Abstract
Introduction and hypothesis
The aim of our study was to assess the interobserver and intraobserver reliability as well as the content and construct validity of the FIGO prolapse assessment scoring system (FASS).
Methods
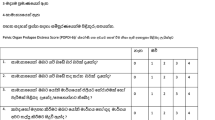
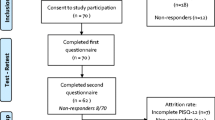
Women with and without (controls) symptoms of pelvic organ prolapse (POP) attending gynaecology outpatient clinics in four different countries were recruited prospectively. Each woman was assessed using the FASS which included: (1) physical examination findings designated with the letter P; (2) presence of symptoms of prolapse, urinary and bowel symptoms designated with the letter S; and (3) assessment of degree of bother designated with the letter B. A scoring system was also developed. For interobserver reliability women were examined by two separate examiners using the FASS. For intraobserver reliability the FASS was repeated by the same examiner within 2 weeks. The interclass correlation coefficient (ICC) was also calculated to assess limits of agreements. Validity was assessed by comparing the FASS scores between symptomatic and asymptomatic women using the Mann-Whitney U test (p value <0.001).
Results
A total of 177 women (98 symptomatic and 79 controls) were recruited. Intraobserver reliability had ICCs between 0.716 and 1. Interobserver reliability had ICCs between 0.795 and 0.909. Domain and total scores were significantly different between symptomatic and asymptomatic women (p < 0.001, Mann-Whitney U test). There was a good correlation between FASS P scores and POP-Q scores (rho 0.763, p < 0.001).
Conclusions
The FIGO prolapse assessment scoring system has good intraobserver and interobserver agreement and has demonstrated both content and construct validity.
Similar content being viewed by others
References
Bump RC, Mattiasson A, Bo K et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175(1):10–17
Hall AF, Theofrastous JP, Cundiff GC et al (1996) Interobserver and intraobserver reliability of the proposed International Continence Society, Society of Gynecologic Surgeons, and American Urogynecologic Society pelvic organ prolapse classification system. Am J Obstet Gynecol 175(6):1467–1471
Kobak WH, Rosenberger K, Walters MD (1996) Interobserver variation in the assessment of pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunc 7(3):121–124
Digesu GA, Athanasiou S, Cardozo L, Hill S, Khullar V (2009) Validation of the pelvic organ prolapse quantification (POP-Q) system in left lateral position. Int Urogynecol J Pelvic Floor Dysfunct 20(8):979–83. doi:10.1007/s00192-009-0884-z
Lemos NL, Auge AP, Lunardelli JL, Carramão Sda S, Faria AL, Aoki T (2008) Validation of the pelvic organ prolapse quantification index (POP-Q-I): a novel interpretation of the POP-Q system for optimization of POP research. Int Urogynecol J Pelvic Floor Dysfunct 19(7):995–997. doi:10.1007/s00192-007-0556-9
Muir TW, Stepp KJ, Barber MD (2003) Adoption of the pelvic organ prolapse quantification system in peer-reviewed literature. Am J Obstet Gynecol 189(6):1632–1635
Treszezamsky AD, Rascoff L, Shahryarinejad A, Vardy MD (2010) Use of pelvic organ prolapse staging systems in published articles of selected specialized journals. Int Urogyn J 21(3):359–363. doi:10.1007/s00192-009-1044-1
Auwad W, Freeman RM, Swift S (2004) Is the pelvic organ prolapse quantification system (POPQ) being used? A survey of members of the International Continence Society (ICS) and the American Urogynecologic Society (AUGS). Int Urogynecol J Pelvic Floor Dysfunct 15(5):324–7
Swift S, Morris S, McKinnie V et al (2006) Validation of a simplified technique for using the POPQ pelvic organ prolapse classification system. Int Urogynecol J Pelvic Floor Dysfunct 17(6):615–620
Lemos N, Korte JE, Iskander M et al (2012) Center-by-center results of a multicenter prospective trial to determine the inter-observer correlation of the simplified POP-Q in describing pelvic organ prolapse. Int Urogynecol J 23(5):579–584. doi:10.1007/s00192-011-1593-y
Steele A, Mallipeddi P, Welgoss J, Soled S, Kohli N, Karram M (1998) Teaching the pelvic organ prolapse quantitation system. Am J Obstet Gynecol 179(6):1458–63; discussion 1463–1464
Weber AM, Abrams P, Brubaker L et al (2001) The standardization of terminology for researchers in pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct 12(3):178–86
Slieker-ten Hove M, Pool-Goudzwaard A, Ejikemans M et al (2009) Symptomatic pelvic organ prolapse and possible risk factors in a general population. Am J Obstet Gynecol 200:184.e1–184.e7
Swift S, Woodman P, O’Boyle A et al (2005) Pelvic organ support study (POSST); the distribution, clinical definition and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol 192(3):795–806
Trowbridge ER, Fultz NH, Patel DA, DeLancey JO, Fenner DE (2008) Distribution of pelvic organ support measures in a population-based sample of middle-aged, community-dwelling African American and white women in southeastern Michigan. Am J Obstet Gynecol 198(5):548.e1–548.e6
Ellerkman RM, Cundiff GW, Melik CF, Nihira M, Leffler K, Bent AE (2001) Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol 185(6):1332–7; discussion 1337–1338
Haylen BT, de Ridder D, Freeman RM et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21(1):5–26
Brubaker L, Norton P (1996) Current clinical nomenclature for description of pelvic organ prolapse. J Pelvic Surg 2:257–9
Berger MB, Morgan DM, Delancey JO (2014) Levator ani defect scores and pelvic organ prolapse: is there a threshold effect? Int Urogynecol J 25(10):1375–1379
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Digesu, G.A., Swift, S., Puccini, F. et al. The FIGO assessment scoring system (FASS): a new holistic classification tool to assess women with pelvic floor dysfunction: validity and reliability. Int Urogynecol J 26, 859–864 (2015). https://doi.org/10.1007/s00192-014-2604-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2604-6