Abstract
Introduction and hypothesis
To test in vitro and in vivo the capability of mesh materials to act as scaffolds for rat-derived mesenchymal stem cells (rMSCs) and to compare inflammatory response and collagen characteristics of implant materials, either seeded or not with rMSCs.
Methods
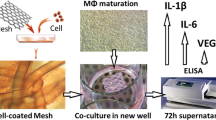
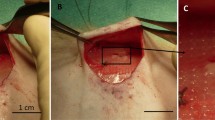
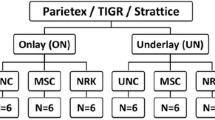
rMSCs isolated from rat bone marrow were seeded and cultured in vitro on four different implant materials. Implants showing the best rMSC proliferation rate were selected for the in vivo experiment. Forty-eight adult female Sprague–Dawley rats were randomly divided into two treatment groups. The implant of interest—either seeded or not with rMSCs—was laid and fixed over the muscular abdominal wall. Main outcome measures were: in vitro, proliferation of rMSCs on selected materials; in vivo, the occurrence of topical complications, the evaluation of systemic and local inflammatory response and examination of the biomechanical properties of explants.
Results
Surgisis and Pelvitex displayed the best cell growth in vitro. At 90 days in the rat model, rMSCs were related to a lower count of neutrophil cells for Pelvitex and a greater organisation and collagen amount for Surgisis. At 7 days Surgisis samples seeded with rMSCs displayed higher breaking force and stiffness.
Conclusions
The presence of rMSCs reduced the systemic inflammatory response on synthetic implants and improved collagen characteristics at the interface between biological grafts and native tissues. rMSCs enhanced the stripping force on biological explants.


Similar content being viewed by others
Abbreviations
- Fmax :
-
Maximum force before the separation of the mesh from the abdominal wall
- FBGC:
-
Foreign body giant cells
- H&E:
-
Haematoxylin/eosin
- MSCs:
-
Mesenchymal stem cells
- PMN:
-
Polymorphonuclear cells
- PN:
-
Pelvitex without rMSCs
- POP:
-
Pelvic organ prolapse
- PP:
-
Polypropylene
- PS:
-
Pelvitex with rMSCs
- rMSCs:
-
Rat-derived mesenchymal stem cells
- S:
-
Stiffness
- S30%:
-
Secant modulus at 30 % elongation
- S50%:
-
Secant modulus at 50 % elongation
- SIS:
-
Small intestine submucosa
- SN:
-
Small intestine submucosa without rMSCs
- SS:
-
Small intestine submucosa with rMSCs
- Δlmax :
-
Maximum elongation before the separation of the mesh from the abdominal wall
References
MacLennan AH, Taylor AW, Wilson DH, Wilson D (2000) The prevalence of pelvic floor disorders and their relation to gender, age, parity, and mode of delivery. Br J Obstet Gynaecol 106:1460–1470
Birch C, Fynes MM (2002) The role of synthetic and biological prostheses in reconstructive pelvic floor surgery. Curr Opin Gynecol Obstet 14:527–535
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Baessler K, Maher CF (2006) Mesh augmentation during pelvic-floor reconstructive surgery: risks and benefits. Curr Opin Obstet Gynecol 18:560–566
Cobb WS, Kercher KW, Heniford BT (2005) The argument for lightweight polypropylene mesh in hernia repair. Surg Innov 12(1):63–69, review
Deprest J, Claerhout F, Zheng F, Kostantinovic M, Spelzini F, Guelinckx I et al (2005) Synthetic and biodegradable prostheses in pelvic floor surgery. Int Congr Ser 1279:387–397
Nazemi TM, Kobashi KC (2007) Complications of grafts used in female pelvic floor reconstruction: mesh erosion and extrusion. Indian J Urol 23:153–160
Fibbe WE. Mesenchymal stem cells. A potential source for skeletal repair. Ann Rheum Dis 2002;61 [Suppl II]:ii29–ii31.
