Abstract
Purpose
In up to a fifth of total knee replacements (TKR), surgeons are not capable of achieving good clinical and functional results. Despite comprehensive diagnostic workup, an underlying cause is not always identified in these patients. The purpose of this study is to compare native and prosthetic trochlear anatomies, to evaluate a potential source of morphologic mismatch and theoretically, of poor clinical outcomes.
Methods
Native trochlear angles of 4116 knee CTs from 360 Knee Systems database of arthritic pre-operative TKR patients were evaluated. A semi-automated tridimensional analysis was performed to define the native trochlear angle in the coronal plane (NTA) among other 142 parameters. An active search was conducted to identify currently available TKR models; prosthetic trochlear orientation in the coronal plane (PTA) was extracted from the technical data provided by manufacturers.
Results
The mean native trochlear angle (NTA) was 1.6° ± 6.6° (valgus) with a range from − 23.8° (varus) to 30.3°(valgus). A valgus NTA was present in 60.6% of the knees and 39.4% of them had a varus NTA. 89 TKR models were identified; trochlear details were available for 45 of them, of which 93% were designed with a valgus orientation of the prosthetic trochlear angle (PTA) and 6.9% showed a neutral (0°) PTA. Varus alignment of PTA was not present in any system. Angular numeric values for PTA were available for 34 models; these ranged from 0° to 15° of valgus, with a median value of 6.18° (SD ± 2.88°).
Conclusion
This study shows a significant mismatch between native and prosthetic trochlear angles. A relevant proportion of the studied knees (41.45%) fall out of the trochlear angle range of currently available implants; representing a potential source for biomechanical imbalance. While further research is warranted to fully understand the clinical implications of the present study, manufacturers may need to take these findings into account for future implant designs.
Level of evidence
Level III, retrospective cohort study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Up to 20% of patients with a total knee replacement (TKR) report poor clinical outcomes [15]. Major complications are associated with suboptimal results [18]; implant malpositioning can also be a determinant factor for chronic pain and dysfunction, too [21]. Under this premise, several alignment philosophies have appeared in the last decades, but to date none of them have proved superior [4].
Moreover, patellofemoral complications are present in up to a fifth of TKRs, with underlying causes frequently remaining unidentified [24]. Initial TKR designs in the 1970s completely neglected the patellofemoral joint (PFJ) [27]; the ideal configuration of the patellofemoral component is still under debate today. It has been assumed that despite state-of-the-art procedures, patellofemoral complications will remain noticeable due to inherent limitations of available implants [5], which have shown significant tridimensional discrepancies with native trochleae [6].
TKR procedures tend to be more and more personalized [19], even though implants are mass-produced to fit average anthropometric measurements. Concerns have been raised about what should be considered as ´normal´, and whether off-the-shelf implants can be applied universally to all patients and surgical techniques: a large anatomical study showed wide variability in several tibio-femoral parameters, with a relevant proportion of arthritic knees presenting with varus-aligned trochleae [10]. As the design of the femoral groove is considered the main determinant of prosthetic patellofemoral tracking [17] and the effect of implant coronal alignment is known to have an impact on patellar loading [29]; might this native/prosthetic mismatch be one of those unidentified causes of dissatisfaction in TKR?
This piece of research has been designed to compare the trochlear coronal alignment of arthritic knees to that of currently universally available TKR models, analyzing a potential source for PFJ imbalance and subsequent poor clinical results. The authors hypothesize wide discrepancies between native and prosthetic trochleae, which may alter patellofemoral tracking and increase patellar loading of replaced knees: the clinical implication of this presumption may affect current knee replacements worldwide.
