10.3389/fnut.2023.1226082.
Yuan Y, Tan W, Huang Y, et al. Association between oxidative balance score and urinary incontinence in females: results from the national health and nutrition examination survey in 2005–2018. Int Urol Nephrol. 2023;55:2145–54. https://doi.org/10.1007/s11255-023-03665-3.
Ricciuto L, Fulgoni III VL, Gaine PC, et al. Intakes of added sugars, with a focus on beverages and the associations with nutrient adequacy in US adults (NHANES 2003–2018). Nutrients. 2023;15(18):3916. https://doi.org/10.3390/nu15183916.
Dallosso HM, McGrother CW, Matthews RJ, Donaldson MMK, Leicestershire MRC Incontinence Study Group. The association of diet and other lifestyle factors with overactive bladder and stress incontinence: a longitudinal study in women. BJU Int. 2003;92(1):69–77. https://doi.org/10.1046/j.1464-410X.2003.04271.x.
Dallosso H, Matthews R, McGrother C, Donaldson M, Leicestershire MRC Incontinence Study Group. Diet as a risk factor for the development of stress urinary incontinence: a longitudinal study in women. Eur J Clin Nutr. 2004;58(6):920–6. https://doi.org/10.1038/sj.ejcn.1601913.
Markland AD, Vaughan C, Huang A, et al. Effect of vitamin D supplementation on urinary incontinence in older women: ancillary findings from a randomized trial. Am J Obstet Gynecol. 2009;226(4):535.e1–12. https://doi.org/10.1016/j.ajog.2021.10.017.
Roosen A, Chapple CR, Dmochowski RR, et al. A refocus on the bladder as the originator of storage lower urinary tract symptoms: a systematic review of the latest literature. Eur Urol. 2009;56(5):810–9. https://doi.org/10.1016/j.eururo.2009.07.044.
Hubeaux K, Deffieux X, Ismael SS, Raibaut P, Amarenco G. Autonomic nervous system activity during bladder filling assessed by heart rate variability analysis in women with idiopathic overactive bladder syndrome or stress urinary incontinence. J Urol. 2007;178(6):2483–7. https://doi.org/10.1016/j.juro.2007.08.036.
Moshtaghian H, Louie JCY, Charlton KE, et al. Added sugar intake that exceeds current recommendations is associated with nutrient dilution in older Australians. Nutrition. 2016;32(9):937–42. https://doi.org/10.1016/j.nut.2016.02.004.
Lee HS, Lee JH. Vitamin D and urinary incontinence among Korean women: a propensity score-matched analysis from the 2008–2009 Korean national health and nutrition examination survey. J Korean Med Sci. 2017;32(4):661–5. https://doi.org/10.3346/jkms.2017.32.4.661.
Zyczynski HM, Albo ME, Goldman HB, et al. Change in overactive bladder symptoms after surgery for stress urinary incontinence in women. Obstet Gynecol. 2015;126(2):423–30. https://doi.org/10.1097/aog.0000000000000929.
Cosentino F, Eto M, De Paolis P, et al. High glucose causes upregulation of cyclooxygenase-2 and alters prostanoid profile in human endothelial cells: role of protein kinase C and reactive oxygen species. Circulation. 2003;107(7):1017–23. https://doi.org/10.1161/01.Cir.0000051367.92927.07.
Castro MC, Massa ML, Gonzalez Arbelaez L, Schinella G, Gagliardino JJ, Francini F. Fructose-induced inflammation, insulin resistance and oxidative stress: a liver pathological triad effectively disrupted by lipoic acid. Life Sci. 2015;137:1–6. https://doi.org/10.1016/j.lfs.2015.07.010.
O’Connor L, Imamura F, Brage S, Griffin SJ, Wareham NJ, Forouhi NG. Intakes and sources of dietary sugars and their association with metabolic and inflammatory markers. Clin Nutr. 2018;37(4):1313–22. https://doi.org/10.1016/j.clnu.2017.05.030.
Tyagi P, Barclay D, Zamora R, et al. Urine cytokines suggest an inflammatory response in the overactive bladder: a pilot study. Int Urol Nephrol. 2010;42(3):629–35. https://doi.org/10.1007/s11255-009-9647-5.
