Abstract
Introduction and hypothesis
A previous randomized controlled trial (RCT) demonstrated that the app Tät II, for self-management of mixed urinary incontinence (MUI) and urgency urinary incontinence (UUI), yielded significant, clinically relevant improvements in symptom severity and quality of life (QoL) compared with a control group. We aimed to assess the cost-effectiveness of Tät II.
Methods
A cost–utility analysis with a 1-year societal perspective was carried out, comparing Tät II with an information app. Data were collected alongside an RCT: 122 community-dwelling women aged ≥18 years with MUI or UUI ≥2 times/week were randomized to 3 months of Tät II treatment focused on pelvic floor muscle training (PFMT) and bladder training (BT; n = 60), or to an information app (n = 62). Self-assessed data from validated questionnaires were collected at baseline and at 3-month and 1-year follow-ups. Costs for assessment, treatment delivery, incontinence aids, laundry, and time for PFMT and BT were included. We calculated quality-adjusted life-years (QALYs) using the International Consultation on Incontinence Modular Questionnaire Lower Urinary Tract Symptoms Quality of Life. The incremental cost-effectiveness ratio (ICER) between the groups was our primary outcome. Sensitivity analyses were performed.
Results
The mean age was 58.3 (SD = 9.6) years. Annual overall costs were €738.42 in the treatment group and €605.82 in the control group; annual QALY gains were 0.0152 and 0.0037 respectively. The base case ICER was €11,770.52; ICERs in the sensitivity analyses ranged from €−9,303.78 to €22,307.67.
Conclusions
The app Tät II is a cost-effective treatment method for women with MUI and UUI.
Similar content being viewed by others
Introduction
Urinary incontinence (UI) is defined as the complaint of involuntary loss of urine [1] and has a prevalence of about 25–45% among adult women [2]. There are three main types of UI: stress urinary incontinence (SUI), which is involuntary leakage of urine upon effort or physical exertion, sneezing, or coughing; urgency urinary incontinence (UUI), which is leakage associated with urgency; and mixed urinary incontinence (MUI) which is a combination of these symptoms [1]. SUI accounts for about half of all UI, followed by MUI and UUI respectively [2]. UI can have a negative impact on quality of life (QoL) and the impact increases with the severity of the leakage [3].
First-line treatment for all types of UI includes pelvic floor muscle training (PFMT). For MUI and UUI, bladder training is usually also recommended. As second-line treatment, pharmacological therapy can be considered [2, 4]. However, many affected women do not seek help. Embarrassment, shame, minimizing of problems, and a lack of knowledge about available efficient treatment can contribute to this [2].
Mobile technologies can be used for conservative self-management of UI and might increase satisfaction and adherence while reducing costs [5]. Women with MUI and UUI without alarm symptoms can be safely diagnosed and treated without face-to-face contact [6]. The eContinence project has developed the app Tät II for self-managed first-line treatment of female MUI and UUI, with a focus on PFMT and bladder training. The app has been evaluated in a randomized controlled trial (RCT) and shown to yield clinically relevant improvements regarding UI symptoms, urgency symptoms, and QoL [7].
Health economic evaluations are based on comparisons of the costs and effects of at least two treatment options and help to prioritize which treatments should be implemented. One commonly used method is the cost–utility analysis (CUA). A CUA can have either a health care perspective, which only includes costs borne by the health care system, or a societal perspective, where all costs are included regardless of who pays them [8]. In Sweden, the societal perspective is recommended [9]. The effect of treatment is defined by measuring QoL to calculate the change in quality-adjusted life-years (QALYs) [8]. The result is presented as an incremental cost-effectiveness ratio (ICER), and there are national [10] and international [11, 12] guidelines available to help evaluate the ICER.
Previous studies have evaluated the cost-effectiveness of internet-based and app-based treatment for SUI [13, 14], and for app-based treatment of SUI, MUI, and UUI compared with care as usual [15]. Here, we performed a cost–utility analysis of self-managed treatment of MUI and UUI, comparing the app Tät II with an app containing information but no treatment program.
Materials and methods
This is a deterministic CUA with a 1-year societal perspective, performed according to the principles established by Drummond et al. [8].