Methods
Data extraction
Native femoral anatomy
Four thousand one hundred and sixteen pre-operative knee 3DCTs (3-dimensional computed tomography) were retrospectively extracted from the 360 Knee Systems Database (Bellberry Human Research Ethics Committee, approval number 2012-03-710; Bellberry Ltd, 123 Glen Osmond Road Eastwood SA 5063 Australia). This cohort represented the entire database from January 2014 until April 2020. Participants were patients with end-stage arthritis recruited from the general Australian population, determined eligible for a primary TKR by one of the Australian 360 Knee Group surgeons. 3DCT capture and analysis was performed by 360 Knee Systems (Pymble, NSW, Australia) with the purpose of generating pre-operative dynamic knee simulation reports that are commercially available from the company. Table 1 summarizes the general characteristics of the sample.
Detailed 3D models were generated from CT imaging according to a standardized protocol: 3D-reconstructed femur and tibia bones are generated through semi-automated segmentation, and are used to landmark and identify points of interest by biomedical engineers using the ScanIP software (Simpleware, Exeter, UK). Bones are converted to stereolithography files and landmarked independently by two engineers. If any parameter differs by a threshold value, a third engineer reviews the sample. This measurement protocol showed ICC values above 0.9 in all landmarks included in a previous study, meaning excellent reliability. Maximal distance and angular measurement accuracy errors have been quantified as 0.5 mm and 0.9°, respectively [30].
For every patient, 143 morphological features were obtained. In relation to the trochlear anatomy, one measurement was taken in considerations for the purpose of the present study:
Native trochlear angle to distal femoral angle (NTA): the line formed by a line of best fit of the deepest valley of the trochlea sulcus to a line drawn tangential to the distal femur (Fig. 1). NTA is measured relative to the femoral coronal plane and rotationally to the anatomical transepicondylar axis.
Prosthetic implants
The first author (SB) conducted an active search to identify current commercially available implants for primary TKR, as of September 2022. Dedicated orthopedic publications, forums and websites, online ordering catalogues and domains from specific commercial manufacturers and distributors were examined for potential references. A list of implants was defined, including all bicondylar models found, regardless of their material, fixation technique (cemented or not) and bearing system (cruciate retaining/sacrificing, posterior stabilized, medial pivot, fixed/mobile, etc.).
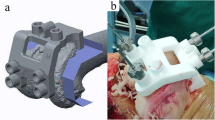
To obtain specific design features of femoral components, written details were acquired directly from manufacturing companies or licensed distributors. These were extracted from technical data available in the company’s websites/catalogues, or by means of direct request to their technical/scientific departments (Fig. 2). Overall orientation (valgus, varus, or neutral) in relation to the component coronal plane (i.e., perpendicular to the joint line/distal condylar angle) and numeric value of the prosthetic trochlear angle were recorded when available.
Prosthetic trochlear angle (PTA): defined as the angle resulting from bisecting the prosthetic distal condylar line and the trochlear sulcus direction in the coronal plane (Fig. 3).
Data analysis
Statistical analysis was performed in IBM SPSS Statistics 27 (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp). The Kolmogorov–Smirnov test was employed to determine sample normality. The Mann–Whitney U test was selected to compare sample means (nonparametric). Categorical variables were summarized using percentages and relative frequencies. Numerical variables were summarized by the mean ± standard deviation (SD).
Results
Native trochlear anatomy
The mean NTA was 1.6° ± 6.6° (valgus) with a range of values from − 23.8° (varus) to 30.3°(valgus). NTA normal distribution resulted in 60.6% of the knees showing a valgus alignment, while 39.4% of the knees showed varus values (Table 2). Among the 4116 knees, 220 specimens (5.3%) had a ‘virtually neutral’ NTA, i.e., an angulation between 0.5° of varus and 0.5° of valgus.
Prosthetic trochlear anatomy
For primary knee replacement, 89 available bicondylar implants were identified. These correspond to 60 manufacturers from 17 countries in Europe, North and South America, Asia, and Oceania. Trochlear design data were available for 45 brands (50.5% of the identified models) (Table 3).
