Abstract
Introduction and hypothesis
The objective was to investigate the impact of mindfulness-based stress reduction therapy on the urinary microbiome of patients with interstitial cystitis/bladder pain syndrome.
Methods
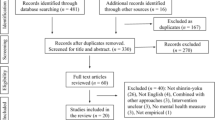
In this Institutional Review Board-approved prospective cohort study, patients with interstitial cystitis/bladder pain syndrome were recruited to attend an 8-week mindfulness-based stress reduction course involving yoga and meditation. Eligible participants were English-speaking women aged 18 or older with interstitial cystitis/bladder pain syndrome. All participants had a negative urinalysis within 2 months of enrollment and were currently undergoing first- or second-line treatment at the time of recruitment. The mindfulness-based stress reduction course met weekly for 1 h. A straight-catheter urine sample was obtained prior to and following the mindfulness-based stress reduction series. DNA from urine samples underwent bacterial 16S ribosomal gene sequencing at Johns Hopkins University Laboratories followed by taxonomic abundance and diversity analysis by Resphera Biosciences Laboratory. Participants completed validated symptom questionnaires pre- and post-intervention.
Results
A total of 12 participants completed the 8-week course and were included in the analysis. The average age was 59 and the majority identified as white. Patient symptoms, measured by the Urogenital Distress Inventory Short Form and Interstitial Cystitis Symptom and Pain Indices, improved significantly (all p < 0.05). Overall composition of the urinary microbiome changed significantly (p < 0.01) and demonstrated an increase in diversity following the intervention.
Conclusions
Mindfulness-based stress reduction therapy improves patient symptoms and was associated with significant changes in the urinary microbiome in patients with interstitial cystitis/bladder pain syndrome.




Similar content being viewed by others
References
Berry SH, Elliott MN, Suttorp M, Bogart LM, Stoto MA, Eggers P, et al. Prevalence of symptoms of bladder pain syndrome/interstitial cystitis among adult females in the United States. J Urol. 2011;186(2):540–4.
Suskind AM, Berry SH, Suttorp MJ, Elliott MN, Hays RD, Ewing BA, et al. Health-related quality of life in patients with interstitial cystitis/bladder pain syndrome and frequently associated comorbidities. Qual Life Res. 2013;22(7):1537–41.
Hanno PM, Erickson D, Moldwin R, Faraday MM, American Urological Association. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol. 2015;193(5):1545–53.
Nickel JC, Tripp DA, Pontari M, Moldwin R, Mayer R, Carr LK, et al. Interstitial cystitis/painful bladder syndrome and associated medical conditions with an emphasis on irritable bowel syndrome, fibromyalgia and chronic fatigue syndrome. J Urol. 2010;184(4):1358–63.
Sampalli T, Berlasso E, Fox R, Petter M. A controlled study of the effect of a mindfulness-based stress reduction technique in women with multiple chemical sensitivity, chronic fatigue syndrome, and fibromyalgia. J Multidiscip Healthc. 2009;2:53–9.
Slavin SL, Rogers RG, Komesu Y, Omotosho T, Hammil S, Lewis C, et al. Complementary and alternative medicine (CAM) use in women with pelvic floor disorders: a cohort study. Int Urogynecol J. 2010;21(4):431–7.
Zernicke KA, Campbell TS, Blustein PK, Fung TS, Johnson JA, Bacon SL, et al. Mindfulness-based stress reduction for the treatment of irritable bowel syndrome symptoms: a randomized wait-list controlled trial. Int J Behav Med. 2013;20(3):385–96.
Kanter G, Komesu YM, Qaedan F, Jeppson PC, Dunivan GC, Cichowski SB, et al. Mindfulness-based stress reduction as a novel treatment for interstitial cystitis/bladder pain syndrome: a randomized controlled trial. Int Urogynecol J. 2016;27(11):1705–11.
Siddiqui H, Lagesen K, Nederbragt AJ, Jeansson SL, Jakobsen KS. Alterations of microbiota in urine from women with interstitial cystitis. BMC Microbiol. 2012;12:205.