Study population and design
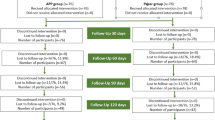
This CUA was based on data collected alongside an RCT evaluating the app Tät II, conducted in Sweden in 2017–2018, with full completion in early 2019. The RCT was registered at clinicaltrials.gov (ID:NCT03097549). [7]. The study flowchart of the RCT and the CUA is presented in Fig. 1.
Flowcharts of the randomized controlled trial (RCT) and the cost–utility analysis (CUA). The boxes represent the RCT and the green circles represent the CUA. The timeline shows the different time points (baseline and follow-ups) of the RCT where data used in the CUA were collected. The area above the red horizontal line represents the treatment app, and the area below the line represents the information app. The black arrow crossing the red line represents the information group getting access to the treatment app after the 3-month follow-up. The dashed line shows that the information group’s 3-month follow-up data were also used for the 1-year follow-up
The RCT’s study population consisted of 123 women with MUI or UUI, recruited via the research project’s website www.econtinence.se. Inclusion criteria were female sex, age ≥18 years, ≥2 or more leakages per week, symptom duration of ≥12 months, access to a smartphone, and ability to send and receive emails. Exclusion criteria included ongoing pregnancy, use of mirabegron or antimuscarinic drugs, use of another PFMT app, and UI surgery within the last 5 years. Other exclusion criteria concerned alarm symptoms indicating the need for physical examination and certain medical conditions: painful urges; previous pyelonephritis; ≥3 urinary tract infections in the last 12 months; dysuria; visible hematuria; uninvestigated bladder-emptying difficulties; metrorrhagia; cancer in the pelvic area, bladder, or bowels; decreased mobility or sensitivity in the legs or pelvic area; previous stroke; neurological disease; and diabetes. Assessment and diagnosis were based on self-completed web-based questionnaires (including validated symptom and QoL questionnaires, see below) sent by email to the participants, a 2-day bladder diary (frequency and measured volume of micturitions, and self-reported leakage episodes), and a telephone interview with a urotherapist to confirm the symptom diagnosis and the absence of exclusion criteria. There was no face-to-face contact with the participants at any time.
The participants were consecutively randomized to two groups. One group received the treatment app, Tät II (n = 60), which included an 11-step PFMT program prescribing training three times daily for 3 months, a seven-step bladder training program, psychoeducation, detailed information on each topic, general lifestyle advice, and individually tailored advice manually generated by a prespecified algorithm using information from each participant’s inclusion questionnaire and bladder diary. The development of the app and its included features have been described in detail elsewhere [7]. The other group (n = 63) received an app with brief information on each topic, but with no active treatment program. After 3 months of treatment, the treatment group was advised to maintain PFMT 2–3 times a week.
In this CUA, we included all participants from the RCT, except for one participant in the information group (total n = 122). The excluded participant had received an intravesical treatment for her UI symptoms prior to the 3-month follow-up.
Data collection
Data collected at baseline included age, body mass index (BMI), education level, occupation, medication use, smoking, parity, current PFMT, use of incontinence aids, extra laundry due to UI, data on UI symptoms, and condition-specific QoL.
The first follow-up was performed 3 months (15 weeks) after randomization and included data on UI symptoms, QoL, use of incontinence aids, and laundry. The participants were also asked to estimate how much time they spent on PFMT and bladder training, and to what extent they did other things, such as walking, watching TV, etc., while performing the exercises. The second follow-up was performed 12 months later and included data on the same topics.
However, the information group was offered access to the treatment app after the 3-month follow-up. Thus, to obtain a control group for this CUA, we included 1-year follow-up data only for the treatment group, whereas for the information group we assumed that data from the 3-month follow-up would remain unchanged for the rest of the year.
Symptom severity
Urinary incontinence symptoms were measured using the International Consultation on Incontinence Questionnaire - Urinary Incontinence Short Form (ICIQ-UI SF). The questionnaire consists of three scored items on frequency, amount of leakage, and the overall impact of UI on everyday life, summarized as an overall score of 0–21 points, with higher values indicating greater severity [16]. Based on the score, severity can be divided into the following categories: slight (1–5 points), moderate (6–12 points), severe (13–18 points), and very severe (19–21 points) [17].
Costs
We included all relevant costs accrued over the course of the first year in the calculations.
Assessment costs included the estimated time spent by our study coordinator in emailing each participant web links to the questionnaires and the 2-day bladder diaries, and the estimated time for the telephone interview conducted by the urotherapist. Treatment delivery cost included the time spent by one of the researchers manually registering the tailored advice for each participant in the treatment group. The time costs were based on the employees’ average gross hourly wage including general payroll taxes in 2017.