From this list of 45 designs, a majority (91.1%) showed a valgus orientation of the PTA, while four implants (8.9%) were designed with a neutral (0°) PTA. PTA varus alignment was not present in any system. Angular numeric values for PTA were available for 34 models, including the 10 most implanted TKR models in Australia in the 2014–2021 period, accounting for the 67.2% of TKRs implanted nationwide [1]. These ranged from 0° to 15° (neutral to valgus), with a mean value of 6.18° (Table 2).
Discussion
The main finding of this study is that trochlear coronal alignment of arthritic knees and that of current TKR implants differ significantly (Table 2). According to the analysis, only 58.55% of knees in the sample would fall in a matched PTA-NTA range if all the studied models were available for implantation, using the mechanical alignment technique (Fig. 4). With a non-mechanical technique, the PTA-NTA would further change; typically, positioning the femoral component in valgus will orientate the prosthetic trochlea in varus (and vice versa), increasing the NTA–PTA discrepancy (as 60.6% of knees have a valgus NTA). It is noteworthy that two-thirds of all primary knee prostheses implanted in Australia in 2014–2021 have been included in this analysis [1], which emphasizes the potential significance of this mismatch in the clinical scenario.
Dejour et al. conducted a morphologic analysis of trochlear design in 14 TKR models available in 2014, with similar results. All trochleae were valgus-oriented (mostly in the 5°–8° range) except for one, which was neutral [5]. Therefore, at least in regards to trochlear coronal orientation, there has been little evolution during the last decade. The trochlear design of current TKR models is based on the assumption that most native knees present a valgus trochlea [2]; this concurs with the present results showing a mean PTA of 6.18° of valgus. However, the analysis also suggests that NTA range is more varus (or less valgus) than it has been generally considered [10].
There are a handful of previous reports rejecting valgus alignment as the natural conformation of the femoral trochlea. Ekhoff et al. and Koh et al. described a neutral orientation of the femoral trochlea, with means of 0.4° ± 5° and − 0.1° ± 9°, respectively [8] [16]. The cadaveric study by Barik et al. revealed an average varus orientation (1.8° ± 2.1°) of the femoral groove [3], while Grassi et al. also encountered 20% of varus-aligned trochleae in a navigation study with 110 arthritic knees [9]. In the present sample, which is by far the largest published, the mean value was valgus (1.6° ± 6.6°), but 39.4% of knees had a varus-oriented trochlea. Therefore, the consideration of a laterally oriented femoral trochlea as a standard feature of the femoral component should be approached with caution. High variability has been observed in the axial plane morphology of arthritic trochleae, too [12].
Riviere et al. reported a high degree of discrepancy between native and prosthetic trochlear alignment in kinematically aligned TKR, with a more valgus orientation of the latter [25]. In additional studies, this discrepancy was also shown for mechanical alignment [13, 26]; this could be interpreted as an inherent limitation of implant designs. Barink has already proposed a more truly anatomical femoral configuration, with a more medially oriented trochlea [2]. In fact, one of the implants with a neutral (0°) PTA showed good patellofemoral performance, with just 5.6% of residual anterior knee pain in a cohort of 1482 TKRs [7]. In addition, according to manufacturers, several models have a ‘widened trochlear angle’, in theory enabling the accommodation of a range of NTAs within a limited extent. Further analysis is warranted to determine the biomechanical and clinical impact of this concept. Besides that, the inception of patient-specific implants may represent a genuine solution to accommodate the wide variability of trochlear [20] and other knee parameters [22]. Longer follow-ups are required to evaluate clinical superiority [31], and a significant reduction in current costs is also required to permit more widespread use. Ultimately, manufacturing companies may need to take this wide variability into account, finding ways to accommodate outlying anatomies, and probably, offering a wider range of prosthetic trochlear orientations.
Positioning of the femoral component with a mild external rotation (3° according to Insall) has been a general recommendation to favor adequate patellar tracking in TKR [23]. However, a previous publication revealed that native trochleae were internally rotated in 27.1% of the cases [10]: external rotation of the femoral implant may exaggerate the NTA–PTA discrepancy. Moreover, it has been analyzed how femoral component rotation critically affects tibial rotation, ligament forces, retropatellar stress, and varus–valgus position [32], highlighting the narrow margin a surgeon has for balancing patellar tracking only by adjusting this parameter.
