Abstract
Introduction and hypothesis
The apical compartment is a keystone in POP treatment. Sacrospinous fixation, suggested half a century ago, today is still one of the most popular and efficient methods of colpo-hysteropexy. However, it has specific side effects: chronic pain syndrome, dyspareunia and а high rate of cystocele de novo. We aimed to evaluate the efficacy and safety of unilateral sacrospinous hysteropexy with a synthetic apical sling combined with anterior subfascial colporrhaphy.
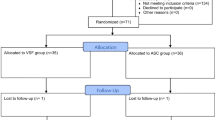
Methods
Following the suggested technique, 174 women with anterior-apical prolapse underwent surgery. The follow-up period took 12 months. Pre- and postoperative examination included: urogynecological examination (POP-Q), uroflowmetry, ultrasound of the bladder and filling in of validated questionnaires (PFDI-20, PISQ-12).
Results
The mean surgery time was 26 ± 7.84 min. No cases of damage of the bladder or rectum or of intraoperative clinically significant bleeding were noted. At the 12-month follow-up, the recurrence rate in the apical compartment was 0.7% (1/147) and in the anterior compartment 7.4% (11/147). The efficacy of the surgery reached 96.5%. During 12 months of follow-up, no cases of mesh exposure or chronic pelvic pain syndrome were detected. The incidence of dyspareunia de novo was observed in just one patient.
Conclusions
A unilateral sacrospinous fixation with a synthetic mesh (apical sling) combined with anterior subfascial colporrhaphy enhances the anatomical efficacy of surgery. It also helps to avoid specific side effects of traditional sacrospinous fixation.


Similar content being viewed by others
References
Hendrix SL, Clark A, Nygaard I, et al. Pelvic organ prolapse in the women’s health initiative: gravity and gravidity. Am J Obstet Gynecol. 2002;186:1160–6.
Brubaker L, Glazener C, Jacquetin B, Maher C, Melgrem A, Norton P, Rajamaheshwari N, Von Theobald P. (2009) Surgery for Pelvic Organ Prolapse// P. Abrams, L. Cordozo, S. Koury (Eds.) 4th International Consultation on Incontinence, Paris, ISBN: 0-9546956-8-2; Chapter 15:1278.
Forde J, Chughtai B, Stone B, Hsu W, Mao J, Te A, et al. Role of uterine preserving surgery in mesh based pelvic organ prolapse repair. Int Urogynecol J. 2017;28(8):1183–95. https://doi.org/10.1007/s00192-016-3244-9.
Maher C, Baessler K, Barber M, Cheon C, Consten E, Cooper K, et al. Surgery for pelvic organ prolapse. In: Abrams P, Cardozo L, Wagg A, Wein A, editors. Incontinence 6th edition. Bristol: ICI-ICS. International Continence Society; 2017. ISBN: 978-0956960733; Chapter 15:1855.
Hefni MA, EL–Toukhy TA. Long-term outcome of vaginal sacrospinous colpopexy for marked uterovaginal and vault prolapse. Eur J Obstet Gynecol Reprod Biol. 2006;127(2):257–63. https://doi.org/10.1016/j.ejogrb.2005.11.028.
Barber MD, Brubaker L, Burgio KL, Richter HE, Nygaard I, et al. Comparison of 2 transvaginal surgical approaches and perioperative behavioral therapy for apical vaginal prolapse: the optimal randomized trial. JAMA. 2014;311(10):1023–34. https://doi.org/10.1001/jama.2014.1719.
Maggiore LR, Alessandri F, Valentino R, Venturini PL, Ferrero S. Vaginal sacrospinous colpopexy using the Capio suture-capturing device versus traditional technique: feasibility and outcome. Arch Gynecol Obstet. 2013;287(2):267–74. https://doi.org/10.1007/s00404-012-2540-y.
Paraiso MFR, Ballard LA, Walters MD, Lee C, Mitchinson AR. Pelvic support defects and visceral and sexual function in women treated with sacrospinous ligament suspension and pelvic reconstruction. Obstet Gynecol. 1996;175(6):1423–31.
Sze EH, Karram MM. Transvaginal repair of vault prolapse: a review. Obstet Gynecol. 1997;89(3):466–75. https://doi.org/10.1016/S0029-7844(96)00337-7.
Unger CA, Walters MD. Gluteal and posterior thigh pain in the postoperative period and the need for intervention after sacrospinous ligament colpopexy. Female Pelvic Med Reconstr Surg. 2014;20(4):208–11. https://doi.org/10.1097/SPV.0000000000000091.
Shkarupa DD, Kubin ND, Shapovalova EA, Zajceva AO, Pisarev AV. The hybrid technique of pelvic organ prolapse treatment: apical sling and subfascial colporraphy. Int Urogynecol J. 2017;28(9):1407–13. https://doi.org/10.1007/s00192-017-3286-7.
Richardson DA, Scotti RJ, Ostergard DR. Surgical management of uterine prolapsed in young women. J Reprod Med. 1989;34(6):388–92.
Ghoniem G, Hammett J. Female pelvic medicine and reconstructive surgery practice patterns: IUGA member survey. Int Urogynecol J. 2015;26(10):1489–94. https://doi.org/10.1007/s00192-015-2734-5.
Slopnick EA, Petrikovets A, Sheyn D, Kim SP, Nguyn CT, et al. Surgical trends and patient factors associated with the treatment of apical pelvic organ prolapse from a national sample. Int Urogynecol J. 2018. https://doi.org/10.1007/s00192-018-3769-1.