We did not include the cost of app development. This is normally not included in health economic analyses, because it is a one-time cost comparable with, for example, the basic education cost of the health care personnel.
Participants’ time spent on PFMT and bladder training was calculated by combining their reported time spent on PFMT and bladder training with the estimates of how much of that time they spent on also doing other things, and we included the time spent exclusively on training. Pricing of the participants’ time was calculated based on average wages for women in Sweden with the same education level as our total study population [18]. The cost per unit was the gross hourly wage and included general payroll taxes.
The price of incontinence aids was based on the price of different absorbent pads for urine leakage protection as collected from the largest pharmacy chain in Sweden. From this, a mean price per unit, referring to a single pad, was calculated.
We estimated the cost of laundry based on the literature and national records [19]. It included the costs of electricity, electricity taxes, water consumption, laundry detergent, and washing machine wear and tear. The latter was based on the average price of a washing machine, assuming a lifespan of 10 years and an average of five washes per week. Participants’ time spent on managing a load of laundry was estimated to be 7.5 min.
At the 1-year follow-up, 4 participants had received pharmacological treatment for their UI and, owing to the low number, we did not include calculations of this cost.
All costs are presented in Euros at the 2017 year-end level. At that time, 1 EUR = SEK 9.85.
Quality of life, utility weights, and quality-adjusted life-years
Condition-specific QoL was measured using the International Consultation on Incontinence Modular Questionnaire - Lower Urinary Tract Symptoms Quality of Life (ICIQ-LUTSqol) [20]. It consists of 19 items on different aspects of everyday life that might be affected by UI. Each item has four response choices: "never," "sometimes," "often," or "all the time," generating 1–4 points respectively. The values of the 19 items are summed to a total score of 19–76 points, with higher numbers indicating greater impact on QoL. We used an established index developed by Brazier et al. [21] to calculate QALYs from the questionnaire. The index incorporates 9 of the 19 items into a health state classification (a certain combination of items). Using the algorithms of the index, we then established syntax to translate the health state classifications into utility weights ranging from 0 (representing the worst) to 1 (the best imaginable health status).
Primary outcome
Our primary outcome was the ICER. To calculate the ICER we used the following formula:
Statistics
For comparisons between groups, we used the Chi-squared test for categorical variables and Student’s t test for continuous variables. For analyses of improvement of QoL within each group, we used paired t tests. The total QALY change in each group was calculated using the “area-under-the curve,” whereas we considered costs to change linearly. p values <0.05 were considered statistically significant. We used SPSS Statistics (version 27.0; IBM Corp) for Mac and Excel for Mac (version 16.45; Microsoft Corp).
Sensitivity analyses
We performed five univariate sensitivity analyses. In one, we adjusted the cost for one-third of our participants’ time by reducing the wages by 50% because they were retired. In the second, we halved the cost per unit of incontinence aids, considering that it might have been overestimated in our pricing, as women with UI presumably try to reduce the cost per unit by purchasing larger packages than those used in our first calculations. In the third we increased, and in the fourth we decreased, the time spent on PFMT and bladder training by 50%, thinking that there was a risk that the participants’ estimates of their time spent on training was either under- or overestimated in the base case. Finally, in the fifth, we removed the cost of participants’ time for training entirely. We also performed a multivariate sensitivity analysis, where we included the adjusted lower wage for the study population, the halved cost for incontinence aids, and the 50% lower value for the estimated time spent on training.
Ethics
The study was approved by the Regional Ethical Review Board, Umeå University (number 2016/523-31). We obtained informed consent from all participants after they were thoroughly informed. No reimbursements were given.
Results
Study population
This study included 122 participants (treatment group n = 60, information group n = 62). Baseline characteristics of the two groups (Table 1), such as age, body mass index, UI symptoms, and QoL were similar. An exception was education level, as participants in the information group had a somewhat lower level of education.
After 3 months, 2 participants (3.3%) were lost from the treatment group, and none from the information group. Of the participants in the treatment group, 85% (51 out of 60) responded to the 1-year follow-up.
Costs
The total assessment cost was €13.76 per participant in both groups. The treatment delivery cost (€2.42) was incurred only by the treatment group.