The results of this study suggest the NTA–PTA mismatch as a feasible cause for biomechanical imbalance and dysfunction. Hochereiter et al. concluded that “any valgisation in TKA will increase (…) lateral PFJ contact pressure” [11]; the present article highlights that PTA is indeed more valgus than native values. This mismatch can be only identified preoperatively by means of 3D CT analysis, allowing surgeons to anticipate a surgical planning to accommodate wide discrepancies. Navigation can also be of extreme usefulness, even if 3D CT is lacking. However, these routines are still not a standard procedure in many settings; a 2021 review revealed that the proportion of navigated TKR was only 32% in Australia (2019), 30% in Germany (2014), 6.3% in USA (2014), and 3% in the UK (2014) [28]; not to mention less wealthy regions. In consequence, substantial variations in NTA may be left unappreciated, potentially compromising current clinical outcomes.
This study has some limitations. Native data have been extracted from arthritic knees; it could be argued that the results are not a reflection of undamaged knees. This would occur only after some degree of bone loss due to advanced disease being present; patients in Australia generally present at early stages of OA, and the sample size would probably eliminate this theoretical deviation. Notwithstanding that, these knees are the ones requiring a replacement, and therefore, the comparison of such anatomical features to those of implants in use has been considered adequate. Either way, a previous study on healthy knees revealed a trochlear valgus orientation of 1° ± 5° [14], a result equally distant from the average PTA values. Another limitation was the inability to source PTA details of all implants currently on the market. Dejour et al. already sentenced that manufactures tend to provide scarce details in regard to trochlear parameters [5]. Nonetheless, it appears unlikely to have missed models with significantly different PTAs, as this would probably have been advertised as a genuine feature in the brochures available for all systems. Further, the authors acknowledge that there are other trochlear parameters such as congruity, depth, lateral height, and the patellar component shape itself that can influence balance, tracking, and functional outcome. Finally, the clinical correlation of patellofemoral complications and trochlear mismatch within the studied cohort has not been analyzed. The fact that this cohort encompasses the records of multiple surgeons across Australia, employing varied surgical protocols and implants, has hindered this analysis, which remains as a future objective. As a consequence, the clinical implications of the NTA–PTA incongruity are still to be defined.
Conclusion
Trochlear coronal orientation in arthritic knees and in currently used implants differ relevantly, which may contribute to patellofemoral imbalance and dissatisfaction after TKR surgery. This mismatch may be especially relevant in newer alignment techniques, where femoral components may be implanted in valgus and/or in internal rotation, further increasing the NTA–PTA discrepancy. An increased awareness is recommended, encouraging surgeons to preoperatively identify discrepancies between the native and implanted trochlea.
