Abstract
Introduction and hypothesis
This study was conducted to assess time-to-effect with darifenacin in patients with overactive bladder (OAB).
Methods
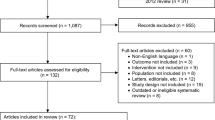
Efficacy and safety data were pooled from 1,059 patients (19–88 years, 85% women) randomized to darifenacin 7.5 or 15 mg once daily or matched placebo in three double-blind 12-week studies. Patients completed electronic bladder symptom diaries (number of micturitions/day; incontinence episodes/day; urgency episodes/day). A post hoc efficacy analysis was performed on the earliest recorded timepoints.
Results
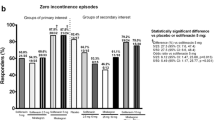
The full analysis population comprised 1,053 patients. Statistically significant improvements were observed in all OAB symptoms (except nocturnal awakenings) for both darifenacin doses versus placebo at week 2, with further improvements over 6 and 12 weeks. Both darifenacin doses significantly improved all OAB symptoms from as early as days 6–8 versus placebo.
Conclusions
Darifenacin 7.5 and 15 mg significantly reduced OAB symptoms throughout the study. The rapid onset-of-effect is desirable to patients with OAB and useful for their clinical management.



Similar content being viewed by others
References
Haylen BT, De Ridder D, Freeman RM et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J Pelvic Floor Dysfunct 21:5–26
Abrams P, Cardozo L, Fall M et al (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21:167–178
Irwin DE, Milsom I, Kopp Z, Abrams P, Cardozo L (2006) Impact of overactive bladder symptoms on employment, social interactions and emotional well-being in six European countries. BJU Int 97:96–100
Coyne KS, Sexton CC, Irwin DE, Kopp ZS, Kelleher CJ, Milsom I (2008) The impact of overactive bladder, incontinence and other lower urinary tract symptoms on quality of life, work productivity, sexuality and emotional well-being in men and women: results from the EPIC study. BJU Int 101:1388–1395
Brown JS, Vittinghoff E, Wyman JF et al (2000) Urinary incontinence: does it increase risk for falls and fractures. J Am Geriatr Soc 48:721–725
Gray M (2007) Incontinence-related skin damage: essential knowledge. Ostomy Wound Manage 53:28–32
Stewart WF, Van Rooyen JB, Cundiff GW et al (2003) Prevalence and burden of overactive bladder in the United States. World J Urol 20:327–336
Vigod SN, Stewart DE (2006) Major depression in female urinary incontinence. Psychosomatics 47:147–151
Irwin DE, Mungapen L, Milsom I, Kopp Z, Reeves P, Kelleher C (2009) The economic impact of overactive bladder syndrome in six Western countries. BJU Int 103:202–209
Ganz ML, Smalarz AM, Krupski TL et al (2010) Economic costs of overactive bladder in the United States. Urology 75:526–532
Irwin DE, Milsom I, Hunskaar S et al (2006) Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 50:1306–1314
Onukwugha E, Zuckerman IH, McNally D, Coyne KS, Vats V, Mullins CD (2009) The total economic burden of overactive bladder in the United States: a disease-specific approach. Am J Manag Care 15:S90–S97
Helfand BT, Evans RM, McVary KT (2010) A comparison of the frequencies of medical therapies for overactive bladder in men and women: analysis of more than 7.2 million aging patients. Eur Urol 57:586–591
Andersson KE (2004) Antimuscarinics for treatment of overactive bladder. Lancet Neurol 3:46–53
Cardozo L, Hessdorfer E, Milani R et al (2008) Solifenacin in the treatment of urgency and other symptoms of overactive bladder: results from a randomized, double-blind, placebo-controlled, rising-dose trial. BJU Int 102:1120–1127
Rudy D, Cline K, Harris R, Goldberg K, Dmochowski R (2006) Time to onset of improvement in symptoms of overactive bladder using antimuscarinic treatment. BJU Int 97:540–546
Sussman DO, Kraus SR, Carlsson M, Guan Z (2007) Onset of efficacy of tolterodine extended release in patients with overactive bladder. Curr Med Res Opin 23:777–781
Rudy D, Cline K, Harris R, Goldberg K, Dmochowski R (2006) Multicenter phase III trial studying trospium chloride in patients with overactive bladder. Urology 67:275–280
Chapple CR, Steers W, Norton P et al (2005) A pooled analysis of three phase III studies to investigate the efficacy, tolerability and safety of darifenacin, a muscarinic M3 selective receptor antagonist, in the treatment of overactive bladder. BJU Int 95:993–1001
Steers W, Corcos J, Foote J, Kralidis G (2005) An investigation of dose titration with darifenacin, an M3-selective receptor antagonist. BJU Int 95:580–586
Haab F, Corcos J, Siami P et al (2006) Long-term treatment with darifenacin for overactive bladder: results of a 2-year, open-label extension study. BJU Int 98:1025–1032
Kelleher CJ (2002) Economic and social impact of OAB. Eur Urol 46:11–16
Abrams P, Kelleher C, Huels J, Quebe-Fehling E, Omar MA, Steel M (2008) Clinical relevance of health-related quality of life outcomes with darifenacin. BJU Int 102:208–213
Campbell JC, Gries KS, Watanabe JH, Ravelo A, Dmochowski R, Sullivan SD (2010) Treatment success for overactive bladder with urinary urge incontinence refractory to oral antimuscarinics: a review of published evidence. BMC Urol 20(18):9
Schabert VF, Bavendam T, Goldberg EL, Trocio JN, Brubaker L (2009) Challenges for managing overactive bladder and guidance for patient support. Am J Manag Care 15:S118–S122
Benner JS, Nichol MB, Rovner ES et al (2010) Patient-reported reasons for discontinuing overactive bladder medication. BJU Int 105:1276–1282
Basra RK, Wagg A, Chapple C et al (2008) A review of adherence to drug therapy in patients with overactive bladder. BJU Int 102:774–779
Yeaw J, Benner JS, Walt JG, Sian S, Smith DB (2009) Comparing adherence and persistence across 6 chronic medication classes. J Manag Care Pharm 15:728–740
Chapple CR, Khullar V, Gabriel Z, Muston D, Bitoun CE, Weinstein DA (2008) The effects of antimuscarinic treatments in overactive bladder: an update of a systematic review and meta-analysis. Eur Urol 54:543–562
van Leeuwen JH, Castro R, Busse M, Bemelmans BL (2006) The placebo effect in the pharmacologic treatment of patients with lower urinary tract symptoms. Eur Urol 50:440–452
Acknowledgments
Funding for editorial support, drafting and revising the manuscript, and for the analysis was provided by Novartis Pharma AG. The authors would like to thank Andrea Larson-Peters (Section Head at Procter & Gamble and previous employee of Warner Chilcott Pharmaceuticals Inc.) for her input into project development, data analysis, and manuscript writing/editing; Karen Boyle (Senior Biostatistician with Rho) for her input into data analysis; and Claire Chinn (professional medical writer with ACUMED®) for her assistance in drafting and revising this manuscript.
Conflicts of interest
V. Khullar is a Consultant to Novartis and a past study investigator, J. Foote has received honoraria from Novartis, Y. Seifu is an employee of Novartis, and M. Egermark is a stockholder and previous employee of Novartis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khullar, V., Foote, J., Seifu, Y. et al. Time-to-effect with darifenacin in overactive bladder: a pooled analysis. Int Urogynecol J 22, 1573–1580 (2011). https://doi.org/10.1007/s00192-011-1522-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-011-1522-0