Participants in the treatment group had spent significantly more time on PFMT by the 3-month follow-up compared with participants in the information group (28.0 min vs 5.9 min per week, p <0.001). Thus, a higher cost for time spent on PFMT was seen in the treatment group compared with the information group (€330.83 vs €153.45), and for the treatment group this constituted the largest part of the total cost. The total annual cost was higher per participant in the treatment group (€741.62) than in the information group (€605.82; Table 2).
Quality-adjusted life-years change
Within both groups, there were significant improvements in QoL scores at the 3-month follow-up (mean ICIQ-LUTSqol reduction in the treatment group: 7.7, 95% CI 6.1–9.2) and mean ICIQ-LUTSqol reduction in the information group: 1.7, 95% CI 0.4–3.0). The improvement at the 3-month follow-up was maintained in the treatment group at the 1-year follow-up. The corresponding utility weights and QALY changes are presented in Fig. 2.
Total quality-adjusted life-years (QALY) change for the treatment app group and information app group. QALY change from baseline to 1-year follow-up. The timeline shows the three time points during the randomized controlled trial where data on participants’ quality of life were collected, using the International Consultation on Incontinence Questionnaire Lower Urinary Tract Symptoms Quality of Life (ICIQ-LUTSqol). The y-axis shows the mean utility weights, which were calculated based on results from the ICIQ-LUTSqol. The utility weights were then used to calculate the area under the curve for each graph, which represents the total QALY change over the year for each study group
Incremental cost-effectiveness ratio and sensitivity analysis
The ICERs for the base case and the sensitivity analyses are presented in Table 3. The ICER for the base case was €11,770.52. The treatment group had a higher total cost in all scenarios, but also larger QALY gains than the information group. The ICERs for the sensitivity analyses were within the range €−9,303.78 to €22,307.67, where the 50% increase and decrease in time spent on PFMT and bladder training resulted in the highest and lowest ICERs respectively.
Discussion
In this cost–utility analysis with a 1-year societal perspective, we demonstrate the cost-effectiveness of the app Tät II, which focuses on PFMT and bladder training for women with MUI and UUI, compared with an app containing information but no training programs. A higher overall cost was seen for the app Tät II, but also greater QALY gains than for the information app, resulting in a base case ICER of €11,770.52. The results were consistent in all tested scenarios.
Strengths and limitations
One strength of this study is that the population can be considered clinically relevant, because all participants actively sought care for their UI, and 96.7% had moderate or severe leakage. Other strengths include the performance of the RCT by an experienced research group according to current guidelines, its low loss to follow-up, and its use of validated [16, 20] questionnaires. Moreover, most costs and QALYs were based on actual data collected from the participants, and we used an established method to calculate the QALYs [21]. Finally, our results were stable in all sensitivity analyses.
One limitation of this study is the comparison group. It would have been interesting to compare the treatment app with a Swedish care-as-usual alternative, but UI treatment varies considerably and there is no gold standard. Given that only a minority of women with UI seek help [2], we consider the comparison with the information app plausible, as it represents a good no-treatment alternative. Moreover, it is possible that participants with MUI experienced UUI symptoms to a variable degree at baseline and thus responded differently to therapy. However, the RCT design should have minimized the impact of this. Other limitations include the relatively small size of the study (n = 122), which may add uncertainty to our results, and the lack of 1-year data for the information group. Instead, based on our previous studies where effects have remained stable for 1 and 2 years [22, 23], we assumed that the information groups’ 3-month data would remain unchanged for the rest of the year. Moreover, the results may be difficult to generalize. The web-based recruitment might have led to a selection bias in the study population. Internet use is widespread in Sweden; for example, in 2018, 90% of Swedish women aged 16–74 years used the internet daily [24]. Nevertheless, our population had a higher education level (63.9% had a university education ≥3 years) than the average Swedish female population in 2018; 30.5% of women aged 25–74 years had the same education level as those in our study [25]. However, it has previously been shown that education level does not seem to affect the ability to learn to perform PFMT [26].
