Abstract
Introduction and hypothesis
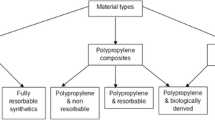
We compared the impact of a mesh manufactured from the soft elastomer polydimethylsiloxane (PDMS) to that of a widely used lightweight polypropylene (PP) mesh. To achieve a similar overall device stiffness between meshes, the PDMS mesh was made with more material and therefore was heavier and less porous. We hypothesized that the soft polymer PDMS mesh, despite having more material, would have a similar impact on the vagina as the PP mesh.
Methods
PDMS and PP meshes were implanted onto the vaginas of 20 rabbits via colpopexy. Ten rabbits served as sham. At 12 weeks, mesh-vagina complexes were explanted and assessed for contractile function, histomorphology, total collagen, and glycosaminoglycan content. Outcome measures were compared using one-way ANOVA and Kruskal-Wallis testing with appropriate post-hoc testing.
Results
Relative to sham, vaginal contractility was reduced following the implantation of PP (p = 0.035) but not the softer PDMS (p = 0.495). PP had an overall greater negative impact on total collagen and glycosaminoglycan content, decreasing by 53% (p < 0.001) and 54% (p < 0.001) compared to reductions of 35% (p = 0.004 and p < 0.001) with PDMS. However, there were no significant differences in the contractility, collagen fiber thickness, total collagen, and glycosaminoglycan content between the two meshes.
Conclusions
Despite having a substantially higher weight, PDMS had a similar impact on the vagina compared to a low-weight PP mesh, implicating soft polymers as potential alternatives to PP. The notion that heavyweight meshes are associated with a worse host response is not applicable when comparing across materials.



Similar content being viewed by others
References
Barber MD, Brubaker L, Burgio KL, Richter HE, Nygaard I, Weidner AC, Menefee SA, Lukacz ES, Norton P, Schaffer J, Nguyen JN, Borello-France D, Goode PS, Jakus-Waldman S, Spino C, Warren LK, Gantz MG, Meikle SF. Comparison of 2 transvaginal surgical approaches and perioperative behavioral therapy for apical vaginal prolapse: the OPTIMAL randomized trial. JAMA J Am Med Assoc. 2014;311(10):1023–34. https://doi.org/10.1001/jama.2014.1719.
Jelovsek JE, Barber MD, Norton P, Brubaker L, Gantz M, Richter HE, Weidner A, Menefee S, Schaffer J, Pugh N, Meikle S. Effect of uterosacral ligament suspension vs sacrospinous ligament fixation with or without perioperative behavioral therapy for pelvic organ vaginal prolapse on surgical outcomes and prolapse symptoms at 5 years in the OPTIMAL randomized clinical trial. JAMA J Am Med Assoc. 2018;319(15):1554–65. https://doi.org/10.1001/jama.2018.2827.
FDA. Urogynecologic surgical mesh: update on the safety and effectiveness of transvaginal placement for pelvic organ prolapse. 2011.
Nygaard I, Brubaker L, Zyczynski HM, Cundiff G, Richter H, Gantz M, Fine P, Menefee S, Ridgeway B, Visco A, Warren LK, Zhang M, Meikle S. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. Jama. 2013;309(19):2016–24. https://doi.org/10.1001/jama.2013.4919.
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–6.
Greca FH, De Paula JB, Biondo-Simões MLP, Da Costa FD, Da Silva APG, Time S, Mansur A. The influence of differing pore sizes on the biocompatibility of two polypropylene meshes in the repair of abdominal defects: experimental study in dogs. Hernia. 2001;5(2):59–64. https://doi.org/10.1007/s100290100001.
Greca FH, Souza-Filho ZA, Giovanini A, Rubin MR, Kuenzer RF, Reese FB, Araujo LM. The influence of porosity on the integration histology of two polypropylene meshes for the treatment of abdominal wall defects in dogs. Hernia. 2008;12(1):45–9. https://doi.org/10.1007/s10029-007-0276-6.
Klinge U, Klosterhalfen B, Birkenhauer V, Junge K, Conze J, Schumpelick V. Impact of polymer pore size on the interface scar formation in a rat model. J Surg Res. 2002;103(2):208–14.
Orenstein SB, Saberski ER, Kreutzer DL, Novitsky YW. Comparative analysis of histopathologic effects of synthetic meshes based on material, weight, and pore size in mice. J Surg Res. 2012;176(2):423–9.
Klinge U, Klosterhalfen B, Conze J, Limberg W, Obolenski B, Öttinger AP, Schumpelick V. Modified mesh for hernia repair that is adapted to the physiology of the abdominal wall. Eur J Surg. 1998;164(12):951–60.
Klinge U, Klosterhalfen B, Muller M, Ottinger AP, Schumpelick V. Shrinking of polypropylene mesh in vivo: an experimental study in dogs. Eur J Surg Acta Chirurgica. 1998;164(12):965–9. https://doi.org/10.1080/110241598750005156.
Klinge U, Junge K, Stumpf M, Öttinger AP, Klosterhalfen B. Functional and morphological evaluation of a low-weight, monofilament polypropylene mesh for hernia repair. J Biomed Mater Res. 2002;63(2):129–36. https://doi.org/10.1002/jbm.10119.
Goh JTW. Biomechanical properties of prolapsed vaginal tissue in pre- and postmenopausal women. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(2):76–9.