Betschart C, Cervigni M, Contreras OO, Doumouchtsis SK, Koyama M, Medina C, et al. Management of apical compartment prolapse (uterine and vault prolapse): a FIGO working group report. Neurourol Urodyn. 2017;36(2):507–13. https://doi.org/10.1002/nau.22916.
Meriwether KV, Antosh DD, Olivera CK, Kim-Fine S, Balk EM, Murphy M, et al. Uterine preservation vs hysterectomy in pelvic organ prolapse surgery: a systematic review with meta-analysis and clinical practice guidelines. Am J Obstet Gynecol. 2018;219(2):129–146.e2. https://doi.org/10.1016/j.ajog.2018.01.018.
Kapoor S, Sivanesan K, Robertson JA, Veerasingham M, Kapoor V. Sacrospinous hysteropexy: review and meta-analysis of outcomes. Int Urogynecol J. 2017;28(9):1285–94. https://doi.org/10.1007/s00192-017-3291-x.
Tseng LH, Chen I, Chang SD, Lee CL. Modern role of sacrospinous ligament fixation for pelvic organ prolapse surgery—a systemic review. Taiwan J Obstet Gynecol. 2013;52(3):311–7. https://doi.org/10.1016/j.tjog.2012.11.002.
de Castro EB, Juliato CR, Piedemonte LA, dos Santos Junior LC. Impact of sacrospinous colpopexy associated with anterior colporrhaphy for the treatment of dome prolapse on all three vaginal compartments. Rev Bras Ginec Obst. 2016;38(2):77–81. https://doi.org/10.1055/s-0035-1571264.
Nager CW, Grimes CL, Nolen TL, Wai CY, Brubaker L, et al. Concomitant anterior repair, preoperative prolapse severity, and anatomic prolapse outcomes after vaginal apical procedures. Female Pelvic Med Reconstr Surg. 2019;25(1):22–8. https://doi.org/10.1097/SPV.0000000000000526.
Lo TS, Uy-Patrimonio MC, Hsieh WC, Yang JC, Huang SY, Chua S. Sacrospinous ligament fixation for hysteropexy: does concomitant anterior and posterior fixation improve surgical outcome? Int Urogynecol J. 2018;29(6):811–9. https://doi.org/10.1007/s00192-017-3487-0.
Beer M, Kuhn A. Surgical techniques for vault prolapse: a review of the literature. Eur J Obstet Gynecol Reprod Biol. 2005;119(2):144–55. https://doi.org/10.1016/j.ejogrb.2004.06.042.
Detollenaere RJ, den Boon J, Stekelenburg J, IntHout J, Vierhout ME, Kluivers KB, et al. Sacrospinous hysteropexy versus vaginal hysterectomy with suspension of the uterosacral ligaments in women with uterine prolapse stage 2 or higher: multicentre randomised non-inferiority trial. BMJ. 2015;351:h3717. https://doi.org/10.1136/bmj.h3717.
Mowat A, Wong V, Goh J, Krause H, Pelecanos A, Higgs P. A descriptive study on the efficacy and complications of the Capio (Boston Scientific) suturing device for sacrospinous ligament fixation. Aust N Z J Obstet Gynaecol. 2018;58(1):119–24. https://doi.org/10.1111/ajo.12720.
Baumann KM, Salvisberg C, Mueller M. Sexual function after sacrospinous fixation for vaginal vault prolapse: bad or mad. Surgical Endoscope. 2009;23(5):1013–7. https://doi.org/10.1007/s00464-008-0108-5.
Senturk MB, Guraslan H, Cakmak Y, Ekin M. Bilateral sacrospinous fixation without hysterectomy: 18-month follow-up. J Turk Ger Gynecol Assoc. 2015;16(2):102–6. https://doi.org/10.5152/jtgga.2015.15220.
Vu MK, Letko J, Jirschele K, Gafni-Kane A, Nguyen A, Du H, et al. Minimal mesh repair for apical and anterior prolapse: initial anatomical and subjective outcomes. Int Urogynecol J. 2012;23(12):1753–61. https://doi.org/10.1007/s00192-012-1780-5.
Jirschele K, Seitz M, Zhou Y, Rosenblatt P, Culligan P, Sand P. A multicenter, prospective trial to evaluate mesh – augmented sacrospinous hysteropexy for uterovaginal prolapse. Int Urogynecol J. 2015;26(5):743–8. https://doi.org/10.1007/s00192-014-2564-x.
Altman D, Mikkola TS, Bek KM, Rahkola-Soisalo P, Gunnarsson J, Engh ME, et al. Pelvic organ prolapse repair using the Uphold™ vaginal support system: a 1-year multicenter study. Int Urogynecol J. 2016;27(9):1337–45. https://doi.org/10.1007/s00192-016-2973-0.
Meriwether KV, Balk EM, Antosh DD, Olivera CK, Kim-Fine S, Murphy M, et al. Uterine-preserving surgeries for the repair of pelvic organ prolapse: a systematic review with meta-analysis and clinical practice guidelines. Int Urogynecol J. 2019. https://doi.org/10.1007/s00192-019-03876-2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial disclaimer/conflict of interest
D.D. Shkarupa and N.D. Kubin are consultants (LlcLintex); other authors claim no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shkarupa, D., Kubin, N., Shapovalova, E. et al. The resurrection of sacrospinous fixation: unilateral apical sling hysteropexy. Int Urogynecol J 31, 351–357 (2020). https://doi.org/10.1007/s00192-019-03964-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-03964-3