Comparison with prior work
The total annual cost was higher in the treatment group than in the information group (€738.42 vs €605.82 respectively). This can be compared with the overall annual cost per participant in our previous CUAs; one compared an internet-based program to a postal treatment program for SUI (overall costs €596.50 and €596.20 respectively) [13], and one assessed the cost-effectiveness of self-management of SUI using the app Tät (overall cost €547.00) [14]. The largest cost in these studies was the participants’ time spent on PFMT, but as both focused on the treatment of SUI, neither included any time for bladder training. For further comparison, Loohuis et al. recently reported overall costs of app-based treatment for SUI, MUI, and UUI, using a 1-year societal perspective, of €1,520, and a cost of care-as-usual of €1,680 [15]. Moreover, from the OPAL study including women with SUI and MUI receiving basic PFMT, Hagen et al. presented an overall cost in the basic PFMT group of £1,535.26 (≈ €1,790) when applying a societal perspective for 24 months [27]. Pharmacological treatment, which is the recommended second-line treatment, is considerably more expensive. For example, Visco et al. presented a comparison of anticholinergics and intradetrusor Botox injections in the treatment of UUI, with annual per patient costs of $2,978 (€2,453) and $2,744 (€2,260) respectively [28].
The treatment group in our study had a total QALY gain of 0.0152, which can be translated into 5.5 additional days in the best imaginable health status for 1 year. The QALY gain observed in the treatment group was higher than that provided by an internet-based program focusing on PFMT for treatment of SUI (QALY gain 0.0104) [13], and for the app Tät, which is intended for self-management of SUI (QALY gain of 0.0101) [14]. It was also higher than the incremental QALY gains (0.01) reported by Albers-Heitner et al. from a primary care setting where women with SUI performed PFMT under the guidance of a specialist nurse or in a GP care-as-usual alternative [29]. The larger QALY gains in our study were expected, since MUI and UUI often have a greater negative impact on QoL than SUI [3, 30], and thus there is a larger potential for improvement. The QALY gain for the treatment group was lower than from pharmacological treatment, where QALY gains of 0.046 and 0.039 for anticholinergic and Botox treatment have been presented [28]. However, although the QALY gains in the treatment group might seem small, both MUI and UUI are common conditions and many women may be helped by the treatment; thus, on a population level, they imply a considerable effect.
The ICER for the base case was €11,770.52, whereas the ICERs for the sensitivity analyses were in the range €−9,303.78 to 22,307.67. Whether this represents cost-effectiveness or not depends on the willingness to pay for extra QALYS, and this might vary in different countries. In Sweden, an incremental cost per QALY gained of less than €10,000 is considered low, and a cost of €49,500–€99,000 is considered high [10]. In the UK, the NICE guidelines prescribe an additional cost for a new intervention in the range €22,500–34,000 (£20,000–30,000) per QALY gained to be considered cost-effective [11], whereas in the US, at least €41,000 ($50,000) per QALY gained is suggested as a threshold value for cost-effectiveness [12].
Clinical implication and future research
There is a need for cost-effective and easily accessible treatment methods for MUI and UUI, and this study provides additional knowledge for guidance when prioritizing what methods should be implemented in clinical practice. Although app treatment might not be the most suitable method for all women, Tät II could provide a new first-line treatment option for many affected women. However, this CUA was performed in a study setting, and when the app is used in other populations, costs and effects are likely to change. Thus, further evaluation of its cost-effectiveness when made publicly available would be of interest. Most likely, the overall costs will be lower in another population, which is not as highly educated as ours, resulting in a reduced cost for the participants’ time. Furthermore, the cost of PFMT would probably be reduced over time, as the women increasingly learn how to train while doing other things. On the other hand, costs of maintenance and technical support of the app will need to be added, but those costs will be split among many users.
Conclusions
The app Tät II is a cost-effective treatment method for women with MUI and UUI. It can be considered a new, first-line treatment option, and may be a way to reach more women wishing treatment.
References
Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26. https://doi.org/10.1007/s00192-009-0976-9.
Abrams PCL, Wagg A, Wein A, editors. Incontinence. 6th ed. Bristol: ICI-ICS. International Continence Society; 2017.
Coyne KS, Kvasz M, Ireland AM, Milsom I, Kopp ZS, Chapple CR. Urinary incontinence and its relationship to mental health and health-related quality of life in men and women in Sweden, the United Kingdom, and the United States. Eur Urol. 2012;61:88–95. https://doi.org/10.1016/j.eururo.2011.07.049.
Balk E, Adam GP, Kimmel H, Rofeberg V, Saeed I, Jeppson P, Trikalinos T. Nonsurgical treatments for urinary incontinence in women: a systematic review update. Rockville (MD): AHRQ Comparative Effectiveness Reviews; 2018.