Subak LL, Wing R, West DS, et al. Weight loss to treat urinary incontinence in overweight and obese women. N Engl J Med. 2009;360(5):481–90. https://doi.org/10.1056/NEJMoa0806375.
Zitnanova I, Rakovan M, Paduchova Z, et al. Oxidative stress in women with perimenopausal symptoms. Menopause. 2011;18(11):1249–55. https://doi.org/10.1097/gme.0b013e318224fa3d.
Acknowledgements
We thank all the contributors and participants in the National Health and Nutrition Examination Survey. We also thank Zhang Jing (Shanghai Tongren Hospital) for his work on the NHANES database. His outstanding work, nhanesR package, and webpage, made it easier for us to explore the NHANES database.
Funding
None.
Author information
Authors and Affiliations
Contributions
Y.Y.: project development, data collection, manuscript writing; Y.H. and H.H.: data analysis; S.Z.: data collection; Z.H.: project development.
Corresponding author
Ethics declarations
Declarations
The studies involving humans were approved by the National Institute of Health Research Ethics Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Conflicts of interest
None.
Additional information
Handling Editor: Catherine Matthews
Editor in Chief: Maria A. Bortolini
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
192_2024_5794_MOESM4_ESM.tif
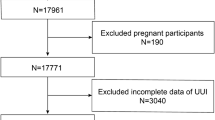
Supplementary file4 The participants selected flow chart from NHANES (2005–2018). NHANES National Health and Nutrition Examination Survey. (TIF 2432 KB)
192_2024_5794_MOESM5_ESM.tiff
Supplementary file5 Subgroup analysis for SUI (forest plots). Above adjusts for age, ethnicity, educational attainment, marital status, PIR, BMI, physical activity, smoking, eGFR, SII, cholesterol, triglyceride, creatinine, uric acid, total energy intake, total water intake, protein intake, fat intake, alcohol, DM, hypertension, CVD, menopause/hysterectomy, and vaginal deliveries. In each case, the model was not adjusted for the stratification variable itself. SUI stress urinary incontinence, PIR poverty-to-income ratio, BMI body mass index, eGFR estimated glomerular filtration rate, SII systemic immune-inflammatory, DM diabetes mellitus, hypertension, CVD cardiovascular disease. (TIFF 376 KB)
192_2024_5794_MOESM6_ESM.tiff
Supplementary file6 Subgroup analysis for UUI (forest plots). Above adjusts for age, ethnicity, educational attainment, marital status, PIR, BMI, physical activity, smoking, eGFR, SII, cholesterol, triglyceride, creatinine, uric acid, total energy intake, total water intake, protein intake, fat intake, alcohol, DM, hypertension, CVD, menopause/hysterectomy, and vaginal deliveries. In each case, the model was not adjusted for the stratification variable itself. UUI urge urinary incontinence, PIR poverty-to-income ratio, BMI body mass index, eGFR estimated glomerular filtration rate, SII systemic immune-inflammatory, DM diabetes mellitus, hypertension, CVD cardiovascular disease. (TIFF 374 KB)
192_2024_5794_MOESM7_ESM.tiff
Supplementary file7 Subgroup analysis for MUI (forest plots). Above adjusts for age, ethnicity, educational attainment, marital status, PIR, BMI, physical activity, smoking, eGFR, SII, cholesterol, triglyceride, creatinine, uric acid, total energy intake, total water intake, protein intake, fat intake, alcohol, DM, hypertension, CVD, menopause/hysterectomy, and vaginal deliveries. In each case, the model was not adjusted for the stratification variable itself. MUI mixed urinary incontinence, PIR poverty-to-income ratio, BMI body mass index, eGFR estimated glomerular filtration rate, SII systemic immune-inflammatory, DM diabetes mellitus, hypertension, CVD cardiovascular disease. (TIFF 377 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yuan, Y., Huang, Y., Huang, H. et al. Association Between Added Sugar Intake and Urinary Incontinence in Females: A Cross-sectional Population-based Study. Int Urogynecol J (2024). https://doi.org/10.1007/s00192-024-05794-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00192-024-05794-4