Abstract
Introduction and hypothesis
Perineorrhaphy (Pe) has not been subject to a comprehensive perioperative quantitative assessment (QA). We wish to nominate such an assessment (Pe-QA) for any Pe, through testing the QA on the excision of the perineal gap (PG) at the time of posterior repair (PR).
Methods
At 50 consecutive PRs, the following measurements were taken pre- and postoperatively: (i) perineorrhaphy width (PW) equals PG [1]; (ii) perineorrhaphy depth (PD); (iii) perineal length (PL); (iv) midperineal thickness (MPT); (v) genital hiatus (GH) and (vi) total posterior vaginal length (TPVL). The total vaginal length was also measured. Surgical details deemed appropriate to each repair were recorded.
Results
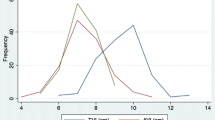
The overall means and ranges (cm) were: (i) PW 2.9 (1.5–5.5); (ii) PD 1.6 (0.8–2.0); (iii) PL 2.9 (1.5–4.5); (iv) MPT 0.7 (0.4–1.1); (v) GH 3.9 (2.3–6.5); (vi) TPVL 9.2 (6.0–12.5). Excision of PG (100 % cases reducing PW and PD to zero) resulted in a mean 23.6 % increase in total vaginal length over that if the repair was commenced at the hymen, despite a 3.3 % decrease in the TPVL perioperatively. There was a mean 30.8 % reduction in the GH, a mean 27.6 % increase in the PL and a mean 57.1 % increase in the MPT.
Conclusions
Pe and the anatomical results of such surgery can be subject to quantitative assessment allowing comparison studies between different forms of Pe and possibly other types of perineal surgeries.




Similar content being viewed by others
References
Haylen BT, Avery D, Chiu TL, Birrell W (2014) Posterior repair quantification (PR-Q) using key anatomical indicators (KAI) – Preliminary Report. International Urogynecological Journal. Published online May: DOI: 10.007/s00192-014-2433-7
DeLancey JOL (1992) Anatomic aspects of vaginal eversion after hysterectomy. Amer J Obstet Gynecol 166:1717–1728
Dua A, Whitworth M, Hill S (2008) Perineal length: Relationship between the length of the perineum and ethnic origin. Abstracts International Continence Society Cairo. October. www.ics.org/Abstracts/Publish/46/000161.pdf
Bump RC, Mattiasson A, Bo K, Brubaker LP et al (1996) The standardization of female pelvic organ prolapse and pelvic floor dysfunction. Amer J Obstet Gynecol 175(1):10–11
Yang A, Mostwin J, Genadry R, Sanders R (1993) Patterns of prolapse demonstrated with dynamic fastscan MRI; reassessment of conventional concepts of pelvic floor weaknesses. Neurourol Urodyn 12(4):310–311
Fowler GE, Richmond DH (2011) Operations for pelvic organ prolapse. In: Lopes T, Spirtos NM, Naik R, Monaghan JM Bonney’s Gynaecological Surgery. 11th Edition. Wiley-Blackwell London. Chapter 16. P154
Nichols DH, Randall CL (1996) Posterior colporrhaphy and perineorrhaphy. In Nichols DH, Randall CL Vaginal Surgery 4th Edition. Williams & Wilkins. Baltimore. Chapter 11 p279
Haylen BT, Freeman RM, de Ridder D, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk D, Sand P, Schaer G (2010) An International Urogynecological Association (IUGA) – International Continence Society (ICS) Joint Report into the Terminology for Female Pelvic Floor Dysfunction. Neurourology & Urodynamics, 29:4–20. International Urogynecology J 21:5–26
Blomquist JL, Cundiff GW (2008) Posterior support defects. In Bent AE, Cundiff GW, Swift SE. Ostergard’s Urogynecology and Pelvic Floor Dysfunction. Lippincott, Williams & Wilkins. Philadelphia. Chapter 30. P500
Pancholy AB, Silva WA, Karram MM (2010) Rectocele- Anatomic and Functional Repair. In: Cardozo L, Staskin D. Textbook of Female Urology and Urogynecology. Informa. London. Chapter 78. P804-806
Shakif A (2005) Surgical anatomy of the perineal muscles and their role in perineal disoders. Anatom Sci Intern 80(3):161–171
Shakif A (2005) Perineal rectocele: A common cause of constipation – pathogenesis, clinical presentation and treatment. J Pelv Med Surg 11(4):199–207
Ghetti C, Grerory WT, Edwards SR, Otto LN, Clark AL (2005) Severity of pelvic organ prolapse associated with measurements of pelvic floor function. Int Urogynecol J 16:432–436
Wagenlehner FME, Del Amo E, Santoro GA, Petros P (2013) Live anatomy of the perineal body in patients with third-degree rectocoele. Color Dis 15(11):1416–1422
Kalis V, Chaloupka P, Turek J, Rokyta Z (2005) The perineal body length and injury at delivery Ceska Gynekol 70(5):355–361
Tsai PJS, Oyama IA, Hiraoka M, Minaglia S, Thomas J, Kanesshiro B (2012) Perineal body length among different racial groups in the first stage of labor. Fem Pelv Med Reconstruct Surg 18(3):165–167
Lloyd J, Crouch NS, Minto CL, Liao LM, Creighton S (2005) Female genital appearance: “normality” unfolds. BJOG 112:643–646
Clark AL, Gregory WT, Smith VJ, Edwards R (2003) Epidemiologic evaluation of re-operation for surgically treated pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol 189(5):1261–1267
Soligo M (2007) Pasterior pelvic floor dysfunction: there is an immediate need to standardize terminology. Int Urogynecol J 18:369–371
Karram MM, Maher C (2013) Surgery for posterior vaginal wall prolapse. Int Urogynecol J 24:1835–1841
Lewicky-Gaupp C, Yousuf A, Larson KA, Fenner DE, DeLancey JOL (2010) Structural position of the posterior vagina and pelvic floor in women with and without posterior vaginal prolapse. Am J Obstet Gynecol 202(5):497
Francis WFA, Jeffcoate TNA (1961) Dyspareunia following vaginal operations. J Obstet Gynaecol Br Commonw 68:1–10
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haylen, B.T., Younis, M., Naidoo, S. et al. Perineorrhaphy quantitative assessment (Pe-QA). Int Urogynecol J 26, 539–544 (2015). https://doi.org/10.1007/s00192-014-2528-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2528-1