Data availability statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- TKR:
-
Total knee replacement
- OA:
-
Osteoarthritis
- CT:
-
Computed tomography
- PFJ:
-
Patellofemoral joint
- NSW:
-
New South Wales
- 3D:
-
3 Dimensions
- NTA:
-
Native trochlear angle
- PTA:
-
Prosthetic trochlear angle
References
Australian Orthopedic Association (2022) Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, Knee & Shoulder Arthroplasty: 2022 Annual Report. Adelaide
Barink M, van de Groes S, Verdonschot N, de Waal MM (2006) The difference in trochlear orientation between the natural knee and current prosthetic knee designs; towards a truly physiological prosthetic groove orientation. J Biomech 39:1708–1715
Barink M, van de Groes S, Verdonschot N, de Waal MM (2003) The trochlea is bilinear and oriented medially. Clin Orthop 411:288–295
Blight TJ, Choong PFM (2022) No consistent association between patient-reported outcome measures and coronal alignment following total knee arthroplasty: a narrative review. Aust N Z J Surg. https://doi.org/10.1111/ANS.18050
Dejour D, Ntagiopoulos PG, Saffarini M (2014) Evidence of trochlear dysplasia in femoral component designs. Knee Surg Sports Traumatol Arthrosc 22:2599–2607
Du Z, Chen S, Yan M, Yue B, Wang Y (2017) Differences between native and prosthetic knees in terms of cross-sectional morphology of the femoral trochlea: a study based on three-dimensional models and virtual total knee arthroplasty. BMC Musculoskelet Disord. https://doi.org/10.1186/s12891-017-1529-x
Dubin JA, Muskat A, Westrich GH (2020) Design modifications of the posterior-stabilized knee system may reduce anterior knee pain and complications following total knee replacement. HSS J 16:344
Eckhoff DG, Burke BJ, Dwyer TF, Pring ME, Spitzer VM, VanGerwen DP (1996) The ranawat award. sulcus morphology of the distal femur. Clin Orthop Relat Res 331:23–28
Grassi A, Asmonti I, Bignozzi S, Zaffagnini S, Neri MP, Cionfoli C, Vanderschelden Y (2021) The sagittal geometry of the trochlear groove could be described as a circle: an intraoperative assessment with navigation. Knee Surg Sports Traumatol Arthrosc 29:1769–1776
Hazratwala K, O’Callaghan WB, Dhariwal S, Wilkinson MPR (2022) Wide variation in tibial slopes and trochlear angles in the arthritic knee: a CT evaluation of 4116 pre-operative knees. Knee Surg Sports Traumatol Arthrosc 30:3049–3060
Hochreiter B, Hirschmann MT, Amsler F, Behrend H (2019) Highly variable tibial tubercle-trochlear groove distance (TT-TG) in osteoarthritic knees should be considered when performing TKA. Knee Surg Sports Traumatol Arthrosc 27:1403–1409
Hochreiter B, Moser LB, Hess S, Hirschmann MT, Amsler F, Behrend H (2021) Osteoarthritic knees have a highly variable patellofemoral alignment: a systematic review. Knee Surg Sports Traumatol Arthrosc 29:483–490
Hull ML, Howell SM (2022) Differences in trochlear morphology from native using a femoral component interfaced with an anatomical patellar prosthesis in kinematic alignment and mechanical alignment. J Knee Surg 35:625–633
Iranpour F, Merican AM, Dandachli W, Amis AA, Cobb JP (2010) The geometry of the trochlear groove. Clin Orthop Relat Res 468:782–788
Kahlenberg CA, Nwachukwu BU, McLawhorn AS, Cross MB, Cornell CN, Padgett DE (2018) Patient satisfaction after total knee replacement: a systematic review. HSS J 14:192–201
Koh YG, Nam JH, Chung HS, Lee HY, Kim HJ, Kim HJ, Kang KT (2019) Gender-related morphological differences in sulcus angle and condylar height for the femoral trochlea using magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc 27:3560–3566
Kulkarni SK, Freeman MAR, Poal-Manresa JC, Asencio JI, Rodriguez JJ (2001) The patellofemoral joint in total knee arthroplasty: is the design of the trochlea the critical factor? Knee Surg Sports Traumatol Arthrosc 9:8–12
Li CY, Cheong Chung KJN, Ali OME, Chung NDH, Li CH (2020) Literature review of the causes of pain following total knee replacement surgery: prosthesis, inflammation and arthrofibrosis. EFORT Open Rev 5:534–543
MacDessi SJ, Griffiths-Jones W, Harris IA, Bellemans J, Chen DB (2021) Coronal Plane Alignment of the Knee (CPAK) classification. Bone Joint J 103:329–337