Abernethy MG, Rosenfeld A, White JR, Mueller MG, Lewicky-Gaupp C, Kenton K. Urinary microbiome and cytokine levels in women with interstitial cystitis. Obstet Gynecol. 2017;129(3):500–6.
Hanno PM, Burks DA, Clemens Q, Dmochowski RR, Erickson D, FitzGerald MP, et al. American Urological Association guideline: diagnosis and treatment interstitial cystitis/bladder pain syndrome. Interstitial Cystitis Guidelines Panel of the American Urological Association Education and Research, Inc. J Urol. 2011;185(6):2162–70.
Harvey MA, Kristjansson B, Griffith D, Versi E. The incontinence impact questionnaire and the urogenital distress inventory: a revisit of their validity in women without a urodynamic diagnosis. Am J Obstet Gynecol. 2001;185(1):25–31.
O'Leary MP, Sant GR, Fowler FJ Jr, Whitmore KE, Spolarich-Kroll J. The interstitial cystitis symptom index and problem index. Urology. 1997;49(5A Suppl):58–63.
Nicholas MK. The pain self-efficacy questionnaire: taking pain into account. Eur J Pain. 2007;11(2):153–63.
Ware J Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33.
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The female sexual function index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26(2):191–208.
Hilt EE, McKinley K, Pearce MM, Rosenfeld AB, Zilliox MJ, Mueller ER, et al. Urine is not sterile: use of enhanced urine culture techniques to detect resident bacterial flora in the adult female bladder. J Clin Microbiol. 2014;52(3):871–6.
Wolfe AJ, Toh E, Shibata N, Rong R, Kenton K, Fitzgerald M, et al. Evidence of uncultivated Bacteria in the adult female bladder. J Clin Microbiol. 2012;50(4):1376.
Jumpstart Consortium Human Microbiome Project Data Generation Working Group. Evaluation of 16s rDNA-based community profiling for human microbiome research. PLoS One. 2012;7:e39315.
Daquigan N, Seekatz AM, Greathouse KL, Young VB, White JR. High-resolution profiling of the gut microbiome reveals the extent of Clostridium difficile burden. NPJ Biofilms Microbiomes. 2017;3(1):1–8.
Drewes JL, White JR, Dejea CM, Fathi P, Iyadorai T, Vadivelu J, et al. High-resolution bacterial 16S rRNA gene profile meta-analysis and biofilm status reveal common colorectal cancer consortia. NPJ Biofilms Microbiomes. 2017;3(1):1–2.
Caporaso JG, Kuczynski J, Stombaugh J, et al. QIIME allows analysis of high-throughput community sequencing data. Nat Methods. 2010;7(5):335–6.
Xia Y, Sun J. Hypothesis testing and statistical analysis of microbiome. Genes Diseases. 2017;4(3):138–48.
Price TK, Lin H, Gao X, Thomas-White KJ, Hilt EE, Mueller ER, et al. Bladder bacterial diversity differs in continent and incontinent women: a cross-sectional study. Am J Obstet Gynecol 2020;223(5):729.e1–e10.
Acknowledgements
The authors thank the TriHealth Hatton Institute Medical Education Research Fund for funding this work. The authors thank Eunsun Yook, Clinical Research Specialist, for statistical analysis and data interpretation; Christine Popa, licensed yoga instructor, for mindfulness-based stress reduction course development and leadership; Vivian Ghodsi, clinical research coordinator, for study coordination and data collection.
Funding
This study was funded by the TriHealth Hatton Institute Medical Education Research Fund, Cincinnati, OH, USA.
Author information
Authors and Affiliations
Contributions
A. Shatkin-Margolis: project development, data collection, manuscript writing; J. White: project development, data collection, manuscript writing/editing; A. Jedlicka: project development, data collection, manuscript writing/editing; T. Tam: project development, data collection, manuscript editing; A. Hill: project development, data collection, manuscript editing; J. Yeung: project development, manuscript editing; C. Crisp: project development, manuscript editing; R. Pauls: project development, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shatkin-Margolis, A., White, J., Jedlicka, A.E. et al. The effect of mindfulness-based stress reduction on the urinary microbiome in interstitial cystitis. Int Urogynecol J 33, 665–671 (2022). https://doi.org/10.1007/s00192-021-04812-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04812-z