Knight KM, Moalli PA, Nolfi A, Palcsey S, Barone WR, Abramowitch SD. Impact of parity on ewe vaginal mechanical properties relative to the nonhuman primate and rodent. Int Urogynecol J Pelvic Floor Dysfunct 2016;1–9. https://doi.org/10.1007/s00192-016-2963-2.
Lei L, Song Y, Chen R. Biomechanical properties of prolapsed vaginal tissue in pre- and postmenopausal women. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(6):603–7. https://doi.org/10.1007/s00192-006-0214-7.
Feola A, Abramowitch S, Jallah Z, Stein S, Barone W, Palcsey S, Moalli P. Deterioration in biomechanical properties of the vagina following implantation of a high-stiffness prolapse mesh. BJOG Int J Obstetr Gynaecol. 2013;120(2):224–32.
Jallah Z, Liang R, Feola A, Barone W, Palcsey S, Abramowitch SD, Yoshimura N, Moalli P. The impact of prolapse mesh on vaginal smooth muscle structure and function. BJOG Int J Obstetr Gynaecol. 2016;123(7):1076–85. https://doi.org/10.1111/1471-0528.13514.
Liang R, Abramowitch S, Knight K, Palcsey S, Nolfi A, Feola A, Stein S, Moalli PA. Vaginal degeneration following implantation of synthetic mesh with increased stiffness. BJOG Int J Obstetr Gynaecol. 2013;120(2):233–43.
Knight KM, Artsen AM, Routzong MR, King GE, Abramowitch SD, Moalli PA. New Zealand white rabbit: a novel model for prolapse mesh implantation via a lumbar colpopexy. Int Urogynecol J. 2020;31(1):91–9. https://doi.org/10.1007/s00192-019-04071-z.
Neuman RE, Logan MA. The determination of hydroxyproline. J Biol Chem. 1950;184(1):299–306.
Bhana B, Iyer RK, Chen WLK, Zhao R, Sider KL, Likhitpanichkul M, Simmons CA, Radisic M. Influence of substrate stiffness on the phenotype of heart cells. Biotechnol Bioeng. 2010;105(6):1148–60. https://doi.org/10.1002/bit.22647.
Engler AJ, Carag-Krieger C, Johnson CP, Raab M, Tang HY, Speicher DW, Sanger JW, Sanger JM, Discher DE. Embryonic cardiomyocytes beat best on a matrix with heart-like elasticity: scar-like rigidity inhibits beating. J Cell Sci. 2008;121(22):3794–802. https://doi.org/10.1242/jcs.029678.
Blakney AK, Swartzlander MD, Bryant SJ. Student award winner in the undergraduate category for the society of biomaterials 9th world biomaterials congress, Chengdu, China, June 1-5, 2012: the effects of substrate stiffness on the in vitro activation of macrophages and in vivo host response to poly(ethylene glycol)-based hydrogels. J Biomed Mater Res Part A. 2012;100 A(6):1375–86. https://doi.org/10.1002/jbm.a.34104.
Brown BN, Mani D, Nolfi AL, Liang R, Abramowitch SD, Moalli PA. Characterization of the host inflammatory response following implantation of prolapse mesh in rhesus macaque. Am J Obstet Gynecol. 2015;213(5):668e661–10. https://doi.org/10.1016/j.ajog.2015.08.002.
Shepherd JP, Feola AJ, Abramowitch SD, Moalli PA. Uniaxial biomechanical properties of seven different vaginally implanted meshes for pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2012;23(5):613–20.
Acknowledgements
The authors are grateful for the financial support provided the Department of Defense (DOD) (grant no. W81XWH-16-1-0133). The DOD did not provide any assistance with the study design, the collection, analysis and interpretation of data or in the writing of this report or in the decision to submit the article for publication. Research efforts for this publication was also supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award no. TL1TR001858. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors would also like to thank Dr. Naoki Yoshimura, MD PhD (Professor of Urology, Pharmacology, and Cell Biology, University of Pittsburgh), for allowing us to use the organ bath system to collect the contractility data reported, Dr. Leslie Meyn (Magee-Womens Research Institute) for statistical assistance, and Jannah Mujaahid for her assistance with animal care and imaging. The code used to image the picrosirius red images was written by Christopher A. Carruthers (PhD graduate of the University of Pittsburgh, Bioengineering Department).
Authors’ contributions
• KM Knight: Manuscript writing/editing, experimentation, data collection, and analysis, project development.
• GE King: Manuscript editing, experimentation, data collection, and analysis.
• SL Palcsey: Manuscript editing, experimentation.
• AM Artsen: Manuscript editing, experimentation.
• SD Abramowitch: Manuscript writing/editing, project/concept development.
• PA Moalli: Manuscript writing/editing, experimentation, project/concept development.
Funding
Financial support was provided by the Department of Defense (DOD) (W81XWH-16-1-0133) and the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH) (TL1 TR001858).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Conference presentation
American Urogynecology Society/International Urogynecological Association Joint Scientific Meeting, Nashville, Tennessee, September 24–28, 2019
Rights and permissions
About this article
Cite this article
Knight, K.M., King, G.E., Palcsey, S.L. et al. A soft elastomer alternative to polypropylene for pelvic organ prolapse repair: a preliminary study. Int Urogynecol J 33, 327–335 (2022). https://doi.org/10.1007/s00192-021-04792-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04792-0