Bernard S, Boucher S, McLean L, Moffet H. Mobile technologies for the conservative self-management of urinary incontinence: a systematic scoping review. Int Urogynecol J. 2020;31:1163–74. https://doi.org/10.1007/s00192-019-04012-w.
Huang AJ, Hess R, Arya LA, et al. Pharmacologic treatment for urgency-predominant urinary incontinence in women diagnosed using a simplified algorithm: a randomized trial. Am J Obstet Gynecol. 2012;206:444.e1–11. https://doi.org/10.1016/j.ajog.2012.03.002.
Wadensten T, Nystrom E, Franzen K, Lindam A, Wasteson E, Samuelsson E. A mobile app for self-management of urgency and mixed urinary incontinence in women: randomized controlled trial. J Med Internet Res. 2021;23:e19439. https://doi.org/10.2196/19439.
Drummond MS, Sculpher MJ, Torrance GW. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford: Oxford University Press; 2005.
The Dental and Pharmaceutical Benefits Agency (2012). The Dental and Pharmaceutical Benefits Agency, Stockholm, Sweden. https://www.tlv.se/in-english/medicines/health-economics.html. Accessed 14 Sept 2021
The National Board of Health and Welfare (2015). Methods for Developing National Guidelines. The National Board of Health and Welfare, Stockholm, Sweden. https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/dokument-webb/nationella-riktlinjer/nationella-riktlinjer-metodbeskrivning.pdf. Accessed 14 Sept 2021
National Institute for Health and Care Excellence (2014). Developing NICE guidelines: the manual. Incorporating economic evaluation. National Institute for Health and Care Excellence, UK. https://www.nice.org.uk/process/pmg20/chapter/incorporating-economic-evaluation. Accessed Sept 14 2021
Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness—the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371:796–7. https://doi.org/10.1056/NEJMp1405158.
Sjostrom M, Umefjord G, Lindholm L, Samuelsson E. Cost-effectiveness of an Internet-based treatment program for stress urinary incontinence. Neurourol Urodyn. 2013;34(3):244–50. https://doi.org/10.1002/nau.22540.
Sjostrom M, Lindholm L, Samuelsson E. Mobile app for treatment of stress urinary incontinence: a cost-effectiveness analysis. J Med Internet Res. 2017;19:e154. https://doi.org/10.2196/jmir.7383.
Loohuis A, van der Worp H, Wessels N, et al. Cost-effectiveness of an app-based treatment for urinary incontinence in comparison to care as usual in general practice: A pragmatic randomised controlled trial over 12 months. Authorea. 2021;19:e154. https://doi.org/10.22541/au.161330881.15636474/v1.
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23:322–30. https://doi.org/10.1002/nau.20041.
Klovning A, Avery K, Sandvik H, Hunskaar S. Comparison of two questionnaires for assessing the severity of urinary incontinence: the ICIQ-UI SF versus the incontinence severity index. Neurourol Urodyn. 2009;28:411–5. https://doi.org/10.1002/nau.20674.
Statistics Sweden (2017) Labour market, salary structure: whole economy. Statistics Sweden. https://www.statistikdatabasen.scb.se/pxweb/en/ssd/START__AM__AM0110__AM0110D/TidsserieUtbniva/. Accessed 28 Sept 2021.
Statistics Sweden (2017) Energy: energy prices on natural gas and electricity, prices on electricity for household consumers. Statistics Sweden. https://www.scb.se/en/finding-statistics/statistics-by-subject-area/energy/price-trends-in-the-energy-sector/electricity-prices-and-electricity-contracts/pong/tables-and-graphs/older-statistics/prices-on-electricity-for-household-consumers-2007/. Accessed 28 Sept 2021.
Kelleher CJ, Cardozo LD, Khullar V, Salvatore S. A new questionnaire to assess the quality of life of urinary incontinent women. Br J Obstet Gynaecol. 1997;104:1374–9. https://doi.org/10.1111/j.1471-0528.1997.tb11006.x.
Brazier J, Czoski-Murray C, Roberts J, Brown M, Symonds T, Kelleher C. Estimation of a preference-based index from a condition-specific measure: the King's Health Questionnaire. Med Decis Making. 2008;28:113–26. https://doi.org/10.1177/0272989X07301820.