Caplan AI (2007) Adult mesenchymal stem cells for tissue engineering versus regenerative medicine. J Cell Physiol 213(2):341–347
Meinel L, Karageorgiou V, Fajardo R, Snyder B, Shinde-Patil V, Zichner L et al (2004) Bone tissue engineering using human mesenchymal stem cells: effects of scaffold material and medium flow. Ann Biomed Eng 32:112–122
Rasmusson I (2006) Immune modulation by mesenchymal stem cells. Exp Cell Res 312:2169–2179
Ochoa I, Peña E, Andreu EJ, Pérez-Ilzarbe M, Robles JE, Alcaine C et al (2011) Mechanical properties of cross-linked collagen meshes after human adipose derived stromal cells seeding. J Biomed Mater Res A 96(2):341–348
Voytik-Harbin SL, Brightman AO, Kraine MR, Waisner B, Badylak SF (1997) Identification of extractable growth factors from small intestinal submucosa. J Cell Biochem 67:478–491
Gandhi S, Kubba LM, Abramov Y, Botros SM, Goldberg RP, Victor TA et al (2005) Histopathologic changes of porcine dermis xenografts for transvaginal suburethral slings. Am J Obstet Gynecol 192:1643–1648
De Tayrac R, Alves A, Therin M (2007) Collagen-coated vs noncoated low-weight polypropylene meshes in a sheep model for vaginal surgery. A pilot study. Int Urogynecol J 18:513–520
Mutter D, Jamali FR, Moody DL, Rodeheaver GT, Therin M, Marescu J (2000) The concept of protected mesh to minimize adhesion formation in intraperitoneal abdominal wall reinforcement. preclinical evaluation of a new composite mesh. Hernia 4 [Suppl]:S3–S9
Donzelli E, Salvadè A, Mimo P, Viganò M, Morrone M, Papagna R et al (2007) Mesenchymal stem cells cultured on a collagen scaffold: in vitro osteogenic differentiation. Arch Oral Biol 52(1):64–73
Badylak S, Kokini K, Tullius B, Simmons-Byrd A, Morff R (2002) Morphologic study of small intestinal submucosa as a body wall repair device. J Surg Res 103(2):190–202
Konstantinovic ML, Lagae P, Zheng F, Verbeken KE, De Ridder D, Deprest JA (2005) Comparison of host response to polypropylene and non-cross-linked porcine small intestine serosal-derived collagen implants in a rat model. BJOG 112:1554–1560
Morishita T, Honoki K, Ohgushi H, Kotobuki N, Matsushima A, Takakura Y (2006) Tissue engineering approach to the treatment of bone tumors: three cases of cultured bone grafts derived from patients’ mesenchymal stem cells. Artif Organs 30(2):115–118
Janssens S, Dubois C, Bogaert J, Theunissen K, Deroose C, Desmet W et al (2006) Autologous bone marrow-derived stem-cell transfer in patients with ST-segment elevation myocardial infarction: double-blind, randomised controlled trial. Lancet 367:113–121
Yamamoto T, Gotoh M, Kato M, Majima T, Toriyama K, Kamei Y et al (2012) Periurethral injection of autologous adipose-derived regenerative cells for the treatment of male stress urinary incontinence: report of three initial cases. Int J Urol 19(7):652–659
Ahn HH, Kim KS, Lee JH, Lee MS, Song IB, Cho MH et al (2007) Porcine small intestinal submucosa sheets as a scaffold for human bone marrow stem cells. Int J Biol Macromol 41(5):590–596
Klosterhalfen B, Klinge U, Schumpelick V (1998) Functional and morphological evaluation of different polypropylene-mesh modifications for abdominal wall repair. Biomaterials 19:2235–2246
Dolce CJ, Stefanidis D, Keller JE, Walters KC, Newcomb WL, Heath JJ et al (2010) Pushing the envelope in biomaterial research: initial results of prosthetic coating with stem cells in a rat model. Surg Endoscop 24(11):2687–2693
Altman AM, Abdul Khalek FJ, Alt EU, Butler CE (2010) Adipose tissue– derived stem cells enhance Bioprosthetic mesh repair of ventral hernias. Plast Reconstr Surg 126(3):845–854
Mouritsen L, Kronschnabl M, Lose G (2010) Long-term results of vaginal repairs with and without xenograft reinforcement. Int Urogynecol J Pelvic Floor Dysfunct 21:467–473
Ozog Y, Konstantinovic ML, Verschueren S, Spelzini F, De RD, Deprest J (2009) Experimental comparison of abdominal wall repair using different methods of enhancement by small intestinal submucosa graft. Int Urogynecol J Pelvic Floor Dysfunct 20:435–441
Boennelycke M, Gras S, Lose G (2013) Tissue engineering as a potential alternative or adjunct to surgical reconstruction in treating pelvic organ prolapse. Int Urogynecol J 24:741–747
Urogynecologic surgical mesh: update on the safety and effectiveness of transvaginal placement for pelvic organ prolapse. July 2011 http://www.fda.gov/downloads/MedicalDevices/Safety/AlertsandNotices/UCM262760.pdf
Hilger WS, Walter A, Zobit ME, Leslie KO, Magtibay P, Cornella J (2006) Histological and biomechanical evaluation of implanted graft materials in a rabbit vaginal and abdominal model. Am J Obstet Gynecol 195(6):1826–1831
Manodoro S, Endo M, Uvin P, Albersen M, Vlacil J, Engels A et al (2013) Graft-related complications and biaxial tensiometry following experimental vaginal implantation of flat mesh of variable dimensions. BJOG 120:244–250
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spelzini, F., Manodoro, S., Frigerio, M. et al. Stem cell augmented mesh materials: an in vitro and in vivo study. Int Urogynecol J 26, 675–683 (2015). https://doi.org/10.1007/s00192-014-2570-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2570-z