Müller JH, Li K, Reina N, Telmon N, Saffarini M, Cavaignac E (2020) Sexual and ethnic polymorphism result in considerable mismatch between native trochlear geometry and off-the-shelf TKA prostheses. Knee Surg Sports Traumatol Arthrosc 28:3871–3878
Nishitani K, Kuriyama S, Nakamura S, Morita Y, Ito H, Matsuda S (2019) Valgus position of the femoral component causes abnormal kinematics in the presence of medial looseness in total knee arthroplasty: a computer simulation model of TKA for valgus knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc 27:2051–2060
O’Callaghan WB, Gouk C, Wilkinson MPR, Haztratwala K (2022) Computer-aided surgery-navigated, functional alignment total knee arthroplasty: a surgical technique. Arthroplast Today 14:121–127
Olcott CW, Scott RD (2000) Determining proper femoral component rotational alignment during total knee arthroplasty. Am J Knee Surg 13:166–168
Park CN, White PB, Meftah M, Ranawat AS, Ranawat CS (2016) Diagnostic algorithm for residual pain after total knee arthroplasty. Orthopedics 39:e246–e252
Rivière C, Dhaif F, Shah H, Ali A, Auvinet E, Aframian A, Cobb J, Howell S, Harris S (2018) Kinematic alignment of current TKA implants does not restore the native trochlear anatomy. Orthop Traumatol Surg Res 104:983–995
Rivière C, Iranpour F, Harris S, Auvinet E, Aframian A, Parratte S, Cobb J (2018) Differences in trochlear parameters between native and prosthetic kinematically or mechanically aligned knees. Orthop Traumatol Surg Res 104:165–170
Roussot MA, Haddad FS (2019) The evolution of patellofemoral prosthetic design in total knee arthroplasty: how far have we come? EFORT Open Rev 4:503–512
Shah SM (2021) After 25 years of computer-navigated total knee arthroplasty, where do we stand today? Arthroplasty 3:41
Slevin O, Schmid FA, Schiapparelli FF, Rasch H, Amsler F, Hirschmann MT (2017) Coronal femoral TKA position significantly influences in vivo patellar loading in unresurfaced patellae after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:3605–3610
Wakelin EA, Tran L, Twiggs JG, Theodore W, Roe JP, Solomon MI, Fritsch BA, Miles BP (2018) Accurate determination of post-operative 3D component positioning in total knee arthroplasty: the AURORA protocol. J Orthop Surg Res 13:1–10
Wendelspiess S, Kaelin R, Vogel N, Rychen T, Arnold MP (2022) No difference in patient-reported satisfaction after 12 months between customised individually made and off-the-shelf total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 30:2948–2957
Woiczinski M, Kistler M, Schröder C, Braun C, Weber P, Müller PE, Jansson V, Steinbrück A (2019) TKA design-integrated trochlea groove rotation reduces patellofemoral pressure. Knee Surg Sports Traumatol Arthrosc 27:1680–1692
Acknowledgements
The authors of this manuscript want to thank the contribution of Andrea Grant, ORIQL Research Coordinator, Joshua Twiggs, Head of Research and Development at 360 Med Care, and all 360 Knee group: Andrew Shimmin, Bede O'Connor, Brad Miles, Brett Fritsch, David Dickison, David Liu, David Parker, Jonathan Barre, Justin Roe, Michael Solomon, Richard Boyle, and Stephen McMahon.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. No institutional or commercial funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
SB: research idea, data collection and analysis, bibliographic review, and manuscript preparation. KH: bibliographic review and manuscript preparation. MW: data collection and manuscript revision.
Corresponding author
Ethics declarations
Conflict of interest
ORIQL members of the research team have no financial association with 360 Knee Systems Pty Ltd. No other potential conflicts of interest are declared.
Ethical approval
Bellberry Human Research Ethics Committee, Approval Number 2012-03-710.
Informed consent
All participants in the study received and signed an informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rosa, S.B., Hazratwala, K. & Wilkinson, M.P.R. Mismatch between trochlear coronal alignment of arthritic knees and currently available prosthesis: a morphological analysis of 4116 knees and 45 implant designs. Knee Surg Sports Traumatol Arthrosc 31, 3116–3123 (2023). https://doi.org/10.1007/s00167-022-07251-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07251-5