Sjostrom M, Umefjord G, Stenlund H, Carlbring P, Andersson G, Samuelsson E. Internet-based treatment of stress urinary incontinence: 1- and 2-year results of a randomized controlled trial with a focus on pelvic floor muscle training. BJU Int. 2015;116:955–64. https://doi.org/10.1111/bju.13091.
Hoffman V, Soderstrom L, Samuelsson E. Self-management of stress urinary incontinence via a mobile app: two-year follow-up of a randomized controlled trial. Acta Obstet Gynecol Scand. 2017;96:1180–7. https://doi.org/10.1111/aogs.13192.
Statistics Sweden (2018) Living conditions: ICT usage in households and by individuals, average use of the internet by sex and study domain. Statistics Sweden. https://www.statistikdatabasen.scb.se/sq/99859?select. Accessed 28 Sept 2021.
Statistics Sweden (2018) Educational attainment of the population. Statistics Sweden. https://www.statistikdatabasen.scb.se/sq/99890. Accessed 28 Sept 2021.
Henderson JW, Wang S, Egger MJ, Masters M, Nygaard I. Can women correctly contract their pelvic floor muscles without formal instruction? Female Pelvic Med Reconstr Surg. 2013;19:8–12. https://doi.org/10.1097/SPV.0b013e31827ab9d0.
Hagen S, Bugge C, Dean SG, et al. Basic versus biofeedback-mediated intensive pelvic floor muscle training for women with urinary incontinence: the OPAL RCT. Health Technol Assess. 2020;24:1–144. https://doi.org/10.3310/hta24700.
Visco AG, Zyczynski H, Brubaker L, et al. Cost-effectiveness analysis of anticholinergics versus Botox for urgency urinary incontinence: results from the anticholinergic versus Botox comparison randomized trial. Female Pelvic Med Reconstr Surg. 2016;22:311–6. https://doi.org/10.1097/SPV.0000000000000277.
Albers-Heitner CP, Joore MA, Winkens RA, Lagro-Janssen AL, Severens JL, Berghmans LC. Cost-effectiveness of involving nurse specialists for adult patients with urinary incontinence in primary care compared to care-as-usual: an economic evaluation alongside a pragmatic randomized controlled trial. Neurourol Urodyn. 2012;31:526–34. https://doi.org/10.1002/nau.21204.
Åstrom Y, Asklund I, Lindam A, Sjostrom M. Quality of life in women with urinary incontinence seeking care using e-health. BMC Womens Health. 2021;21:337. https://doi.org/10.1186/s12905-021-01477-0.
Acknowledgements
We would like to thank the participating women for making this study possible. Many thanks also to our study administrator Susanne Johansson for holding it all together, to Anna Lindam for help with the statistical analyses, and to PhD student Towe Wadensten for advice and input throughout the study.
Funding
Open access funding provided by Umea University. This study was funded with grants from the County Council Region Jämtland Härjedalen (JLL-933083, JLL-930732), from the Northern County Councils (931113), and the Kamprad Family Foundation for Entrepreneurship, Research, and Charity (20170202).
Author information
Authors and Affiliations
Contributions
J. Ekersund: main contributor to data analysis and manuscript writing; E. Samuelsson: main contributor to project development and data collection, participated in data analysis and manuscript editing; L. Lindholm: participated in project development, data analysis, and manuscript editing; M. Sjöström: participated in project development, main responsibility for data analysis and manuscript writing.
Corresponding author
Ethics declarations
Conflicts of interests
The logos Tät and Tät.nu are registered as trademarks by the Swedish Patent and Registration office for eContinence AB, a Swedish e-health company founded in July 2021 with the aim of maintaining, spreading, commercializing, and further developing the apps created within the research project Tät.nu (eContinence.se). Malin Sjöström and Eva Samuelsson are cofounders and shareholders of eContinence AB and have a potential future financial gain in the app Tät II. Eva Samuelsson is the managing director of eContinence AB. Julia Ekersund and Lars Lindholm declare that they have no conflicts of interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ekersund, J., Samuelsson, E., Lindholm, L. et al. A mobile app for the treatment of female mixed and urgency incontinence: a cost-effectiveness analysis in Sweden. Int Urogynecol J 33, 1273–1282 (2022). https://doi.org/10.1007/s00192-022-05137-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05137-1